General anesthesia keeps patients asleep and pain-free during surgery. It uses medicines to make the patient sleep, ensuring they stay calm and comfortable during the operation. Many people wonder, do you have to be intubated for general anesthesia? In most cases, intubation is done to help patients breathe safely while they are under anesthesia.
At Liv Hospital, many patients wonder about general anesthesia and intubation. Intubation is often used to keep the airway safe during surgery. But, it’s not always needed. Knowing more about anesthesia and airway management can make patients feel more prepared and calm before their surgery.
Key Takeaways
- General anesthesia induces a sleep-like state using a combination of medicines.
- Intubation is often performed to ensure a secure airway during surgery.
- Not all surgeries requiring general anesthesia necessitate intubation.
- Liv Hospital prioritizes patient-centered care and transparency regarding medical procedures.
- Understanding anesthesia and airway management can alleviate patient concerns.
Understanding General Anesthesia

General anesthesia is a complex medical process. It makes patients unconscious and pain-free during surgery. It uses different anesthetic agents to keep patients safe and comfortable.
Definition and Purpose
General anesthesia is a deep sedation that prevents movement and memory loss. It’s used to keep patients pain-free and relaxed during surgery.
Components
General anesthesia mixes different anesthetic agents. These include hypnotics, analgesics, and neuromuscular blockers. They work together to make patients unconscious, pain-free, and ready for surgery.
The main parts are:
- Hypnotics: Agents like propofol that make patients sleep.
- Analgesics: Medications such as opioids that block pain.
- Neuromuscular blockers: Drugs that relax muscles and help with intubation.
Effects on the Body
General anesthesia makes the body unconscious and pain-free. It also relaxes muscles. It affects the central nervous, cardiovascular, and respiratory systems.
| Bodily System | Effects of General Anesthesia |
| Central Nervous System | Induced unconsciousness and amnesia |
| Cardiovascular System | Potential changes in blood pressure and heart rate |
| Respiratory System | Controlled ventilation and possible respiratory depression |
What Is Intubation and Why Is It Used?

Intubation is a key medical procedure used during general anesthesia. It ensures a patient’s airway is secure. A breathing tube, called an endotracheal tube, is placed in the trachea. This is vital for safe breathing during surgery.
Definition of Endotracheal Intubation
Endotracheal intubation means putting a tube through the mouth or nose into the lungs. This tube helps provide a safe airway. It allows oxygen and anesthetic gases to reach the lungs directly.
A laryngoscope is used to guide the tube into the correct spot. This tool helps place the tube accurately.
The Process of Intubation
The intubation process starts with anesthesia to relax the patient. A laryngoscope is then used to see the vocal cords. It guides the endotracheal tube into the trachea.
After the tube is in place, it’s secured with tape or a device. This keeps it from moving during surgery.
Primary Functions of Intubation During Surgery
The main roles of intubation during surgery are to ensure a secure airway. It also helps with ventilation and protects the lungs from harmful substances. By keeping the airway secure, it allows anesthesiologists to manage the patient’s breathing.
Intubation is also key in preventing lung damage. It stops stomach contents from entering the lungs. This is critical during surgery to avoid respiratory problems. Intubation is essential for effective anesthesia care, ensuring the patient’s airway is managed well during surgery.
Do You Have to Be Intubated for General Anesthesia?
Intubation is common in surgeries under general anesthesia. But, it’s not always needed. The choice to intubate depends on the surgery and the patient’s health.
When Intubation Is Necessary
Intubation is needed for surgeries needing full control over the airway and breathing. This is true for longer surgeries or those in the chest or abdomen.
Surgeries That Typically Require Intubation
Some surgeries always need intubation, like:
- Cardiothoracic surgeries
- Neurosurgeries
- Major abdominal surgeries
These surgeries need precise airway control for safe anesthesia.
Procedures Where Intubation May Not Be Required
Some procedures might not need intubation, such as:
- Minor surgeries with short durations
- Certain endoscopic procedures
- Surgeries where a laryngeal mask airway (LMA) is enough
In these cases, other airway management methods can be used.
Factors That Determine the Need for Intubation
Several factors decide if intubation is needed, including:
| Factor | Description |
| Surgery Type | The surgery’s nature and complexity |
| Surgery Duration | Long surgeries often need intubation |
| Patient’s Health | The patient’s health can influence the decision |
Deciding on intubation for general anesthesia varies. It depends on the surgery and the patient’s health.
Alternative Airway Management Techniques
Intubation isn’t the only way to manage airways during general anesthesia. Other methods are used based on the surgery type, patient’s health, and the anesthesiologist’s choice.
Laryngeal Mask Airways (LMAs)
Laryngeal Mask Airways (LMAs) are placed over the larynx to seal it. This allows for breathing without endotracheal intubation. LMAs are less invasive and suitable for surgeries where intubation isn’t needed.
Face Mask Ventilation
Face mask ventilation is used to manage airways during general anesthesia. A mask is placed over the patient’s nose and mouth. It delivers oxygen and anesthetic gases. This method is used for short procedures or with other techniques.
Supraglottic Airway Devices
Supraglottic airway devices are like LMAs but used without intubation. They sit above the glottis for ventilation. They are useful for procedures that don’t need muscle paralysis.
When Alternatives Are Preferred Over Intubation
The choice between intubation and alternatives depends on several factors. These include the surgery type, its duration, the patient’s medical history, and the anesthesiologist’s judgment. Alternatives are often chosen for less invasive procedures or when intubation risks are high.
| Airway Management Technique | Description | Typical Use Cases |
| Laryngeal Mask Airways (LMAs) | Device placed over the larynx for ventilation | Surgeries not requiring intubation |
| Face Mask Ventilation | Mask placed over nose and mouth for oxygen delivery | Short procedures, combined with other techniques |
| Supraglottic Airway Devices | Devices sitting above the glottis for ventilation | Procedures not requiring muscle paralysis |
Risks and Complications of Intubation
Intubation is a lifesaving procedure, but it comes with risks. It’s important for patients to know these risks before undergoing general anesthesia. This procedure secures a patient’s airway during surgery and can lead to serious complications.
Common Complications
Patients may face sore throat, difficulty swallowing, and vocal cord damage after intubation. These issues are usually temporary but can be uncomfortable. In some cases, more severe problems like esophageal intubation or tracheal trauma can happen.
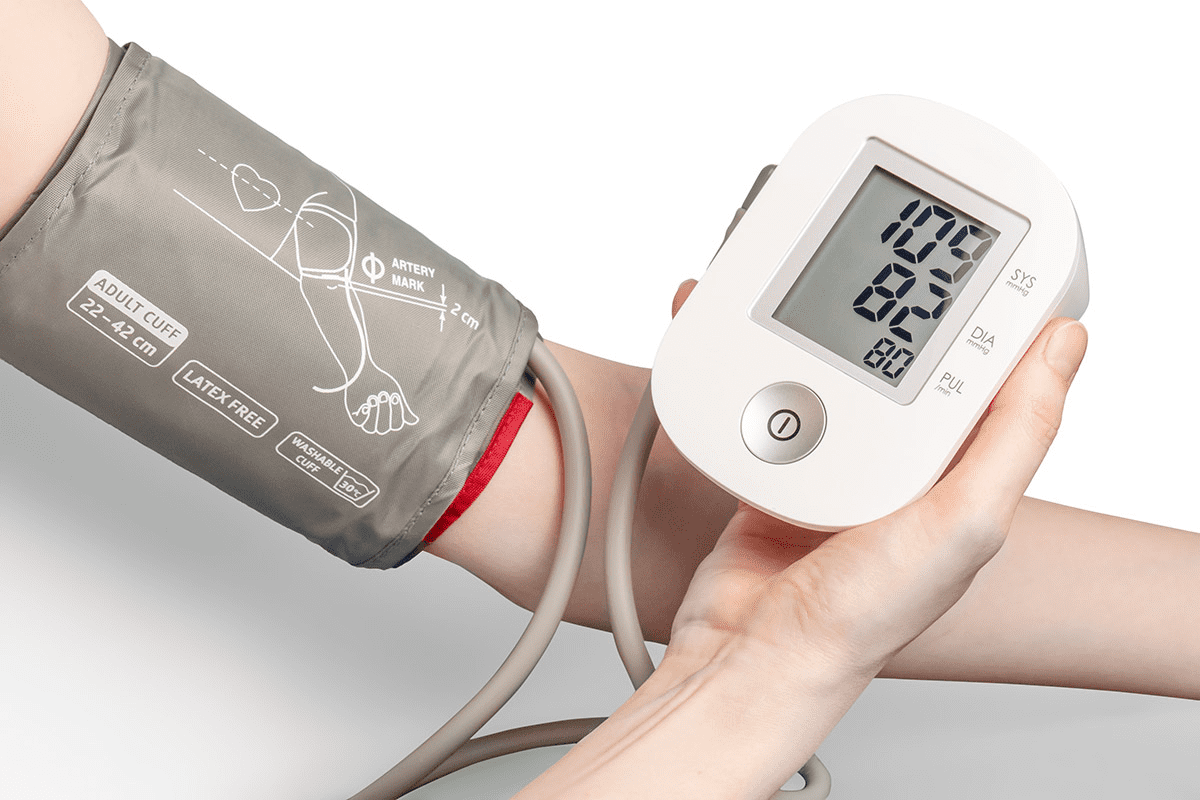
Cardiovascular Risks
Intubation can also affect the heart and blood pressure. The stress of inserting the endotracheal tube can cause heart rate and blood pressure changes. Patients with heart conditions need close monitoring during the procedure.
Post-Intubation Symptoms
After intubation, patients may have a sore throat, hoarseness, and trouble speaking. These symptoms are usually short-term but can be painful. In some cases, patients may face more severe symptoms like breathing trouble or chest pain, which need immediate medical help.
Statistical Overview of Intubation Risks
Recent studies show the risks of intubation. Up to 45% of critically ill patients face complications after intubation. Knowing these risks helps healthcare providers and patients make better decisions about airway management.
Being aware of intubation risks helps patients prepare for the procedure. They can discuss their concerns with their healthcare provider.
Patient Factors That Influence Airway Management Decisions
The anesthesia team looks at many patient factors to choose the best airway management. These factors help decide if intubation or another method is best during general anesthesia.
Medical History Considerations
A patient’s medical history is key in airway management decisions. Conditions like diabetes, hypertension, and heart disease can change anesthesia choices. The team checks the patient’s health history, including past surgeries, allergies, and current meds.
Anatomical Factors
Anatomical factors like the airway, neck, and jaw structure can affect intubation ease. Patients with certain features might need different airway management techniques.
Previous Anesthesia Experiences
A patient’s previous experiences with anesthesia can shape current airway management choices. Knowing about any past complications or reactions is vital for the team.
Risk Assessment Process
The risk assessment process evaluates the patient’s health, the surgery’s complexity, and other factors. This tailored approach aims to minimize risks and ensure a safe anesthesia experience.
Modern Protocols and Advancements in Airway Management
Advances in airway management have greatly improved patient care. This is thanks to modern protocols and evidence-based practices. Liv Hospital is dedicated to using the latest, top-notch protocols. These focus on keeping patients safe and comfortable.
Evidence-Based Practices
New research in anesthesiology has led to evidence-based practices in airway management. These practices are always updated with the newest research. This ensures patients get the best care possible.
Technological Innovations
Technological innovations have been key in improving airway management. New ventilation methods and advanced monitoring systems have made airway care safer and more effective.
Internationally Competitive Standards
Liv Hospital follows internationally competitive standards in airway management. This means patients get care that meets global best practices. The hospital’s commitment to excellence shows in its protocols and practices.
Quality and Safety Measures
Putting quality and safety measures first is essential in airway management. Liv Hospital’s protocols aim to reduce risks and provide top-notch care. The hospital constantly monitors and improves its practices.
What to Expect Before and After Intubation
Getting ready for intubation means following a few key steps. Knowing what happens before, during, and after can make things less scary. It can also help improve how well you do.
Preparation for Intubation
Before the procedure, you’ll get instructions on when to stop eating and drinking. This is to make sure your stomach is empty. It’s very important to follow these instructions to avoid problems.
You might also need to take off jewelry, contact lenses, or dentures before going to the operating room. Anesthesia experts will also look over your medical history. They’ll check for any risks or special needs for intubation.
The Patient Experience
During intubation, you’ll be under general anesthesia. You won’t feel the procedure. A breathing tube is put through your mouth or nose into your lungs. This makes sure you get enough oxygen during surgery.
Anesthesia professionals will watch you closely during the procedure. They make sure you’re safe and comfortable. The whole process is usually quick, and you won’t remember it.
Recovery from Intubation
Once the surgery is over, the tube is taken out, and you go to the recovery room. Recovery might feel a bit uncomfortable, like a sore throat or trouble swallowing.
These feelings usually go away on their own or with some help from medicine or throat lozenges. You’ll also be watched for any signs of trouble, like breathing problems or a lot of pain.
Managing Post-Intubation Discomfort
To deal with discomfort after intubation, you might get pain medicine or other treatments. Drinking plenty of water and resting your voice can also help with throat soreness.
It’s very important to follow the instructions from your healthcare team to recover well. If you’re feeling really bad or symptoms don’t go away, reach out to your healthcare provider for help.
Conclusion: Making Informed Decisions About Your Anesthesia Care
It’s important for patients to understand the link between general anesthesia and intubation. Knowing when intubation is needed and what alternatives exist helps patients navigate their surgery better.
Patients should talk to their healthcare providers about their medical history and any past anesthesia experiences. This way, they can find the best airway management for them. This approach helps patients get care that fits their unique needs.
Deciding on anesthesia care means weighing the risks and benefits of intubation and other airway methods. With this knowledge, patients can feel more ready for their surgery.
Being informed lets patients take a bigger role in their care. This leads to a smoother and more successful surgery. By talking openly with their healthcare providers, patients can make choices that match their needs and wishes.
FAQ
Do you have to be intubated with general anesthesia?
No, you don’t always need to be intubated with general anesthesia. But, it’s often done to make sure your airway is safe during surgery.
Are you always intubated during surgery?
No, not every surgery needs intubation. Whether or not you need it depends on your surgery, health history, and other factors.
What is the difference between general anesthesia and intubation?
General anesthesia makes you unconscious with drugs. Intubation is when a tube is put into your trachea to secure your airway.
Can you have general anesthesia without intubation?
Yes, you can have general anesthesia without a tube. Sometimes, doctors use other methods like laryngeal mask airways or face mask ventilation.
What are the risks associated with intubation?
Intubation can have risks, like common problems and heart risks. But, these risks are low if done by skilled healthcare professionals.
How do patient factors influence airway management decisions?
Your medical history, body shape, and past anesthesia experiences help decide how to manage your airway.
What can I expect before and after intubation?
Before, you’ll get meds and monitoring. After, you’ll be watched closely and any discomfort will be managed.
Are there alternative airway management techniques?
Yes, there are other ways to manage your airway, like laryngeal mask airways, face mask ventilation, and supraglottic airway devices.
Does general anesthesia require intubation?
Not always. Intubation is common with general anesthesia, but it depends on your surgery and health.
What are the modern protocols and advancements in airway management?
Today, we use evidence-based practices and new technologies. We focus on quality and safety to get the best results.
References
- Andrews, S., et al. (2013). Gallstone size e related to the incidence of post-cholecystectomy retained bile duct stones. Surgery Journal, 5(3), 143-147. Retrieved from https://www.sciencedirect.com/science/article/pii/S1743919113000484