Many adults worry and often ask, “does leukemia come back” after they’ve been in remission. Acute Myeloid Leukemia (AML) is a type of leukemia that can return even after successful treatment. It’s important for patients and doctors to understand AML recurrence and how long remission usually lasts.
AML treatment includes remission induction, consolidation, and sometimes maintenance therapy. The treatment plan depends on several factors, including the patient’s age, health, and genetic mutations. At Liv Hospital, we create personalized treatment plans to meet each patient’s unique needs and improve long-term outcomes.
Key Takeaways
- AML can relapse after remission, with high rates in adults.
- Understanding AML recurrence and remission duration is key for patients and doctors.
- Treatment for AML includes remission induction, consolidation, and sometimes maintenance therapy.
- The treatment choice depends on age, health, and genetic mutations.
- Liv Hospital provides personalized treatment plans for AML patients.
Understanding Leukemia and AML Recurrence
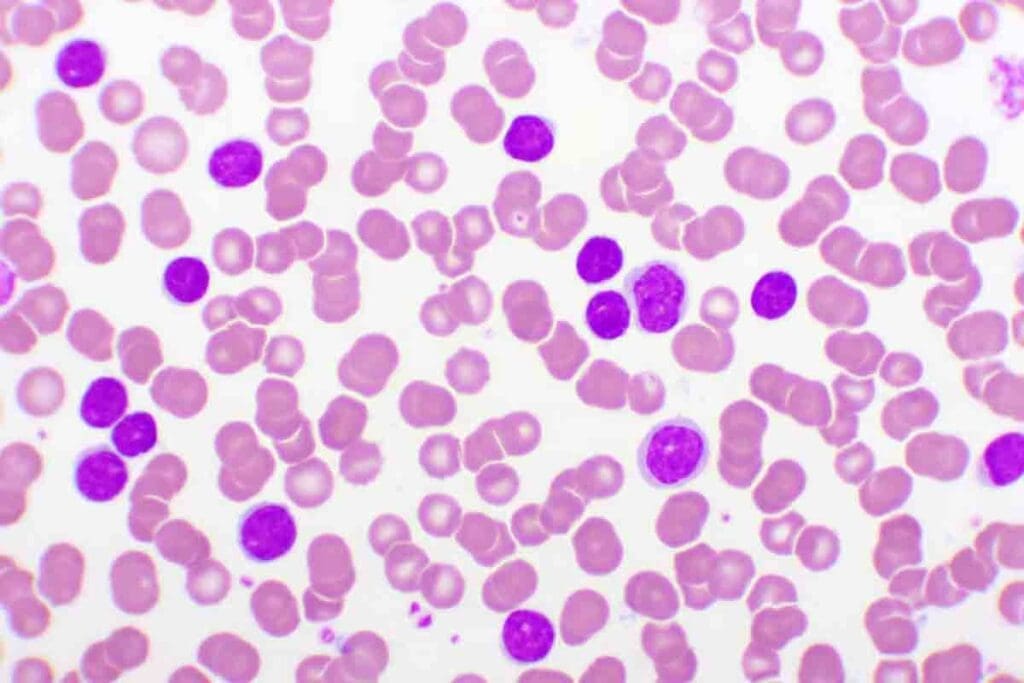
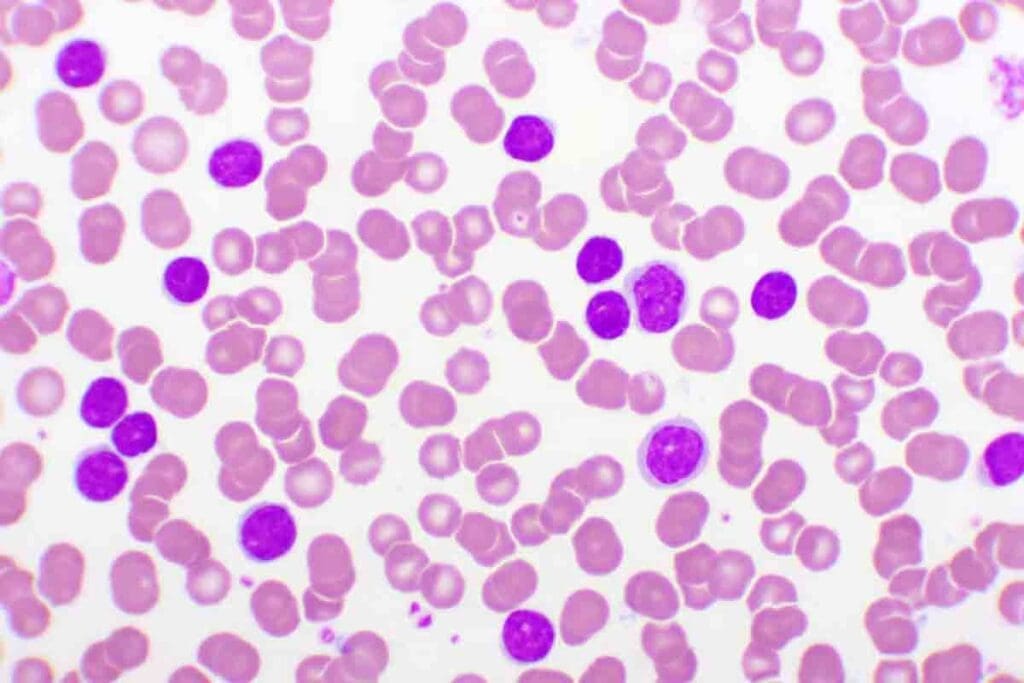
To understand how often leukemia comes back, we need to know about Acute Myeloid Leukemia (AML) and its effects on the body. AML is a cancer that starts in the bone marrow and quickly spreads to the blood. It can also reach other parts of the body, like the lymph nodes, liver, spleen, and more.
What is Acute Myeloid Leukemia (AML)?
Acute Myeloid Leukemia (AML) is a fast-growing cancer that affects the bone marrow. It stops the normal production of blood cells. This leads to health problems.
The symptoms of AML include fatigue, fever, infections, and easy bleeding or bruising. It’s important to know that AML has different types, based on the leukemia cells’ genetic makeup.
The Concept of Remission in Leukemia
Remission in leukemia means the disease is controlled, and no leukemia cells are found in the blood or bone marrow. Remission induction is the first step in treatment, aiming to clear the body of leukemia cells. Reaching remission is a big achievement in AML treatment.
But, remission doesn’t mean the disease is cured. It shows the treatment has worked well enough to hide the leukemia.
Differences Between Remission and Cure
It’s important to know the difference between remission and cure. Remission is a state where the disease is not detectable, achieved through treatment. A cure means the disease won’t come back.
In AML, getting a cure is hard because of the risk of recurrence. The chance of relapse depends on the leukemia’s genetics, how well it responds to treatment, and if there’s any leftover disease.
Does Leukemia Come Back After Treatment?
Leukemia can come back after treatment, which worries many patients. The chance of it happening depends on the leukemia type and how well the first treatment worked.
Recurrence Rates in Different Types of Leukemia
Leukemia types have different chances of coming back. For example, Acute Myeloid Leukemia (AML) has a higher chance of recurrence. Studies show that up to two-thirds of AML patients may see it return.
- AML recurrence rates are significant, with most relapses occurring within the first 18 months after treatment.
- Chronic Lymphocytic Leukemia (CLL) tends to have a lower recurrence rate compared to AML, but it can also come back after treatment.
- The recurrence rate for Acute Lymphoblastic Leukemia (ALL) varies, with some studies indicating a higher relapse rate in adults compared to children.
Why Relapses Occur in Leukemia Patients
Leukemia relapses can happen for several reasons, including:
- Genetic mutations: Some genetic mutations can make leukemia cells resistant to treatment, leading to recurrence.
- Inadequate initial treatment response: Patients who don’t respond well to the first treatment are more likely to relapse.
- Minimal Residual Disease (MRD): MRD after treatment can signal a higher risk of recurrence.
A study found that “The presence of MRD is a strong predictor of relapse in patients with AML” (
Source: Journal of Clinical Oncology
).
Timeframe for Most Common Recurrences
Most leukemia recurrences happen within the first year after treatment. A big number occur in the first 6-18 months. It’s important to keep up with regular check-ups during this time to catch any recurrence early.
Early detection of recurrence can significantly impact treatment outcomes and patient survival.
Typical AML Remission Duration
Patients with Acute Myeloid Leukemia (AML) often wonder how long they will stay in remission. The time in remission can vary a lot from person to person. This depends on several factors.
The average length of the first remission is important for both patients and doctors. Generally, the first remission can last from 6 to 18 months. But, this time can change based on different factors.
Average Length of First Remission
Studies show that the average first remission for AML patients is between 6 to 18 months. This time is key as it shows how well the treatment worked.
Factors That Influence Remission Duration
Many things can affect how long a patient stays in remission. These include:
- Age: Older adults might have shorter remissions because of weaker bodies and health issues.
- Genetic Mutations: Some genetic changes can make relapse more likely and shorten remission.
- Response to Initial Treatment: Patients who do well with the first treatment tend to stay in remission longer.
- Minimal Residual Disease (MRD): MRD means a higher risk of relapse.
The table below shows the main factors that affect AML remission duration:
| Factor | Impact on Remission Duration |
| Age | Older age may result in shorter remission |
| Genetic Mutations | Certain mutations can increase relapse risk |
| Initial Treatment Response | Positive response correlates with longer remission |
| Minimal Residual Disease (MRD) | Presence of MRD may shorten remission duration |
Knowing these factors helps patients and doctors make better treatment plans and follow-up care.
AML Relapse Statistics and Timeframes
The chance of AML relapse changes over time. There are clear patterns in the years after diagnosis. Knowing these patterns helps patients and doctors make better treatment choices.
First-Year Relapse Rates
The first year is very important. About 40% of patients have a relapse then. This shows why it’s key to watch patients closely during this time.
Second-Year Recurrence Patterns
In the second year, the relapse rate goes down to 17%. While it’s lower than the first year, it’s not safe to let your guard down.
Third-Year and Beyond Recurrence
By the third year, the rate drops to 2%. This trend keeps going, showing a lower risk of relapse for those in remission.
Long-Term Remission Beyond Five Years
| Year After Diagnosis | Relapse Rate |
| 1st Year | 40% |
| 2nd Year | 17% |
| 3rd Year and Beyond | 2% |
The table shows the risk of AML relapse goes down over time. This info is key for managing patient hopes and planning follow-up care.
“The risk of relapse is a significant concern for AML patients, making it essential to understand the statistics and timeframes associated with recurrence.”
Expert Opinion
By looking at AML relapse stats and understanding when it happens, doctors can make better treatment plans. This helps improve patient outcomes.
Risk Factors for AML Recurrence
Several key factors can increase the likelihood of AML recurrence, affecting patient outcomes significantly. Understanding these risk factors is essential for developing effective treatment plans and improving patient prognosis.
Age-Related Risk Factors in Adults
Age is a significant risk factor for AML recurrence. Older adults tend to have a higher risk of relapse due to decreased physical reserves, comorbidities, and less aggressive treatment approaches often necessitated by age-related health issues.
Older patients are more likely to experience a relapse, partly because their leukemia cells may be more resistant to treatment. As noted by experts, “The older the patient, the more likely they are to have adverse genetic factors and less likely to tolerate intensive chemotherapy.”
Genetic and Cytogenetic Influences
Genetic mutations play a critical role in AML recurrence. Certain cytogenetic abnormalities, such as those involving chromosomes 5 or 7, are associated with a higher risk of relapse.
- Adverse cytogenetics: Patients with adverse cytogenetic profiles tend to have poorer outcomes and higher relapse rates.
- Genetic mutations: Specific mutations, such as FLT3-ITD, can significantly impact the risk of recurrence.
Impact of Initial Treatment Response
The initial response to treatment is a critical predictor of AML recurrence. Patients who achieve complete remission after the first cycle of chemotherapy generally have a better prognosis than those who require multiple cycles.
A swift and complete response to initial treatment is often associated with a lower risk of relapse. On the other hand, a slow or incomplete response can indicate a higher risk of recurrence.
Minimal Residual Disease (MRD)
Minimal Residual Disease (MRD) refers to the presence of leukemia cells that remain detectable after treatment, even when the patient is in complete remission. MRD is a powerful predictor of AML recurrence.
“The presence of MRD after treatment is a strong indicator of possible relapse, highlighting the need for continued monitoring and potentially more aggressive treatment strategies.”
Monitoring MRD levels can help healthcare providers identify patients at higher risk of relapse, allowing for timely intervention.
Bone Marrow and Stem Cell Transplant Outcomes
For many AML patients, bone marrow and stem cell transplants are a key chance at long-term remission. These procedures replace the patient’s diseased bone marrow with healthy stem cells. This can be from the patient themselves (autologous transplant) or from a donor (allogeneic transplant).
Relapse Rates After Transplantation
Relapse is a big worry after these transplants. The risk of relapse depends on several things. These include the type of transplant, the patient’s condition at transplant, and the presence of minimal residual disease (MRD).
Understanding relapse rates after transplantation is key to knowing patient outcomes. Here’s a summary of recent studies:
| Transplant Type | Relapse Rate | Survival Rate at 2 Years |
| Allogeneic Transplant | 20-40% | 50-60% |
| Autologous Transplant | 40-60% | 40-50% |
Factors Affecting Post-Transplant Recurrence
Many factors can affect AML recurrence after transplant. These include the patient’s age, the leukemia’s cytogenetic risk profile, and MRD presence. Knowing these factors helps manage patient expectations and guide care after transplant.
Survival Rates Following Transplant Relapse
The outlook for patients with transplant relapse is generally poor. But, survival rates can vary. This depends on when the relapse happens and the patient’s health. Some may get additional treatments, like salvage chemotherapy or a second transplant.
Innovative Approaches to Prevent Post-Transplant Relapse
Researchers are looking into new ways to lower relapse risk. They’re exploring targeted therapies to get rid of MRD, immunotherapies to boost the graft-versus-leukemia effect, and new conditioning regimens to improve transplant success.
By improving our understanding of transplant outcomes, we can better support AML patients. This helps in their treatment journey and aims to increase long-term survival rates.
Monitoring and Detecting AML Relapse
It’s key for patients in remission to watch for any signs of AML coming back. This means regular check-ups, tests, and learning about early warning signs.
Follow-up Protocols After Remission
After remission, follow-up plans include blood tests and bone marrow biopsies. These are based on the patient’s risk and medical history. Sticking to these plans is important for catching relapse early.
How often you need to visit the doctor may lessen if you’re doing well. But, it depends on your situation and what your doctor says.
Early Warning Signs of Recurrence
Know the signs of AML coming back, like feeling very tired, losing weight, getting sick a lot, and bleeding easily. Telling your doctor about these symptoms right away is key.
Spotting these signs early can lead to better treatment and outcomes.
Modern Detection Methods
Today, we have better ways to find AML relapse, like molecular tests and flow cytometry. These help spot tiny amounts of cancer cells, which is vital for catching relapse early.
Thanks to these advanced methods, we can keep a closer eye on AML relapse and adjust treatments as needed.
Treatment Options for Relapsed AML
Treatment for relapsed AML involves many strategies. The right treatment depends on the patient’s age, health, and past treatments.
Second-Line Chemotherapy Regimens
For those with relapsed AML, second-line chemotherapy is often used. These treatments aim for a second remission. Success rates depend on how long the first remission lasted and the patient’s health.
- High-dose cytarabine: A common chemotherapy agent used in various regimens.
- Fludarabine and idarubicin: Combination therapies that may be employed.
- Cladribine: Another agent that can be used in combination with other drugs.
Targeted Therapies for Refractory Cases
Targeted therapies are a promising option for refractory AML. They focus on specific molecular targets, which can reduce harm to normal cells.
Examples include:
- FLT3 inhibitors: For patients with FLT3 mutations.
- IDH1 and IDH2 inhibitors: Targeting specific metabolic mutations.
Salvage Transplantation Approaches
Salvage transplantation, like allogenic stem cell transplantation, is a potentially curative option. The decision to go for transplantation depends on the patient’s health and donor availability.
Clinical Trials for Relapsed Patients
Clinical trials offer innovative treatments not available elsewhere. They are key to improving relapsed AML treatment.
Patients should talk to their healthcare providers about the benefits and risks of clinical trials.
Medical Protocols and Institutional Approaches
Managing Acute Myeloid Leukemia (AML) relapse needs strict medical protocols and institutional approaches. Places like Liv Hospital lead in AML treatment. They use the latest methods to help patients.
Liv Hospital’s Diagnostic and Treatment Protocols
Liv Hospital takes a detailed approach to AML diagnosis and treatment. They focus on personalized care. Studies show that certain treatments can lower relapse rates.
Liv Hospital’s methods aim for the best care. They use the newest AML treatments.
“A team effort is key in AML management,” says a top expert. This is seen in Liv Hospital’s care plans. They are made for each patient’s needs.
International Guidelines for AML Relapse Management
Liv Hospital follows international guidelines for AML relapse. This ensures patients get the best care. The guidelines stress the need for quick action and new treatments.
- Regular monitoring for signs of relapse
- Use of targeted therapies for refractory cases
- Consideration of salvage transplantation approaches
Multidisciplinary Team Approach
A multidisciplinary team approach is key at Liv Hospital. It brings together many healthcare experts. They work together to create treatment plans for each patient.
By using medical protocols and institutional approaches, Liv Hospital offers full care for AML relapse. This helps patients get better and recover well.
Conclusion: Living with the Possibility of AML Recurrence
Knowing the risk of AML coming back is key for both patients and doctors. AML recurrence is a big worry, but understanding the risks helps manage it. This includes watching for signs and having good treatment plans.
Dealing with AML means a team effort. It includes regular check-ups, early warning signs, and new treatments. Patients can handle their disease better by knowing the risks. This way, they can make smart choices about their health.
Handling AML recurrence well needs a team of experts. Places like Liv Hospital lead the way with the latest treatments. This helps patients live better and longer.
Patients can improve their chances of beating AML by staying informed and active. As science moves forward, there’s hope for better managing AML recurrence. This brings new hope to those fighting this tough disease.
FAQ
What is the typical duration of AML remission?
AML remission can last from 6 to 18 months on average. But, it depends on age, genetics, and how well the treatment works.
How often does leukemia come back in adults?
Leukemia can come back, but it depends on the type and the person. For AML, about 40% relapse in the first year, then it drops to 17% in the second year and 2% in the third.
Can leukemia come back after a bone marrow transplant?
Yes, leukemia can come back after a transplant. The chance of it happening depends on the patient’s health, if there’s any cancer left, and the type of transplant.
What are the risk factors for AML recurrence?
AML can come back due to age, genetics, how well the first treatment worked, and if there’s cancer left behind.
How is AML relapse detected?
Doctors check for AML relapse with blood tests, bone marrow biopsies, and other tests. Early signs include feeling tired, losing weight, or getting infections often.
What treatment options are available for relapsed AML?
For AML that comes back, treatments include second-line chemotherapy, targeted therapies, transplant options, and clinical trials.
How long does AML remission last after treatment?
How long AML remission lasts depends on the treatment’s success and if there’s cancer left behind.
What is the role of minimal residual disease in AML recurrence?
Minimal residual disease (MRD) means small cancer cells are left after treatment. It’s a big risk factor for AML coming back.
Can AML relapse be prevented?
AML relapse can’t be completely stopped, but new treatments like targeted therapies and immunotherapies can lower the risk. Regular check-ups are key to catching and managing relapse early.
What is the significance of long-term remission in AML patients?
AML patients who stay in remission for over five years have a lower chance of it coming back. But, they should keep getting checked and cared for to stay healthy.
References
- Cancer.Net Editorial Board. (2023, June 16). Leukemia – Acute Myeloid (AML): Diagnosis. Cancer.Net. American Society of Clinical Oncology (ASCO) via Cancer.Net: https://www.cancer.net/cancer-types/leukemia-acute-myeloid-aml/diagnosis





