Last Updated on November 20, 2025 by Ugurkan Demir

Sickle cell disease (SCD) is a genetic disorder that affects how the body makes hemoglobin. This can lead to serious health problems and even death if not treated properly. Find out: does sickle cell kill you? Understand the serious risks, fatality factors, and prevention strategies for mortality.
In the U.S., about 100,000 people, mostly African Americans, have SCD. It’s a serious condition that needs to be understood to prevent its risks. Worldwide, SCD led to around 34,400 deaths in 2021.
It’s important to know the dangers of SCD. This knowledge helps in managing and preventing the disease effectively.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- SCD can lead to significant morbidity and mortality if not properly managed.
- Approximately 100,000 people in the U.S. are affected by SCD.
- Globally, SCD caused about 34,400 deaths in 2021.
- Understanding SCD risks and prevention strategies is key.
What Is Sickle Cell Disease?

Sickle Cell Disease (SCD) is a group of disorders that affect hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. It’s important for the body’s oxygen supply.
The Genetics Behind Sickle Cell Disease
Sickle Cell Disease is caused by a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation leads to abnormal hemoglobin S (HbS).
This abnormal hemoglobin can change red blood cells into sickle-shaped, rigid cells. The genetic mutation is inherited in an autosomal recessive pattern. This means a person needs two defective HBB genes, one from each parent, to have the disease.
Carriers have one normal and one defective gene. They usually don’t show the disease’s full symptoms. But they can pass the mutated gene to their children.
How Sickle Cell Affects Red Blood Cells
In SCD, the abnormal hemoglobin S makes red blood cells sickle-shaped and less flexible. Normally, these cells are flexible and move easily. But sickled cells can get stuck in small blood vessels.
This can cause pain crises, infections, and organ damage. The sickling also leads to the early destruction of red blood cells. This results in anemia.
Anemia means not enough healthy red blood cells to carry oxygen. People with SCD often feel tired and weak.
Understanding SCD’s genetics and its effects on red blood cells is key. It helps us understand the disease better and find ways to manage it.
Does Sickle Cell Kill You? Understanding Mortality Rates

The death rates linked to SCD are key to grasping the disease’s severity. Sickle Cell Disease is a genetic disorder that affects how red blood cells make hemoglobin. This leads to various health issues.
Global Statistics on Sickle Cell Fatalities
In 2021, SCD caused about 34,400 deaths worldwide. This adds up to a total of 376,000 deaths. These numbers show how much SCD affects global health.
| Year | Global Deaths | Total Mortality |
| 2021 | 34,400 | 376,000 |
| 2020 | 33,100 | 364,000 |
| 2019 | 32,000 | 352,000 |
Regional differences are key in SCD death rates. Sub-Saharan Africa is hit hard, with higher death rates than other areas.
Regional Differences in Mortality
The impact of SCD varies worldwide. Sub-Saharan Africa, and children under five there, suffer the most.
It’s vital to understand these regional differences for better help. Health policies and programs need to focus on these disparities to reduce SCD deaths.
By looking at global and regional data, we can tackle SCD’s death rates. This helps in reducing its effects.
Who Is at Risk for Sickle Cell Disease?
Sickle Cell Disease is a genetic disorder that affects certain ethnic and geographic groups. Knowing who is at risk is key to early diagnosis and treatment.
Ethnic and Geographic Distribution
Sickle Cell Disease is common among people of African descent. The CDC says it affects about 1 in 365 Africans. It also affects those from the Mediterranean, the Middle East, and South Asia, but less often.
This is because the sickle cell trait helps fight malaria, a big problem in these areas. Malaria was once widespread, so the sickle cell trait became more common to survive.
Inheritance Patterns and Genetic Risk
Sickle Cell Disease is inherited in a specific way. A person needs two bad hemoglobin genes, one from each parent, to have the disease. Carriers have one good and one bad gene and usually don’t show symptoms, but can pass the bad gene to their kids.
The chance of having a child with SCD depends on the parents’ genes. If both parents are carriers, each child has a 25% chance of having SCD, a 50% chance of being a carrier, and a 25% chance of not having the disease or being a carrier. Knowing this is important for planning families.
For people at high risk, like those of African descent, getting genetic tests and counseling is a good idea. These services help people understand their risk and plan their families better. Finding out who is a carrier or has SCD early can lead to better health care.
Children and Sickle Cell Disease: A Vulnerable Population
Children with sickle cell disease face a big challenge. They are more at risk because of their age and growing immune systems.
Why Children Under Five Are at Higher Risk
Young children, under five, are very vulnerable to sickle cell disease. Their bodies are not fully developed, making them more likely to get sick. A study in the Journal of Pediatrics found that these kids are at a higher risk of severe infections.
Increased susceptibility to infections is a big worry for this age group. These infections can cause serious problems like vaso-occlusive crises and acute chest syndrome.A pediatric hematologist says, “Preventive measures and early intervention are key for these young ones.”
Childhood Mortality in Sub-Saharan Africa
Sub-Saharan Africa struggles a lot with sickle cell disease, leading to high child death rates. The area’s healthcare is limited, and infections are common. The World Health Organization reports that in some countries, up to 50% of children with sickle cell disease die before they are five.
Many factors contribute to these high death rates, like limited access to healthcare, poor nutrition, and co-existing infections like malaria. Improving healthcare, increasing access to treatment, and implementing preventive measures are essential to save more children’s lives.
“Sickle cell disease is a major public health issue in sub-Saharan Africa, where it contributes significantly to childhood mortality. Addressing this issue requires a comprehensive approach that includes healthcare system strengthening, community education, and targeted interventions.”
-Global health experts.
Creating care programs with newborn screening, antibiotics, and family education can help a lot. These efforts can improve the lives of children with sickle cell disease, mainly in high-risk areas like sub-Saharan Africa.
Life-Threatening Complications of Sickle Cell Disease
It’s important to know about the complications of SCD to manage and prevent deaths. Sickle Cell Disease can cause serious problems that affect a person’s health in many ways.
Acute Chest Syndrome
Acute Chest Syndrome (ACS) is a big problem for SCD patients. It shows up as a new lung issue on X-rays, often with fever, breathing troubles, or chest pain. ACS can quickly lead to breathing failure, so quick diagnosis and treatment are vital.
The cause of ACS is complex, involving infections, fat clots, and blocked blood vessels. Treatment usually includes antibiotics, pain relief, and sometimes blood transfusions. Quick action is key to saving lives.
Stroke and Neurological Complications
Stroke is a serious problem for SCD patients, more so in children. It happens when blood vessels in the brain get blocked, causing damage. Stroke can cause lasting brain damage, affecting life quality.
“The risk of stroke in children with SCD is significantly higher than in the general pediatric population, highlighting the need for regular monitoring and preventive measures,” as highlighted by specialists.
Other brain problems, like silent strokes, can also occur. These may not show symptoms but can harm brain function. Regular brain scans are advised to catch these risks early.
Organ Damage and Failure
SCD can harm different organs due to blocked blood flow and the breakdown of red blood cells. Organ damage can lead to long-term health problems, like an enlarged heart, heart failure, and lung pressure.
- Splenic sequestration and autosplenectomy can happen from repeated blockages.
- Damage to the kidneys can cause chronic kidney disease and failure.
- The liver can also be affected by sickling.
Severe Infections
People with SCD are more likely to get serious infections, like those from Streptococcus pneumoniae. This is because their spleen often doesn’t work well due to damage.
Preventing infections is key, with vaccines and antibiotics. Quick treatment of infections is also critical to avoid severe problems.
Acute Pain Crises: When Sickle Cell Becomes Dangerous
Acute pain crises, or vaso-occlusive crises, are serious and can be life-threatening. They happen when sickled red blood cells block blood vessels. This causes tissue ischemia and pain.
The frequency and severity of these crises vary among people with sickle cell disease. Some have them often, while others rarely. Knowing the triggers and how to manage them is key to managing the disease.
Understanding Vaso-occlusive Crises
Vaso-occlusive crises happen when sickled red blood cells block blood vessels. This causes severe pain. The pain is often sharp, stabbing, or throbbing. Various factors can trigger these crises, including dehydration, infection, cold weather, and stress.
Common Triggers for Vaso-occlusive Crises:
- Dehydration
- Infections
- Cold temperatures
- Stress
- High altitude
Managing these triggers is important to prevent vaso-occlusive crises. Patients are advised to stay hydrated, avoid extreme temperatures, and manage stress through relaxation techniques.
When to Seek Emergency Care
People with sickle cell disease need to know when to seek emergency care. Severe pain that doesn’t respond to usual treatments, signs of infection, and trouble breathing are signs to seek help.
| Symptom | Action |
| Severe pain not relieved by medication | Seek emergency care |
| Signs of infection (fever, chills) | Seek emergency care |
| Difficulty breathing or chest pain | Seek immediate emergency care |
Quick medical attention is vital to manage the crisis. It helps prevent complications and reduces the risk of long-term damage. It’s also important for patients to have a plan for managing acute pain crises. This includes having emergency contacts and knowing the nearest emergency care facility.
Can You Develop Sickle Cell Later in Life?
To understand if Sickle Cell Disease can appear later in life, we need to look at its genetic roots. Sickle Cell Disease (SCD) is a genetic condition caused by a mutation in the HBB gene. This mutation results in abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
Debunking Myths About Sickle Cell Acquisition
Many believe SCD can be developed later in life, like catching an illness. But SCD is a genetic disorder present from birth. The confusion might come from people not being diagnosed until later. This can happen due to mild symptoms, lack of healthcare access, or misdiagnosis.
It’s important to know SCD isn’t something you can get later in life. It’s inherited in an autosomal recessive pattern. This means you need to inherit two defective HBB genes (one from each parent) to have the disease.
Late Diagnosis vs. Late Development
The difference between late diagnosis and late development is key. While SCD is present from birth, symptoms can vary. Some people may have mild symptoms or no symptoms at all until later in life, leading to a delayed diagnosis.
- Late Diagnosis: Happens when people are diagnosed with SCD later in life, often because they had mild or no symptoms early on.
- Late Development: This doesn’t apply to SCD, as it’s a genetic condition people are born with.
It’s important to understand this difference. While SCD can’t be developed later in life, early diagnosis and treatment can greatly improve life quality for those affected.
Living with Sickle Cell: Treatment Options and Management
Living with sickle cell disease means having a treatment plan that includes medicine, pain control, and prevention. It’s important to manage the disease well. This helps reduce pain and improves life quality.
Medical Treatments and Medications
Medical treatments aim to control symptoms, prevent problems, and enhance life quality. Hydroxyurea is used to lessen pain crises and may lower the risk of other issues. Blood transfusions also play a key role, improving oxygen to tissues and lowering complication risks.
For more info on sickle cell disease treatment, check out trusted health sites.
| Treatment | Purpose | Benefits |
| Hydroxyurea | Reduce frequency of painful crises | Decreases risk of complications, improves quality of life |
| Blood Transfusions | Improve oxygen delivery, reduce risk of complications | Reduces risk of stroke and other complications |
| Gene Therapy | Potential cure by correcting the genetic defect | Offers hope for a cure, reduces the need for ongoing treatment |
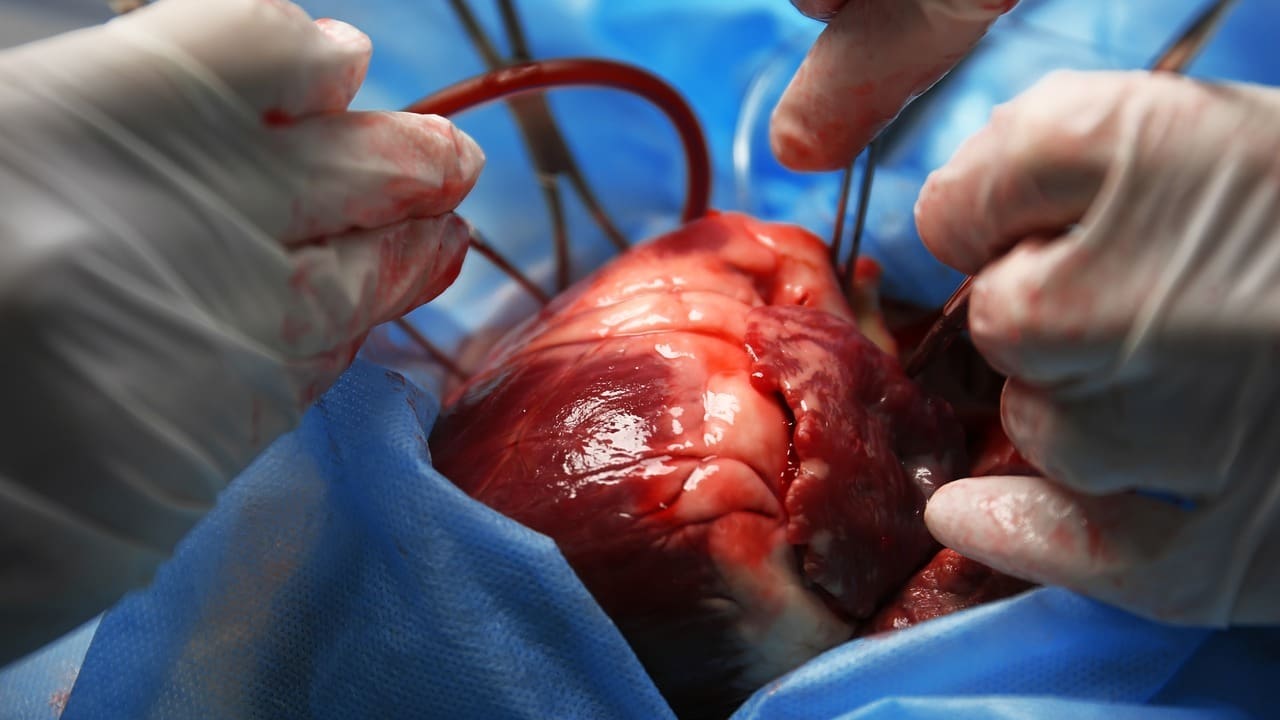
Bone Marrow Transplantation and Gene Therapy
Bone marrow transplantation is the only cure for sickle cell disease. It replaces the patient’s marrow with healthy marrow from a donor. Though it can cure, it’s risky and used for severe cases only.
Gene therapy is a new hope for sickle cell disease treatment. It fixes the genetic defect causing the disease. Early research shows great promise for a cure without a donor.
Managing Pain and Preventing Crises
Managing pain is key for sickle cell disease patients. It involves medicine, lifestyle changes, and prevention to avoid crises. Working with healthcare providers to create a pain plan is essential.
Preventive steps include staying hydrated, avoiding extreme temperatures, and managing stress. By being proactive, people with sickle cell disease can live more active and fulfilling lives.
Conclusion: Understanding the Seriousness of Sickle Cell Disease
Sickle cell disease is a serious genetic disorder that affects millions worldwide. It causes a lot of health problems and can be deadly. It’s important to know about its risks, complications, and treatments to manage it well.
The dangers of SCD are very real. It can cause serious problems like acute chest syndrome, stroke, and damage to organs. Knowing the risks and using the right management strategies can greatly improve life for those with SCD.
By raising awareness about SCD, we can help improve diagnosis, treatment, and care. This includes getting access to medical treatments, managing pain, and preventing complications.
In short, understanding the seriousness of sickle cell disease is key to better patient outcomes. By pushing forward in research and healthcare, we can make a big difference in the lives of those with this condition.
FAQ
What is sickle cell disease?
Sickle cell disease is a serious genetic condition. It affects how red blood cells are made. This causes them to become abnormally shaped.
Can sickle cell disease kill you?
Yes, it can be fatal. This is because of complications like acute chest syndrome and stroke. Organ damage and severe infections are also risks.
Who is at risk for sickle cell disease?
It’s more common in certain ethnic and geographic groups. People with a family history of the disease are also at higher risk.
Can you develop sickle cell anemia later in life?
No, it’s an inherited condition. People are born with it. While diagnosis can happen later, the disease itself doesn’t develop later.
What are the life-threatening complications of sickle cell disease?
Complications include acute chest syndrome and stroke. Organ damage and severe infections are also risks.
How is sickle cell disease managed?
Managing it requires a treatment plan. This includes medical treatments and pain management. Preventive measures against crises are also important.
Is sickle cell disease fatal in children?
Children under five face higher risks. The disease is a significant cause of death in this age group, mainly in sub-Saharan Africa.
What are the symptoms of a vaso-occlusive crisis?
Acute pain crises happen due to vaso-occlusive crises. Knowing when to seek emergency care is key to managing the disease.
Are there new treatments available for sickle cell disease?
Yes, new treatments like gene editing and bone marrow transplantation are promising.
Can sickle cell disease be prevented?
While the disease itself can’t be prevented, understanding risks helps. Taking preventive measures against crises can help manage the disease.
References
- Chang, H., & Tabb, L. (2023). Long-term survival with sickle cell disease: a nationwide cohort. PLoS One / PMC. https://www.ncbi.nlm.nih.gov/articles/PMC10336259
- World Health Organization. (2025). Sickle-cell disease fact sheet.https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease