Uveitis is a serious eye disease that can cause blindness. It happens when the uvea, a key part of the eye, gets inflamed. If not treated quickly, it can lead to vision loss.
Uveitis is a major cause of preventable blindness worldwide. It needs quick action and special treatment. Knowing the risks and how to prevent it is key to keeping your eyes healthy.
Key Takeaways
- Uveitis is a serious inflammatory eye disease that can lead to blindness if not treated.
- Prompt recognition and treatment are critical to prevent vision loss.
- Understanding the risks and complications of uveitis is essential for effective management.
- Prevention methods play a significant role in preserving sight and overall eye health.
- Specialized treatment is necessary to address uveitis and its possible complications.
What is Uveitis? Understanding the Inflammatory Eye Condition
Uveitis is an inflammatory disease that affects the uvea, the middle layer of the eye. It causes inflammation of the uvea and can lead to vision problems if not treated.
The Anatomy of the Uvea and Its Function
The uvea is a key part of the eye, made up of the iris, ciliary body, and choroid. It helps control light entry and keeps the eye healthy. The iris changes the pupil size to control light. The ciliary body makes aqueous humor, which feeds the lens and cornea. The choroid gives blood and oxygen to the retina.
Types of Uveitis Based on Location
Uveitis is divided into types based on where the inflammation is. The main types are:
- Anterior Uveitis: Inflammation at the front, often in the iris.
- Intermediate Uveitis: Inflammation in the middle, affecting the ciliary body.
- Posterior Uveitis: Inflammation at the back, in the choroid.
- Panuveitis: Inflammation in all parts of the uvea.
Each type of uveitis needs a different treatment approach. Knowing the exact type is key to managing it well and saving vision.
Recognizing the Symptoms and Signs of Uveitis
Uveitis symptoms can vary, but there are common signs that mean you need to see a doctor. This condition affects the uvea and can cause vision problems and eye discomfort.
Common Symptoms of Uveitis
Common symptoms include eye pain, redness, sensitivity to light, blurred vision, and floaters. These symptoms can start suddenly or slowly.
- Eye pain is a common complaint, feeling sharp or dull.
- Redness of the eye is due to inflammation.
- Sensitivity to light (photophobia) makes daily tasks hard.
- Blurred vision happens when inflammation affects the eye.
- Floaters are spots in your vision that move with your eyes.
How Long Does Blurred Vision Last with Uveitis?
The time blurred vision lasts with uveitis depends on the type and severity. In some cases, vision clears up once the inflammation is treated. But in severe or chronic cases, blurred vision can last longer.
Several factors affect how long blurred vision lasts:
- The type of uveitis (anterior, intermediate, posterior, or panuveitis).
- The severity of inflammation and any complications.
- The effectiveness of treatment and how well you respond.
Knowing these factors helps manage expectations and guide treatment. We’ll look at treatment options in more detail later.
Does Uveitis Cause Blindness? Examining the Connection
To understand if uveitis can cause blindness, we need to look at how it affects vision. Uveitis is an inflammatory eye condition that hits the uvea, the eye’s middle layer. We’ll dive into how uveitis can lead to vision loss, including stats and its global effects.
Statistics on Uveitis-Related Vision Loss
Uveitis is a big reason for vision problems around the world. It’s behind 10 to 20 percent of blindness in rich countries and up to 25 percent in poor ones. If not treated or treated late, it can cause long-term vision loss. These numbers show the extent of the issue.
Global Impact: Developed vs. Developing Countries
The effect of uveitis on vision loss differs between rich and poor countries. In rich countries, quick medical care can lessen vision loss. But, poor countries struggle with limited healthcare, leading to more blindness from uveitis. Knowing these differences helps us create better health plans.
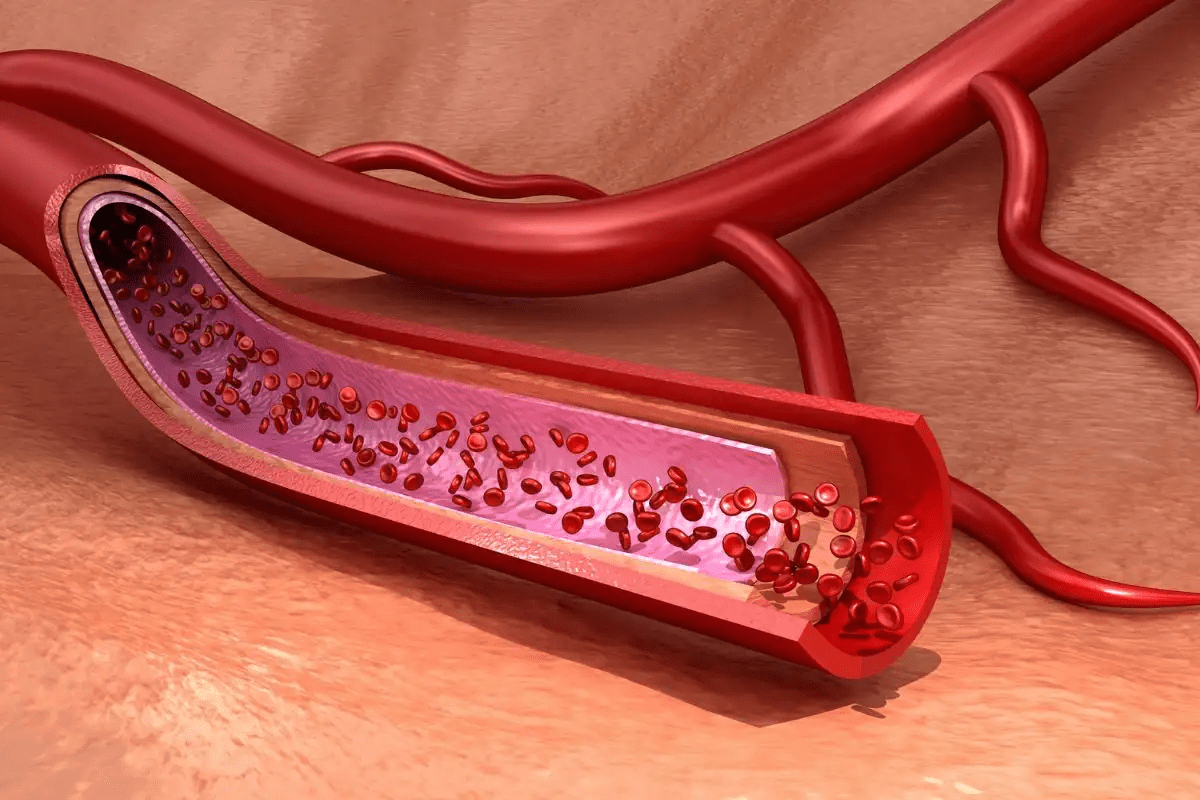
Mechanisms of Vision Damage in Uveitis
Uveitis can harm vision in several ways. Long-term inflammation can cause cataracts, glaucoma, and macular edema. These issues can lead to permanent vision loss if not treated right. We’ll look into how uveitis damages vision and why early treatment is key.
The ways uveitis damages vision are complex, involving inflammation that changes the eye’s structure. By understanding these, doctors can find better treatments to stop vision loss.
How Long Can Uveitis Last? Understanding Disease Duration
Knowing how long uveitis lasts is key to managing it well. Uveitis, an inflammatory eye condition, can greatly affect a person’s life if not managed right. The time uveitis lasts varies a lot, depending on several factors.
Acute vs. Chronic Uveitis
Uveitis is divided into two types: acute and chronic. Acute uveitis starts suddenly and usually lasts less than three months. It can often be treated well, and vision can be restored.
Chronic uveitis lasts more than three months. It needs ongoing care and can cause eye damage if not controlled well. Chronic uveitis can lead to long-term inflammation.
Factors Affecting Recovery Time and Recurrence
Many things can affect how long it takes to recover from uveitis and if it comes back. These include:
- The underlying cause of uveitis
- The effectiveness of the treatment plan
- The presence of any underlying health conditions
- The patient’s response to therapy
It’s important to understand these factors for effective treatment. We work closely with patients to monitor their condition and adjust treatment plans as needed to improve outcomes.
Recovery time can vary a lot among people. Some may get better quickly, while others may need longer treatment. Regular check-ups are key to managing the condition well and avoiding complications.
Risk Factors for Developing Sight-Threatening Uveitis
Several factors can increase the risk of getting sight-threatening uveitis. These include age, health conditions, and genetics. Knowing these risks helps in catching the condition early and managing it well.
Age-Related Risk Factors
Age is a big factor in uveitis. People over 60 are at higher risk of serious uveitis. This is because of aging and other health issues that come with it.
- Increased susceptibility to inflammation
- Higher likelihood of underlying health conditions
- Potential for delayed diagnosis due to attribution of symptoms to other age-related conditions
Underlying Health Conditions and Autoimmune Disorders
Some health conditions and autoimmune disorders raise the risk of uveitis. These can cause inflammation and harm the eyes.
Common underlying conditions include:
- Rheumatoid arthritis
- Lupus
- Multiple sclerosis
- Inflammatory bowel disease
These conditions can make the immune system attack the eye, causing uveitis.
Genetic and Environmental Factors
Genetics and environment also affect uveitis risk. People with a family history of uveitis or autoimmune diseases are more at risk.
Environmental triggers include:
- Infections
- Exposure to toxins
- Other external factors that may trigger an inflammatory response
Knowing these risk factors helps in preventing and treating uveitis early.
Vision-Threatening Complications of Untreated Uveitis
Untreated uveitis can cause serious damage to your eyes. It can lead to vision loss if not treated. This is because it can cause several serious problems.
Cataract Development
Untreated uveitis can cause cataracts. This is when the lens in your eye gets cloudy. It makes it hard to see. Surgery might be needed to fix this, but it can be harder with uveitis.
Glaucoma and Increased Eye Pressure
Uveitis can also cause glaucoma. This is when the pressure in your eye gets too high. It can harm your optic nerve and lead to vision loss. To manage this, doctors use medicines to lower the pressure and fight inflammation.
Cystoid Macular Edema
Cystoid macular edema (CME) is another problem that can happen. It’s when fluid builds up in the macula, making vision blurry. Doctors treat it with medicines to reduce swelling and improve sight.
Retinal Scarring and Detachment
Long-term inflammation from uveitis can cause scarring on the retina. This can lead to retinal detachment, a serious issue. It needs surgery to fix. Regular check-ups with an eye doctor are key to catching these problems early.
The table below shows the possible problems from untreated uveitis and how they are treated:
Complication | Description | Typical Treatment |
Cataract | Clouding of the lens | Cataract surgery |
Glaucoma | Increased intraocular pressure | Medications to reduce IOP |
Cystoid Macular Edema | Fluid accumulation in the macula | Anti-inflammatory medications |
Retinal Scarring/Detachment | Scarring or detachment of the retina | Surgical intervention |
Diagnosis and Medical Evaluation of Chronic Eye Inflammation
Getting a clear diagnosis is key to treating uveitis. It helps us understand how serious the inflammation is and how it affects the eye.
Comprehensive Eye Examination Procedures
We start with a detailed eye check-up. This helps us see how healthy the eye is. We look at:
- Visual acuity testing to check vision sharpness
- Slit-lamp examination to look at the front part of the eye
- Fundoscopy to check the back part, like the retina and vitreous
Slit-lamp microscopy is very important. It lets us see the front of the eye for signs of inflammation. Fundoscopy helps us check the back for signs of uveitis, like haze in the vitreous and problems with blood vessels in the retina.
Laboratory and Imaging Tests for Underlying Causes
To find out why uveitis is happening, we might do some tests. These include:
Test | Purpose |
Blood Tests | To find infections or autoimmune disorders |
Fluorescein Angiography | To see if there’s leakage or lack of blood in the retina |
Optical Coherence Tomography (OCT) | To check how thick the retina is and for swelling |
Tests like OCT and fluorescein angiography give us important details. They help us see how bad the damage is and if treatment is working.
“Accurate diagnosis is the cornerstone of effective uveitis management. By combining clinical examination findings with laboratory and imaging tests, we can tailor treatment to the individual needs of each patient.”
Treatment and Prevention Strategies to Preserve Vision
Keeping vision safe in uveitis patients needs a mix of treatments and prevention. It’s all about a detailed plan for each patient. This plan fits their unique situation and disease type.
Anti-Inflammatory and Immunosuppressive Medications
Corticosteroids are key in treating uveitis. They help lower inflammation. But, they can cause side effects over time. So, immunosuppressive drugs are used to help control the immune system.
“Our goal is to fight inflammation and avoid complications,” says Dr. [Last Name], an eye specialist. “By mixing anti-inflammatory and immunosuppressive treatments, we can greatly help our patients.”
Surgical Interventions for Complications
When uveitis causes problems like cataracts or glaucoma, surgery might be needed. Surgical treatments aim to fix these issues and improve vision. For example, cataract surgery can greatly help those with vision problems from uveitis.
Lifestyle Modifications and Preventive Measures
Medical and surgical treatments are just part of the solution. Lifestyle changes also play a big role. Regular eye check-ups, quitting smoking, and eating well are important. Wearing sunglasses to protect eyes from UV rays is also key.
Being proactive in managing uveitis can greatly reduce vision loss risk. As research grows, so does hope for those with uveitis.
Conclusion: Living with Uveitis and Protecting Your Eyesight
Uveitis is a complex eye condition that can harm your vision if not treated right. To protect your eyesight, you need a detailed plan. This plan helps prevent vision loss in the long run.
Getting an early diagnosis and treatment is key. Knowing the symptoms and treatment options helps you act fast. Regular eye checks and following your treatment plan are vital. This helps avoid serious problems like cataracts, glaucoma, and retinal scarring.
Keeping your eyes safe is more than just medical care. Healthy habits and staying informed are also important. We aim to provide top-notch healthcare and support for international patients. Our goal is to help you keep your vision and enjoy a good quality of life.
FAQ
What is uveitis?
Uveitis is a type of eye inflammation. It affects the uvea, the middle layer of the eye. This can cause vision problems and may lead to blindness if not treated.
Can uveitis lead to blindness?
Yes, uveitis can cause blindness if not managed properly. The risk of losing vision depends on the type and severity of uveitis. It also depends on how well treatment works.
How long does blurred vision last with uveitis?
The time blurred vision lasts with uveitis varies. It depends on how severe the inflammation is, how well treatment works, and any underlying conditions.
What are the symptoms of uveitis?
Symptoms of uveitis include eye pain, redness, and blurred vision. You might also feel sensitive to light and see floaters. The symptoms can differ based on the type of uveitis.
How is uveitis diagnosed?
Diagnosing uveitis involves a detailed eye exam. This includes checking your medical history, visual acuity tests, and lab and imaging tests. These help find the cause.
What are the risk factors for developing sight-threatening uveitis?
Risk factors for sight-threatening uveitis include age and certain health conditions. Genetic predispositions and environmental factors also play a role.
How is uveitis treated?
Uveitis treatment often includes anti-inflammatory and immunosuppressive medications. Sometimes, surgery is needed to address complications like cataracts or glaucoma.
Can uveitis be prevented?
While uveitis can’t be completely prevented, some lifestyle changes can help. These can reduce the risk of getting it or having it come back.
How long can uveitis last?
Uveitis can last from a few weeks to several years. It depends on whether it’s acute or chronic and how well treatment works.
What are the potentially serious complications of untreated uveitis?
Untreated uveitis can lead to serious problems. These include cataracts, glaucoma, cystoid macular edema, retinal scarring, and detachment. These can cause permanent vision loss.
Is chronic uveitis curable?
Chronic uveitis is not curable, but it can be managed. Treatment aims to control inflammation, preserve vision, and prevent complications.
References
National Center for Biotechnology Information. Uveitis: Risks, Inflammation, and Preventable Vision Loss. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC1772296/