For those with severe obesity, duodenal switch surgery complications can be a game-changer. It leads to significant and lasting weight loss. This surgery removes a big part of the stomach and changes the small intestine’s path.
It’s very effective, but knowing the risks and side effects is key. This knowledge helps patients make better choices.
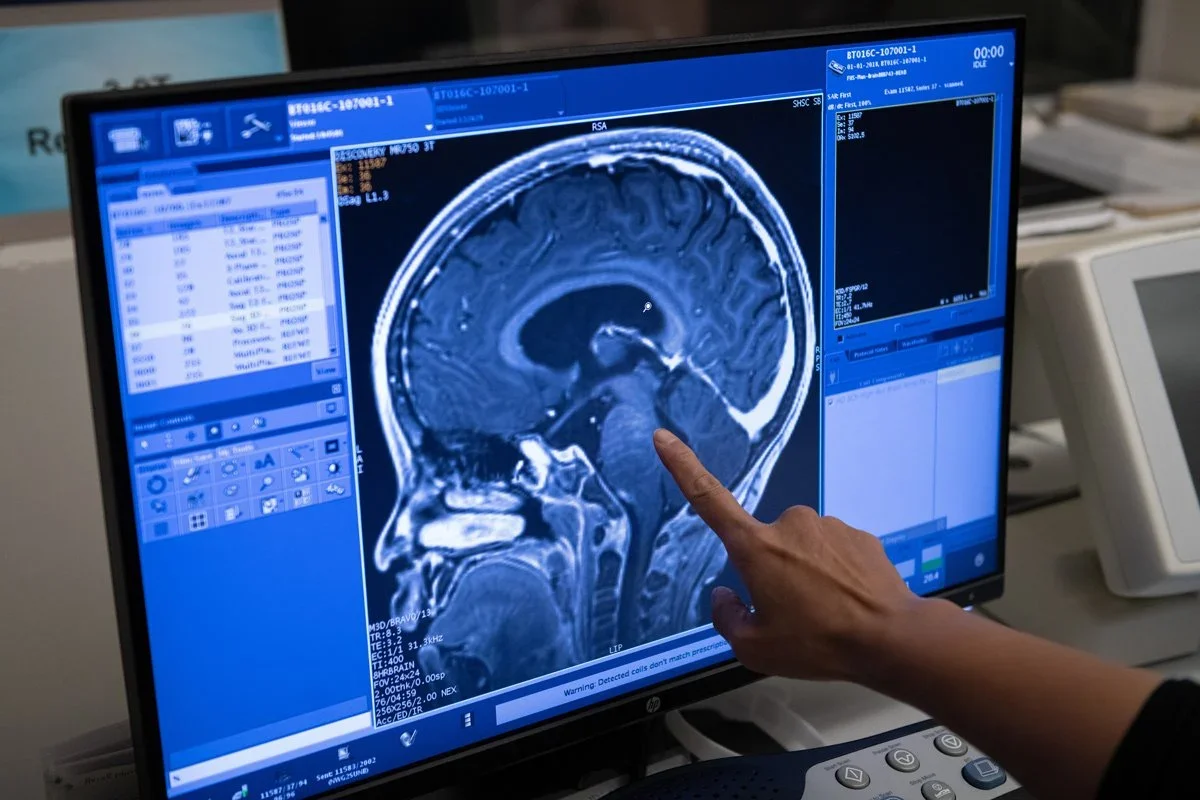
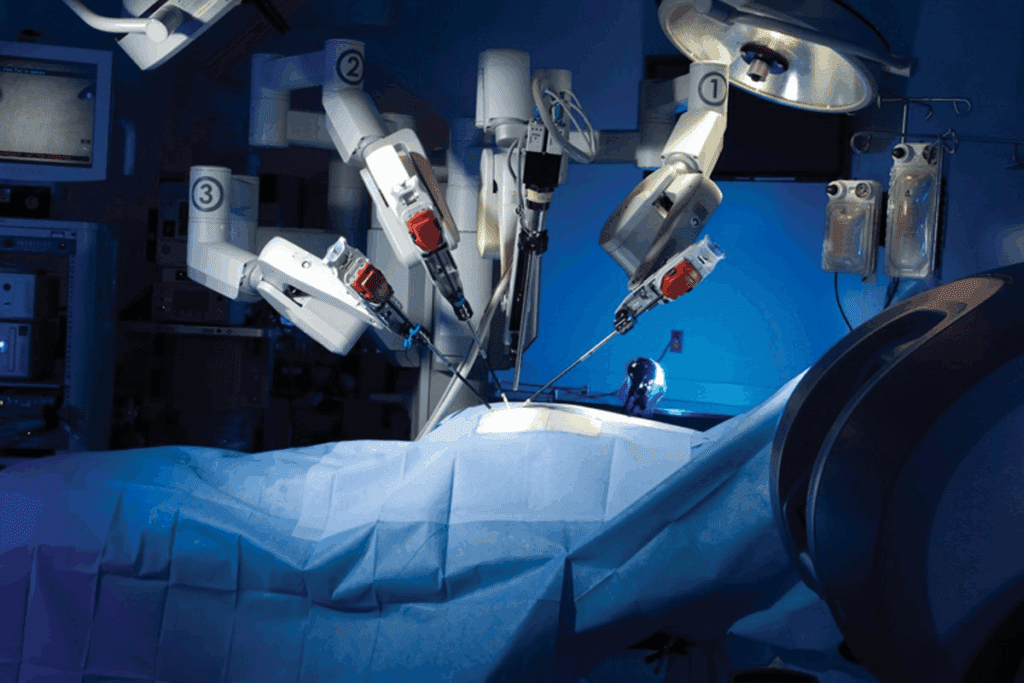
At Liv Hospital, we provide top-notch bariatric care. Our team of experts works together to support patients on their weight loss journey. We use advanced surgical techniques and tailor care to each patient. This way, we help them reach their weight loss goals safely.
Key Takeaways
- Duodenal switch surgery is a highly effective weight loss solution for severe obesity.
- The procedure involves removing up to 80% of the stomach and rerouting the small intestine.
- Understanding the risks is vital for making informed choices.
- Liv Hospital offers world-class bariatric care with a multidisciplinary team of experts.
- Advanced surgical techniques and personalized care help avoid complications.
Understanding Duodenal Switch Surgery

Duodenal switch surgery is a complex weight loss method. It combines sleeve gastrectomy with biliopancreatic diversion. This makes it a strong solution for those with severe obesity.
What is Biliopancreatic Diversion with Duodenal Switch (BPD-DS)
BPD-DS is a bariatric surgery with two parts. It starts with removing a big part of the stomach, like a sleeve gastrectomy. Then, it reroutes the small intestine to cut down on nutrient absorption. This limits food intake and reduces calorie absorption.
How the Procedure Promotes Weight Loss
The duodenal switch works in two ways: restriction and malabsorption. The sleeve gastrectomy limits how much food you can eat. The intestinal bypass cuts down on nutrient absorption. Together, they lead to significant weight loss, often 70 to 80% of excess weight in two years.
Expected Outcomes and Success Rates
Patients can expect big weight loss and health improvements from duodenal switch surgery. The success rate is high, with many seeing weight loss and better health. Sticking to diet plans and regular check-ups are key to keeping weight off and avoiding complications.
Duodenal Switch Surgery Complications: Statistical Overview
It’s important to know about the complications of duodenal switch surgery before deciding on it. We’ll look at how often these problems happen, what increases the risk, and compare them to other surgeries.
Incidence Rates in Clinical Research
Studies give us a clear picture of the complications after duodenal switch surgery. About 15% of patients face early complications. Bowel obstruction is a big issue, affecting around 16% of patients.
We’ve gathered data from many studies to give you a full view of complication rates.
| Complication | Incidence Rate (%) |
|---|---|
| Bowel Obstruction | 16 |
| Anastomotic Leaks | 2-5 |
| Nutritional Deficiencies | 30-40 |
| Ventral Hernias | 10-15 |
Risk Factors That Increase Complication Likelihood
Some factors can make complications more likely after duodenal switch surgery. These include pre-existing medical conditions like diabetes and high blood pressure. Also, having had surgery before can increase risks. Knowing these factors helps in managing and reducing complications.
Comparison with Other Bariatric Procedures
It’s key to compare complication rates when choosing a bariatric surgery. Duodenal switch surgery has a higher rate of complications than some, like gastric bypass. Yet, it offers significant weight loss for many.
Here’s a table comparing complication rates of duodenal switch with other common surgeries:
| Bariatric Procedure | Complication Rate (%) |
|---|---|
| Duodenal Switch | 15-20 |
| Gastric Bypass | 10-15 |
| Sleeve Gastrectomy | 5-10 |
Understanding the complications of duodenal switch surgery helps both patients and doctors make better choices. It’s about weighing the risks against the benefits.
Complication #1: Anastomotic Leaks
Anastomotic leaks are serious and can be life-threatening after duodenal switch surgery. These leaks happen when the connection between two parts of the intestine breaks. This allows intestinal contents to leak into the abdominal cavity.
Causes of Anastomotic Leaks
Several factors can lead to anastomotic leaks after duodenal switch surgery. These include:
- Technical issues during surgery, such as imperfect suturing or stapling
- Poor blood supply to the anastomotic site
- Tension on the anastomosis
- Pre-existing conditions that impair healing, such as diabetes or malnutrition
Understanding these risk factors is key for both surgeons and patients. It helps in reducing the chance of anastomotic leaks.
Symptoms and Warning Signs
It’s important to recognize the symptoms of anastomotic leaks early. Common signs include:
- Severe abdominal pain
- Fever
- Tachycardia
- Abdominal tenderness
If you notice any of these symptoms after duodenal switch surgery, seek medical help right away.
Treatment Approaches
The treatment for anastomotic leaks often involves a few steps:
- Drainage of the leak, either percutaneously or surgically
- Administration of antibiotics to manage infection
- Nutritional support to promote healing
- In some cases, additional surgery may be required to repair the leak
Quick treatment is essential to prevent further complications and improve outcomes.
| Treatment Approach | Description |
|---|---|
| Drainage | Removal of leaked intestinal contents to prevent further infection |
| Antibiotics | Administration of antibiotics to manage and prevent infection spread |
| Nutritional Support | Ensuring adequate nutrition to support the healing process |
| Surgical Repair | In some cases, additional surgery is needed to repair the anastomotic leak |
Dealing with complications like anastomotic leaks can be tough. Our team is dedicated to providing full care and support to manage these risks effectively.
Complication #2: Bowel Obstruction
Bowel obstruction is a common problem after Duodenal Switch surgery. It affects about 16% of patients. This is a big worry for both patients and doctors.
Mechanisms of Intestinal Blockage
Several things can cause bowel obstruction after Duodenal Switch. Adhesions are bands of tissue that can block the intestine. Internal hernias happen when part of the intestine bulges through a weak spot. Intussusception is when one part of the intestine slides into another, blocking it.
Warning Signs and Symptoms
It’s important to know the signs of bowel obstruction. Patients might feel abdominal pain, nausea, and vomiting. They might also have trouble passing gas or stool. These symptoms can get worse over time.
Diagnostic and Treatment Protocols
To diagnose bowel obstruction, doctors use imaging tests. A CT scan helps find the problem and where it is. Treatment often involves surgery to fix the blockage. The surgery aims to remove the blockage and get the intestine working right again.
In summary, bowel obstruction is a serious issue after Duodenal Switch surgery. Knowing the causes, symptoms, and treatments helps patients manage their care better.
Complication #3: Hemorrhage and Bleeding
Post-operative hemorrhage is a serious risk with duodenal switch surgery. Bleeding can happen, and it’s key for patients to know the risks and signs.
Common Sites of Post-operative Bleeding
Bleeding can happen at the surgery site or inside the belly. It often occurs at the places where tissue was cut or stapled. It’s vital to spot and treat bleeding quickly to avoid serious problems.
Recognizing Hemorrhage Symptoms
Symptoms of post-operative hemorrhage include fast heart rate, low blood pressure, and belly pain. Patients might also feel dizzy, faint, or see a big drop in hemoglobin levels. Patients should get medical help right away if they notice these signs.
“Bleeding is a common immediate complication, reported in 2.7% of RYGB cases, and duodenal switch surgery carries similar risks.”
Emergency Interventions
Emergency care for hemorrhage involves making the patient stable and possibly more surgery to stop the bleeding. Quick action is key to avoid severe issues. We stress the need for careful watching and follow-up to manage and lower the risk of bleeding.
In summary, while hemorrhage is a serious issue with duodenal switch surgery, knowing the risks, symptoms, and emergency steps can greatly help patient results. We’re dedicated to giving our patients full care and support during their treatment.
Complication #4: Nutritional Deficiencies
Duodenal Switch Surgery helps with weight loss but can cause nutritional problems if not managed right. This major issue comes from not absorbing important nutrients well.
Protein Malnutrition Risks
Protein malnutrition is a big risk with Duodenal Switch Surgery. Patients need to eat enough protein to avoid malnutrition. This can cause muscle loss and weaken the immune system.
Essential Vitamin and Mineral Deficiencies
Patients might not get enough vitamin B12, iron, and other key nutrients because of malabsorption. These shortages can lead to anemia, fatigue, and even neurological problems.
Supplementation Requirements
To avoid these problems, lifelong supplements are needed. Patients must take personalized vitamin and mineral supplements to get the nutrients they need.
Monitoring Protocols and Lab Testing
It’s important to do regular lab tests to check nutritional levels and adjust supplements if needed. We suggest regular visits to a healthcare provider to manage nutritional deficiencies well.
By knowing the risks and taking action, patients can lower the chance of nutritional problems. This helps them get a better outcome after Duodenal Switch Surgery.
Complication #5: Gastrointestinal Issues
Duodenal switch surgery can cause many gastrointestinal problems. The changes in the digestive system can lead to issues that affect life quality after surgery.
Chronic Diarrhea and Malabsorption
Chronic diarrhea is a common problem after this surgery. It often comes with malabsorption of important nutrients. This happens because the intestine’s surface area to absorb food is reduced. Malabsorption can cause a lack of essential vitamins and minerals, so it’s important to watch and supplement.
To deal with chronic diarrhea, patients need to change their diet a lot. They should eat smaller meals more often and avoid foods that make diarrhea worse.
Dumping Syndrome
Dumping syndrome happens when food, like sugar, moves too fast from the stomach to the small intestine. Symptoms include nausea, vomiting, diarrhea, stomach cramps, and flushing. The severity of dumping syndrome can vary among patients, but it’s usually managed with diet changes.
Patients are told to avoid sugary foods and drinks. They should eat smaller meals and drink liquids separately from solid food to help symptoms.
Gastroesophageal Reflux Disease (GERD)
GERD is when stomach acid flows back into the esophagus often. This can irritate the esophagus lining, causing discomfort. After duodenal switch surgery, the risk of GERD may go up because of the changed anatomy.
Dietary Modifications for Symptom Control
Changing your diet is key to managing issues like chronic diarrhea, dumping syndrome, and GERD. Patients are advised to follow a tailored diet that includes eating smaller, more frequent meals. They should avoid foods that trigger problems and get enough nutrients through supplements if needed.
A sample dietary plan might include:
- Eating lean proteins and vegetables
- Avoiding high-sugar and high-fat foods
- Incorporating fiber-rich foods to manage diarrhea
- Staying hydrated by drinking plenty of water
By adjusting their diet, patients can lessen the severity of these complications. This can greatly improve their quality of life after duodenal switch surgery.
Complication #6: Ventral Hernias and Wound Complications
Duodenal switch surgery helps with weight loss but also risks ventral hernias and wound problems. Ventral hernias happen when tissue bulges through the abdominal wall, often at a surgical cut. We’ll look at how these issues develop, their symptoms, diagnosis, and how to prevent them. We’ll also talk about fixing them with surgery.
Development and Risk Factors
Ventral hernias can happen because of the surgery cut and changes in abdominal pressure. Several things can make you more likely to get ventral hernias, including:
- Previous abdominal surgery: Past surgeries can weaken the abdominal wall.
- Obesity: Being overweight adds extra pressure on the abdominal wall.
- Poor wound healing: Issues like diabetes or smoking can slow healing.
Symptoms and Diagnosis
The signs of ventral hernias can differ, but common ones are:
- A visible bulge or lump near the surgical site
- Pain or discomfort, mainly when coughing, lifting, or bending
- Nausea or vomiting in severe cases
Doctors usually diagnose ventral hernias with a physical check-up and might use imaging like ultrasound or CT scans.
Preventive Measures
To lower the chance of ventral hernias, you can take a few steps:
- Proper wound care: Make sure the surgical area heals right.
- Using mesh during initial surgery: Adding mesh to the abdominal wall can help.
- Lifestyle modifications: Keep a healthy weight and avoid heavy lifting.
Surgical Repair Options
If ventral hernias happen, surgery is usually needed. The surgery aims to strengthen the weak area, often with mesh. The type of surgery depends on the hernia’s size, location, and the patient’s health.
Handling complications like ventral hernias can be tough. Our team is dedicated to giving full care and support to tackle these problems well.
Complication #7: Psychological and Lifestyle Impacts
Duodenal switch surgery changes more than just your body. It affects your mind and lifestyle too. People going through this surgery face big emotional and social changes.
Body Image Changes
One big change is how you see yourself. Patients often feel a big shift in body image. This can be both empowering and hard.
As you lose weight, you might see your body differently. This can affect your self-esteem and identity. It’s important to have support to deal with these changes.
Counseling and support groups are key. They help you adjust to your new body image and emotional changes.
Eating Behavior Adjustments
Patients must change how they eat after surgery. They need to follow a strict diet, eat small meals, and avoid certain foods. These changes can be tough and may cause anxiety about food.
To handle these changes, learning about proper nutrition and meal planning is vital. A dietitian or nutritionist can help create a meal plan that’s healthy and meets your needs.
Relationship with Food
After surgery, your relationship with food changes a lot. You need to learn to eat in a healthy way. This means eating mindfully, listening to your hunger and fullness cues, and avoiding unhealthy foods.
Support Resources and Coping Strategies
Patients need strong support to deal with these changes. This includes psychological counseling, support groups, and education on nutrition and lifestyle. With these resources, you can better handle the challenges of duodenal switch surgery.
A good support system is key to recovery and success. By understanding the psychological impacts and providing support, we help our patients not just lose weight but also improve their quality of life.
Conclusion
It’s important to know about duodenal switch surgery complications to give the best care. These issues can include leaks, blockages, and problems with nutrition and mental health. Handling these problems well is essential for good results.
Managing these issues needs a detailed plan. This includes choosing the right patients, doing the surgery carefully, and taking good care after. Knowing the risks helps doctors and patients work together better.
We aim to give top-notch care to patients from around the world. By tackling duodenal switch surgery complications, we can make patients’ lives better. This improves their health and happiness.
FAQ
What are the most common complications of duodenal switch surgery?
Common issues include anastomotic leaks, bowel obstruction, and hemorrhage. Nutritional deficiencies and gastrointestinal problems are also common. Ventral hernias and psychological impacts are other possible complications.
How can I identify symptoms of an anastomotic leak after duodenal switch surgery?
Look out for abdominal pain, fever, and tachycardia. These signs may indicate an infection. If you notice these symptoms, get medical help right away.
What are the risks of bowel obstruction after duodenal switch surgery?
Bowel obstruction can happen due to adhesions or internal hernias. Symptoms include pain, nausea, and vomiting. Doctors usually use CT scans to diagnose it.
How can nutritional deficiencies be managed after duodenal switch surgery?
Patients need lifelong supplements and regular check-ups. Lab tests help ensure they get enough nutrients.
What dietary modifications can help manage gastrointestinal issues after duodenal switch surgery?
Eating smaller meals and avoiding certain foods can help. This approach can manage symptoms like diarrhea and GERD.
What are the risks of ventral hernias after duodenal switch surgery?
Ventral hernias can occur at the surgical site. Proper wound care and mesh use can help prevent them. If they happen, surgery is usually needed to fix them.
How can patients cope with the psychological impacts of duodenal switch surgery?
Patients need ongoing support and counseling. This helps with body image and eating behavior changes. Support and strategies are key for success.
What are the long-term complications of duodenal switch surgery?
Long-term issues include nutritional deficiencies and gastrointestinal problems. Psychological impacts are also possible. Ongoing care and support are essential to manage these risks.
How can I minimize the risk of complications after duodenal switch surgery?
To reduce risks, prepare well before surgery and follow post-op instructions. Regular follow-ups with your doctor are also important.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19885793/).
- Dorman, R. B., et al. (2012). Benefits and complications of the duodenal switch: A review. PubMed. https://pubmed.ncbi.nlm.nih.gov/22959653/