An epiretinal membrane is a thin layer of tissue on the retina. It can make your vision blurry and cause blind spots.What is ERM retina? This essential guide explains the epiretinal membrane, how serious it is, and treatment options.
As we get older, the chance of getting this condition goes up. It’s common among older people around the world. Knowing about epiretinal membrane is key to keeping your eyes healthy.
At Liv Hospital, we focus on treating epiretinal membrane and other eye problems. Our team creates custom plans to help you keep your vision sharp.
Key Takeaways
- Epiretinal membrane is a condition that affects the retina, causing visual disturbances.
- The risk of developing epiretinal membrane increases with age.
- Understanding the causes, symptoms, and treatment options is critical for eye health.
- Liv Hospital provides detailed care for patients with epiretinal membrane.
- Custom treatment plans are available to protect your vision.
Understanding Epiretinal Membrane (ERM)

Epiretinal membrane (ERM) is a condition where a layer of fibrous tissue forms on the retina. This happens on the macula, which is key for central vision. The retina is a complex neural tissue that lines the inner eye surface. It plays a vital role in converting light into signals for the brain.
The formation of an ERM can distort this process. This can lead to visual disturbances.
The anatomy of ERM includes the retina’s internal limiting membrane. This is where fibrocellular proliferation occurs. This membrane is between the retina and the vitreous body, a gel-like substance in the eyeball’s center.
Understanding this anatomy is key to knowing how ERM affects vision. It also helps us understand the challenges in treating it.
How ERM Forms on the Retinal Surface
The formation of an epiretinal membrane is complex. It involves the growth of various cells on the retina’s surface. These include glial cells, retinal pigment epithelial cells, and inflammatory cells.
This process can start due to several factors. These include posterior vitreous detachment (PVD), retinal tears, or eye inflammation. As these cells grow, they form a membrane. This membrane can contract and cause retinal distortion.
This can lead to symptoms like blurred vision and distorted vision. The progression of ERM varies among people. Some may experience significant visual problems, while others may not notice anything.
Understanding what causes ERM to form and progress is key. It’s essential for finding effective ways to manage it.
The Prevalence of ERM Retina Conditions
[Add image here]
Epiretinal membrane (ERM) retina conditions are a big worry worldwide. They affect a lot of people. Knowing how common ERM is helps both patients and doctors.
Global Statistics and Demographics
Research shows ERM’s prevalence changes a lot in different groups. It’s estimated that 5-10% of people over 50 have ERM. This number will likely go up as more people get older.
Some groups get ERM more often. For example, people with myopia and those who’ve had cataract surgery are more likely to get it. Also, ERM seems to affect men and women differently, with women possibly getting it more.
Age-Related Prevalence Patterns
Getting older increases your risk of getting ERM. It’s more common after 50. Up to 20% of people over 70 might have it. This shows why eye checks are important as we age.
Regional Variations in ERM Occurrence
ERM’s prevalence varies by region and ethnicity. For instance, some studies say it’s more common in Asians than Caucasians. This shows we need more specific data to understand ERM better.
In summary, ERM’s prevalence is influenced by many factors like age, demographics, and where you live. Knowing these helps us find better ways to diagnose and treat ERM.
Types and Classification of Epiretinal Membranes
Epiretinal membranes are divided into primary and secondary types. Each type has its own features. Knowing this helps doctors understand how the condition affects vision and choose the right treatment.
Primary (Idiopathic) ERM
Primary or idiopathic epiretinal membranes happen without a known cause. They are more common in older people. The exact mechanism of primary ERM formation is not fully understood, but it’s thought to involve cell growth and membrane formation on the retina.
Secondary ERM
Secondary epiretinal membranes are linked to eye diseases or surgeries. Conditions like diabetic retinopathy, retinal detachment, and eye trauma can cause them. The presence of secondary ERM often complicates the management of the underlying condition, requiring a detailed treatment plan.
Here are some common causes of secondary ERM:
- Diabetic retinopathy
- Retinal detachment
- Ocular trauma
- Previous ocular surgeries
Classification Based on Severity
ERM can also be classified by how severe it is. This is usually done with imaging like optical coherence tomography (OCT). The severity helps decide if surgery is needed and when.
Experts say, “The classification of ERM based on severity is a critical step in managing the condition effectively.”
“Accurate assessment of ERM severity is essential for clinicians to decide on the most appropriate treatment strategy, optimizing patient outcomes.”
Understanding the types and classification of epiretinal membranes is key for both doctors and patients. It helps in diagnosing and treating the condition. This improves the quality of life for those with ERM.
Common Causes and Risk Factors
Knowing the causes and risk factors of Epiretinal Membrane (ERM) helps in early detection and management. Age-related changes, other eye conditions, and health issues all play a role. This shows that a mix of factors contributes to ERM.
Age-Related Changes
Age is a big risk factor for ERM. As we get older, the vitreous gel in our eyes changes. This can cause ERM. Age-related changes are a main factor because ERM risk goes up after 50.
Posterior Vitreous Detachment
Posterior Vitreous Detachment (PVD) is also linked to ERM. PVD happens when the vitreous gel separates from the retina. It’s common with age and can lead to ERM. The relationship between PVD and ERM shows why it’s key to watch retinal health after PVD.
Other Ocular Conditions
Other eye conditions can raise ERM risk. These include diabetic retinopathy, retinal tears, and past eye surgeries. Knowing how these conditions relate to ERM can help manage and prevent ERM.
Systemic Risk Factors
Health issues like diabetes and high blood pressure also increase ERM risk. Managing these conditions is important for overall health and lowering ERM risk.
To understand the link between these risk factors and ERM, let’s look at the data in the table below:
Risk Factor | Description | Association with ERM |
Age-Related Changes | Natural aging process affecting the vitreous gel | Strongly associated, specially after age 50 |
Posterior Vitreous Detachment | Separation of vitreous gel from the retina | Associated; can lead to ERM formation |
Diabetic Retinopathy | Complication of diabetes affecting the retina | Increases risk of ERM |
Systemic Conditions (Diabetes, Hypertension) | Health conditions affecting overall vascular health | Linked to increased risk of ERM |
By knowing these causes and risk factors, people can take steps to keep their eyes healthy. This can help lower the risk of getting Epiretinal Membrane.
Signs and Symptoms of Epiretinal Membrane
Knowing the signs and symptoms of ERM is key for early treatment. It’s important to spot the early signs of Epiretinal Membrane to act fast.
Visual Disturbances
Visual disturbances are a main symptom of ERM. People often see blurred vision or distorted vision. Straight lines might look wavy or crooked.
Metamorphopsia is when images look distorted. This makes it hard to read, drive, or even see faces clearly.
Progression of Symptoms
The symptoms can change a lot from person to person. Some might stay the same for years, while others get worse. How fast it gets worse depends on how thick the membrane is and if there are other eye problems.
Symptom | Early Stage | Advanced Stage |
Visual Distortion | Mild blurring | Significant distortion |
Visual Acuity | Minimal impact | Significant loss |
When Symptoms Require Medical Attention
If your vision suddenly gets worse, see a doctor right away. They can figure out what to do next.
It’s smart to get your eyes checked often, if you’re at risk for ERM or already have it. Catching it early can make treatment more effective.
How Serious Is Epiretinal Membrane?
Understanding the seriousness of epiretinal membrane (ERM) means looking at how it compares to other eye problems. We’ll see how ERM stacks up against other eye issues, its effects on daily life, and what happens if it’s not treated.
Comparing ERM to Other Retinal Conditions
ERM is often compared to conditions like macular degeneration and retinal detachment. While they share some traits, ERM is different in severity and vision impact. For example, retinal detachment is more severe and can cause sudden vision loss if not treated quickly. ERM, on the other hand, progresses slowly and usually doesn’t cause complete vision loss.
Condition | Severity | Progression Rate | Impact on Vision |
Epiretinal Membrane (ERM) | Mild to Moderate | Slow | Distorted Vision, Blurred Vision |
Macular Degeneration | Moderate to Severe | Variable | Central Vision Loss |
Retinal Detachment | Severe | Rapid | Sudden Vision Loss |
Impact on Vision and Daily Activities
ERM can significantly affect vision, causing blurred and distorted vision. These symptoms can make everyday tasks like reading and driving harder. A study in the Ophthalmology Journal found that ERM patients struggle with tasks needing sharp vision.
“ERM can significantly affect a patient’s quality of life by impairing their visual acuity and causing discomfort.”
For patients, the impact on daily life is a big concern. Simple tasks become challenging, which can lower overall quality of life.
Long-term Progression Without Treatment
How ERM progresses without treatment varies. Some people may keep stable vision for years, while others see a slow decline. Regular eye exams are key to tracking ERM’s progression and discussing treatment options with an eye doctor.
We advise patients with ERM to stay in close touch with their healthcare provider. This helps manage the condition effectively and address any concerns about its seriousness and vision impact.
Diagnosing Epiretinal Membrane
To find out if someone has an epiretinal membrane, doctors use many methods. They need to be sure to pick the right treatment. This helps the patient get better faster.
Clinical Examination Techniques
First, doctors do a detailed check-up. They test how well you can see with a visual acuity test. They also look at your retina with a fundus examination.
They use indirect ophthalmoscopy and slit-lamp biomicroscopy to see the retina. This helps them find any signs of ERM.
Imaging Technologies
Modern tools are key in finding ERM. Optical Coherence Tomography (OCT) gives clear pictures of the retina and the membrane. This helps doctors understand how thick the membrane is and its effect on the retina.
Fluorescein angiography is also used. It helps doctors see the blood vessels in the retina. This can show if there are any other problems.
Differential Diagnosis
Doctors must figure out if it’s really ERM. They compare it with other eye problems that look similar. This includes vitreomacular traction syndrome and macular edema.
By combining careful checks and new imaging, doctors can accurately diagnose ERM. This helps them treat it right and avoid confusing it with other eye issues.
Treatment Options for ERM
There are many ways to treat ERM, including watching it, surgery, and care after surgery. The right treatment depends on how bad the symptoms are, how much they affect your vision, and your overall health.
Observation and Monitoring
If your ERM symptoms are mild, you might just watch it closely. This means regular eye tests and pictures of your retina to see if it’s getting worse.
Surgical Interventions
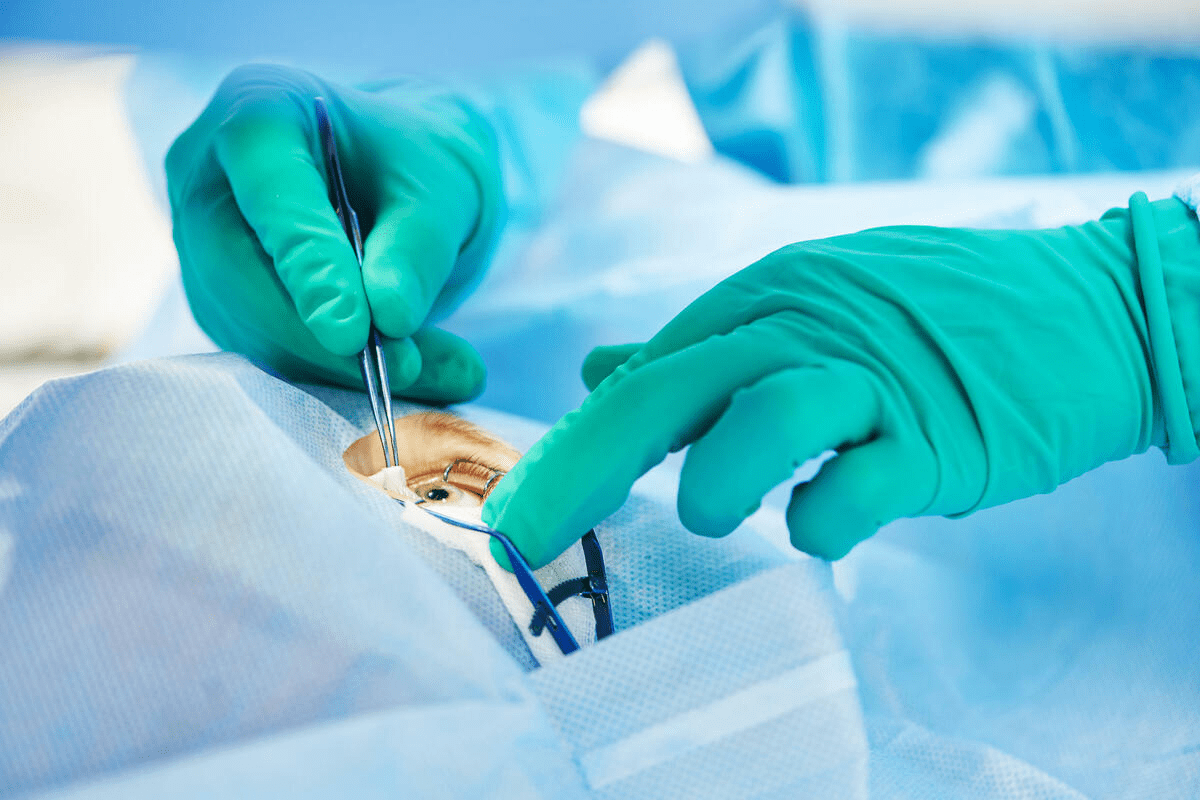
If ERM is really messing with your vision, surgery might be needed. The main surgery for ERM is vitrectomy with membrane peeling. This means removing the vitreous gel and carefully taking off the membrane from your retina.
Here’s a summary of the surgical outcomes:
Surgical Outcome | Description | Success Rate |
Visual Improvement | Improvement in visual acuity post-surgery | 70-80% |
ERM Recurrence | Recurrence of ERM after surgery | 5-15% |
Complications | Occurrence of surgical complications | <5% |
Post-Surgical Care
After surgery, you’ll need to follow a special care plan to heal well. This includes using eye drops to prevent infection, avoiding hard activities, and going to all your follow-up appointments.
Emerging Treatment Approaches
Scientists are always looking for new ways to treat ERM. They’re exploring medicines that might stop the membrane from forming or make it go away. These new treatments are promising, but they’re not yet proven safe and effective in big studies.
We keep an eye on the latest in ERM treatment. Our goal is to offer the best and most advanced care for our patients.
Complications and Prognosis
It’s important for patients and doctors to know about Epiretinal Membrane’s complications and how it will turn out. We need to look at different things that can change how well someone does.
Potential Complications
ERM can cause problems like retinal detachment, vitreomacular traction, and cataract formation. These issues can really affect how well someone can see and their quality of life.
“The development of complications in ERM patients highlights the need for close monitoring and quick action,” say experts. Seeing an eye doctor regularly is key to managing these risks.
Recovery Timeline
How long it takes to get better after ERM treatment, like surgery, can differ for everyone. Most people see their vision get better slowly over a few months after surgery.
- Right after surgery: Rest and check-ups
- Short-term (weeks to months): Vision starts to get better
- Long-term (months to a year or more): Vision keeps getting better and then stabilizes
Visual Outcome Expectations
Most people see their vision improve after ERM surgery. But, how much better it gets can depend on other eye problems.
Factors Affecting Prognosis
Several things can affect how well someone does with ERM. These include how bad the membrane is, if there are other eye problems, and the person’s overall health. Knowing these helps set realistic hopes and plan the best care.
In summary, ERM is tough, but knowing about its problems and how it might end up helps us take better care of those affected.
Conclusion
Managing epiretinal membrane (ERM) well is key to keeping your vision sharp and improving your life quality. We’ve covered what ERM is, how common it is, its types, causes, symptoms, how it’s diagnosed, and treatment choices.
Handling ERM right means using a full approach. This includes watching it closely, monitoring it, and sometimes surgery. Knowing how important treatment is helps a lot. It can really change how the condition goes and how well you can see.
Learning about ERM and its treatments helps patients make better choices for their care. We stress the need to see a doctor if symptoms don’t go away or get worse. This ensures you get the best care for ERM.
FAQ
What is epiretinal membrane (ERM) in ophthalmology?
Epiretinal membrane, also known as macular pucker or premacular fibrosis, is a condition. It forms a layer of fibrous tissue on the retina’s surface. This can cause visual disturbances.
How serious is epiretinal membrane?
ERM’s severity can vary. Some cases are mild and don’t affect vision much. But, others can cause significant vision loss, impacting daily life.
What are the causes of epiretinal membrane?
ERM can be caused by aging, posterior vitreous detachment, and other eye conditions. Systemic risk factors also play a role.
What are the symptoms of epiretinal membrane?
Symptoms include blurred vision, distorted vision (metamorphopsia), and double vision. These symptoms can worsen over time if not treated.
How is epiretinal membrane diagnosed?
Diagnosis involves clinical exams and imaging. Techniques like fundus examination and optical coherence tomography (OCT) are used.
What are the treatment options for epiretinal membrane?
Treatment options range from monitoring mild cases to surgery for severe cases. Surgery includes vitrectomy with membrane peeling.
What is the prognosis for epiretinal membrane?
The prognosis depends on the condition’s severity, treatment success, and individual eye health.
Can epiretinal membrane recur after treatment?
Yes, recurrence is possible. This highlights the need for post-surgical care and follow-up appointments.
Are there any emerging treatment approaches for ERM?
Research is exploring new treatments. This includes pharmacological interventions and advancements in surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560703/