Every 40 seconds, someone in the United States has a heart attack. A stent is a medical device. It helps restore blood flow in blocked arteries. Reaffirming the criteria for intervention and the necessary blockage percentage for stent placement for optimal outcomes.
Coronary artery disease is a top cause of heart attacks. Knowing when a stent is needed is key. The choice to use a stent depends on the artery blockage severity.
It’s important to understand coronary artery disease to know how blockages happen and affect the heart. This disease narrows or blocks the coronary arteries, which carry blood to the heart. It’s a major cause of heart attacks and other heart problems.
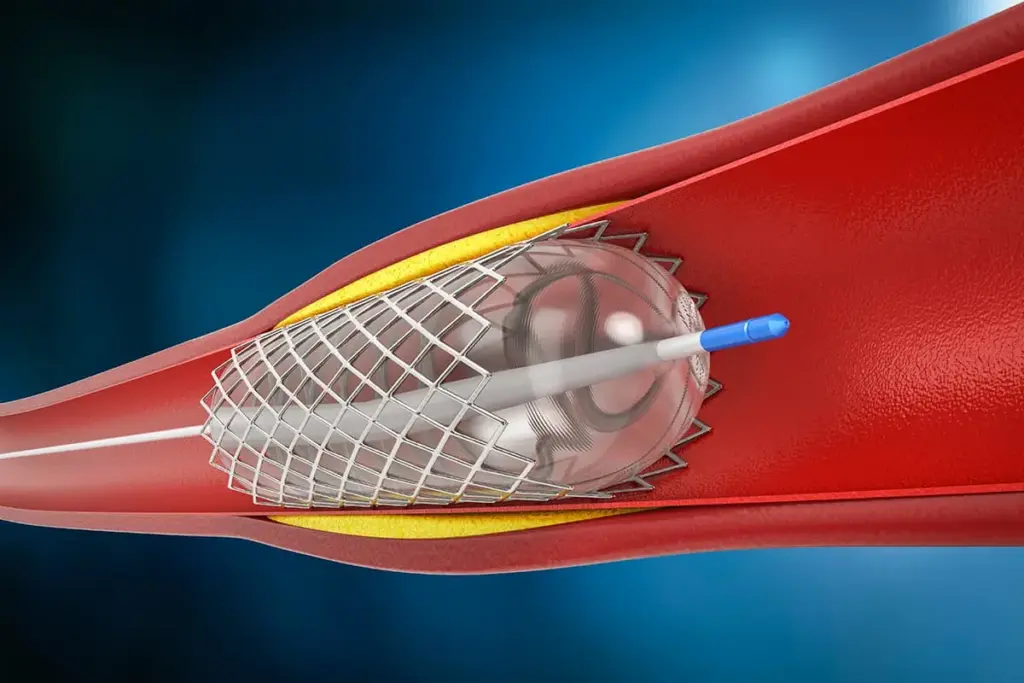
Atherosclerosis is when arteries get blocked. It happens when plaque, a mix of fat, cholesterol, and other stuff, builds up inside the arteries. This buildup can narrow the arteries, reducing blood flow to the heart. Atherosclerosis is a gradual process that can be affected by diet, lifestyle, and genetics.
It’s key to measure how severe artery blockages are to choose the right treatment. Doctors use coronary angiography to see the blockage and fractional flow reserve (FFR) to check pressure differences. These tools help doctors decide if a stent is needed.
Blockage severity is measured as a percentage. A higher percentage means a more severe blockage. For example, a blockage of 50% or more might need a stent.
Figuring out when a stent is needed is key in managing heart disease. Not every blockage needs a stent. The choice depends on how bad the blockage is and how it affects the patient’s health.
Moderate blockages, between 50-70%, are a tricky spot for stent decisions. Doctors look at symptoms, overall health, and test results like Fractional Flow Reserve (FFR). FFR measures pressure differences in coronary arteries during angiography.
Studies show stenting can help patients with moderate blockages, if FFR shows significant ischemia. The FFR helps us find which blockages cause ischemia and need stenting.
“The FFR helps us identify which lesions are causing ischemia and would benefit from stenting.”
Blockages over 70% usually need a stent to improve blood flow. These blockages cause more symptoms and increase the risk of heart problems. Stenting is often the clear choice to restore blood flow and ease symptoms.
|
Blockage Severity |
Typical Treatment Approach |
Considerations |
|---|---|---|
|
Moderate (50-70%) |
Stent placement considered based on FFR and symptoms |
Patient’s overall health, presence of symptoms |
|
Severe (>70%) |
Stent placement typically recommended |
Significant impairment of blood flow, risk of cardiac events |
The left main coronary artery is vital for the heart. Blockages here are very serious. Stenting is often advised for blockages over 50% in this artery to avoid severe problems.
About 600,000 stenting procedures happen in the U.S. each year. This shows how critical it is to know when to use stents.
Deciding on stent placement is more than just looking at blockage percentages. While blockage degree is key, other factors also play a role in stent decisions.
Symptom severity and quality of life are big factors. Patients with severe angina or other debilitating symptoms might get stents, even with moderate blockages. For example, someone with a 60% blockage but frequent angina might get a stent to improve their life quality.
The blockage’s location and complexity are very important. Blockages in critical areas, like the left main coronary artery, or complex lesions often require stenting. The blockage’s length and shape also affect the decision.
A patient’s heart function, measured by the ejection fraction (EF), is also key. Patients with low EF might get stents to boost heart function and lower cardiac event risks.
A patient’s medical history and risk factors, like diabetes, hypertension, and hyperlipidemia, are considered too. These can affect stenting success and overall heart health risk.
In conclusion, choosing to place a stent involves looking at many factors, not just blockage percentages. Understanding these factors helps doctors make better decisions for their patients.
Cardiologists use several tests to find out how bad artery blockages are. These tests are key in deciding the best treatment, like if a stent is needed.
A coronary angiogram is a test done by a cardiologist to see if heart arteries have blockages. A special dye is injected into the arteries, and X-ray images show them. This test shows where and how bad the blockages are.
Key benefits of coronary angiogram:
Fractional Flow Reserve (FFR) is a method used during angiography to check blockage severity. It measures pressure differences across blockages to see if blood flow is blocked. An FFR value of 0.8 or less means a blockage is serious.
Techniques like Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT) give detailed views of artery walls and plaque. These help doctors understand blockage complexity and plan the best treatment.
Benefits of IVUS and OCT:
It’s important to know about the different stents for treating artery blockages. The right stent can greatly improve a patient’s life after the procedure.
Stent technology has evolved, leading to various types. Each has its own benefits and drawbacks. These include bare metal stents, drug-eluting stents, and bioabsorbable stents.
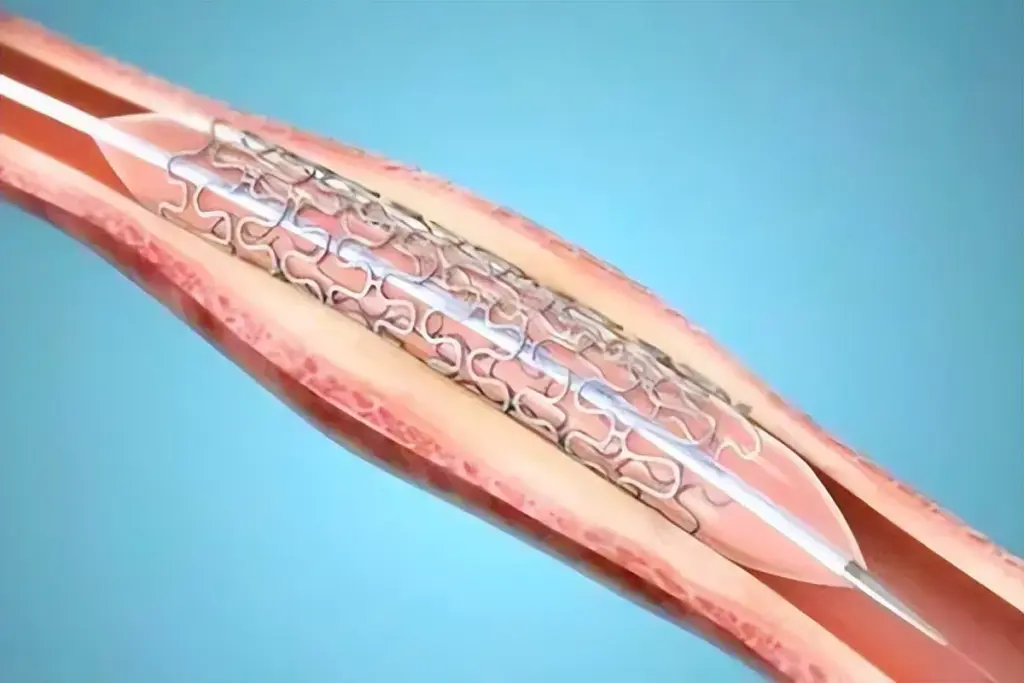
Bare metal stents are the first type made from metal mesh. They work well but might cause the artery to narrow again. They’re used for simple blockages and when the patient is at low risk for problems.
Drug-eluting stents release medicine to prevent the artery from narrowing. They’re great for complex blockages and are often the first choice. The medicine they release lowers the chance of the artery narrowing again.
Bioabsorbable stents, or bioresorbable scaffolds, dissolve over time. They leave no permanent implant. This technology aims to make the artery natural again, reducing long-term issues with metal stents.
Each stent type is suited for different needs. Doctors choose the best stent based on the blockage’s severity, the patient’s history, and overall health.
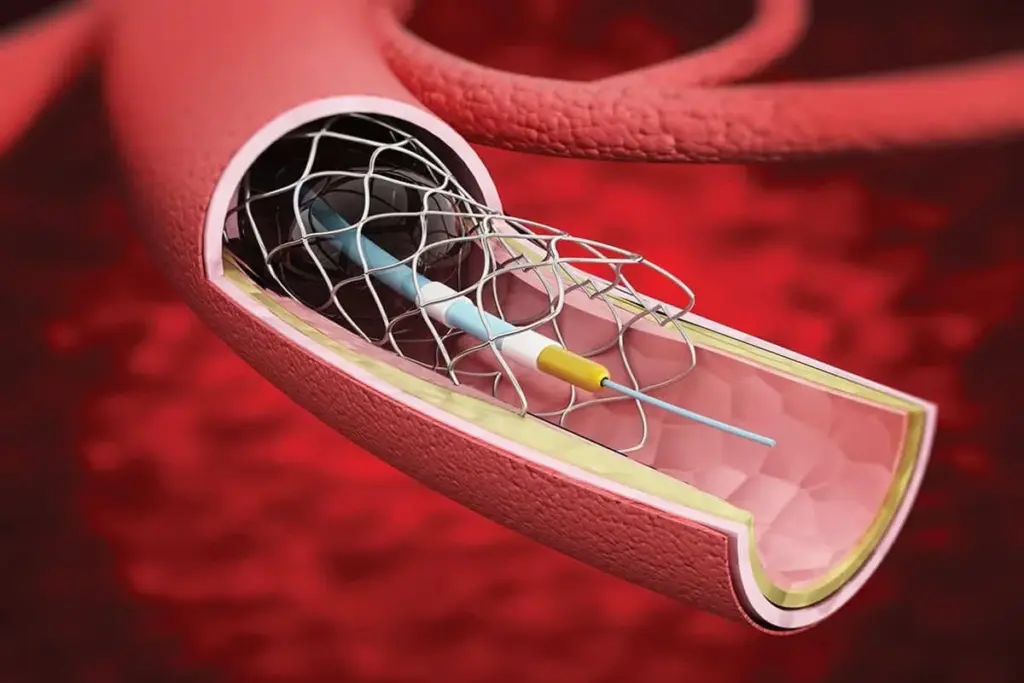
The stent placement process has several key steps to fix artery blockage. It’s a minimally invasive method to open blocked or narrowed coronary arteries. This helps improve blood flow to the heart.
Before stent placement, patients get a detailed check-up. This includes looking at their medical history, symptoms, and test results. They might need to stop certain medicines and fast beforehand. The team will also talk about the procedure’s risks and benefits.
During the procedure, the patient gets local anesthesia. This numbs the area where the catheter goes in, usually in the groin or arm. Angioplasty uses a balloon to push plaque against the artery walls. Then, a stent is put in to keep the artery open. The stent is a small, mesh-like tube that stays in the artery to support it and improve blood flow.
After the procedure, patients are watched in a recovery area for a few hours. They’re told to rest and avoid hard activities for a bit. The team will also give them medicine to prevent clots around the stent. It’s important to follow up to make sure the stent works well and to watch for any problems.
The stent placement procedure is a very effective way to treat artery blockage. It offers big benefits for people with coronary artery disease.
After getting a stent, you need to follow a treatment plan and make lifestyle changes. This helps the stent work right and stops new blockages.
Patients usually take dual antiplatelet therapy (DAPT) after a stent. This means taking two medicines to stop blood clots on the stent. How long you take DAPT depends on the stent type and your health risks.
Seeing a cardiologist regularly is key after a stent. They check for symptoms and complications. They might also do tests to see how the stent and arteries are doing.
Changing your lifestyle is important to avoid more blockages. Eating a heart-healthy diet, exercising, quitting smoking, and managing stress are key. These steps can lower your chance of heart problems.
|
Lifestyle Change |
Benefit |
|---|---|
|
Adopting a heart-healthy diet |
Reduces risk of further blockages |
|
Regular physical activity |
Improves cardiovascular health |
|
Quitting smoking |
Significantly reduces cardiovascular risk |
It’s important for patients to know the risks and benefits of stent placement. This procedure helps treat coronary artery disease by opening blocked arteries. It allows blood to flow freely again.
Stenting can greatly help those with severe blockages (>70%). It can lessen symptoms and lower the risk of heart attacks. Restoring blood flow also boosts heart function and improves life quality.
Research shows stenting can reduce angina symptoms and improve how well you can exercise.
Stenting is usually safe, but there are risks. These include infection, bleeding, and the artery getting narrow again. These risks depend on the blockage’s severity, the patient’s health, and other medical conditions.
Stent placement outcomes vary with blockage severity. Those with severe blockages need closer monitoring and aggressive risk factor management. Following dual antiplatelet therapy and making lifestyle changes are key for the best long-term results.
In summary, choosing stent placement should consider the blockage’s severity and the patient’s health. It’s a decision that needs careful thought.
Knowing the right blockage percentage for stent placement is key in treating coronary artery disease. Stents are important tools that help open blocked arteries. This improves blood flow and patient health.
Doctors decide on stent placement based on several things. These include the blockage’s size, how bad the symptoms are, and where the blockage is. They also look at the patient’s heart health and medical history.
Tests like coronary angiograms and advanced imaging are very important. They help doctors choose the best treatment. This way, they can improve patient care and quality of life.
A coronary angiogram is a key test for finding out if a stent is needed. Understanding stents and how they are used helps patients make informed choices. It’s a step towards better heart health.
The need for a stent depends on several factors. These include the blockage’s location and how severe it is. Also, how well the heart is working plays a role. Generally, a blockage over 70% might need a stent.
A blockage is considered severe if it’s over 70%. In such cases, a stent is often recommended. It helps restore blood flow and lowers the risk of heart attack.
Yes, there are various stents available. These include bare metal stents, drug-eluting stents, and bioabsorbable stents. The right stent depends on the blockage’s level, complexity, and the patient’s health.
Tests like coronary angiograms and fractional flow reserve (FFR) measurements help assess blockage severity. Advanced imaging techniques, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), also play a role.
Decisions on stent placement consider more than just blockage percentage. Factors include symptom severity, blockage complexity, heart function, and patient medical history.
The procedure starts with preparation and assessment. Then, angioplasty and stent deployment happen. After, there’s immediate recovery and monitoring.
Post-stent placement, patients need dual antiplatelet therapy. They also require follow-up care and lifestyle changes to avoid further blockages.
Stent placement benefits include restoring blood flow and lowering heart attack risk. Risks include bleeding, clotting, and restenosis.
The left main coronary artery is vital for heart muscle supply. Blockages here are high-risk. They often require stent placement or other interventions.
After stent placement, patients should make lifestyle changes. These include dietary adjustments, exercise, quitting smoking, and stress reduction. These help prevent further blockages and keep the heart healthy.
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamacardiology/fullarticle/2775374
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!