Last Updated on November 26, 2025 by Bilal Hasdemir

Endovascular Aortic Aneurysm Repair (EVAR) is a new, less invasive technique that has transformed the treatment of abdominal aortic aneurysms (AAA).
At Liv Hospital, we specialize in the EVAR surgery procedure, using the latest technology to offer patients a safer alternative to traditional open surgery. Our experienced team is dedicated to providing top-notch care and achieving the best possible outcomes.
During the EVAR surgery procedure, a stent-graft is placed inside the aorta to block blood flow to the aneurysm. This significantly reduces the risk of rupture and enhances overall patient health.
Key Takeaways
- EVAR is a minimally invasive treatment for abdominal aortic aneurysms.
- Liv Hospital offers advanced EVAR procedures with exceptional patient care.
- The EVAR procedure involves stent-graft placement to exclude the aneurysm.
- Reduced risk of rupture and improved patient outcomes are associated with EVAR.
- Our experienced team is dedicated to delivering the best possible results.
Understanding Endovascular Aortic Aneurysm Repair (EVAR)
The EVAR procedure has changed how we treat abdominal aortic aneurysms. It’s a less invasive option compared to open surgery. Let’s look into what EVAR is, its history, and why it’s better than traditional surgery.
Definition and Medical Significance of EVAR
EVAR is a minimally invasive way to treat abdominal aortic aneurysms (AAA). It involves placing a stent-graft in the aorta. This method has made treating AAA safer, reducing the risks of open surgery.
EVAR is very important for patients at high risk for open surgery or with complex anatomy. It offers a safer option with fewer complications.
Historical Development of the EVAR Technique
The idea of EVAR started in the 1990s, changing how we treat AAA. Over time, stent-graft technology and imaging have improved a lot. These advancements have made EVAR suitable for more patients, even those with complex aortic anatomy.
Continuous innovation in EVAR technology has made it safer and more effective.
Advantages Over Traditional Open Surgical Repair
EVAR is less invasive than open surgery, leading to less pain and shorter hospital stays. It also has lower risks during and after surgery. This makes EVAR a great choice for patients who can’t have open surgery.
The minimally invasive nature of EVAR means patients can recover faster. They can get back to their daily activities sooner. EVAR also avoids big incisions, reducing tissue damage and preserving the abdominal wall.
Exploring EVAR shows it’s a big step forward in treating abdominal aortic aneurysms. Knowing what EVAR is, its history, and its benefits helps us see its importance in vascular surgery today.
Abdominal Aortic Aneurysms (AAA): Pathophysiology and Risk Assessment
Understanding abdominal aortic aneurysms (AAA) is key to knowing the risk of rupture and the right treatment. AAA is when the main blood vessel in the abdomen and legs gets too big.
Etiology and Natural History of AAA
The growth of AAA involves complex processes. Inflammation and degradation of the aortic wall play big roles. The aneurysm gets bigger over time, which can lead to rupture if not treated.
Many things can cause AAA, like genetics, smoking, high blood pressure, and atherosclerosis. Knowing these can help find who’s at risk.
Risk Factors for Aneurysm Rupture
Knowing the risk of rupture is key to deciding if treatment is needed. Diameter is a big factor; aneurysms over 5.5 cm are at high risk. Other factors include how fast it’s growing, if you smoke, and if you have symptoms.
| Risk Factor | Description | Impact on Rupture Risk |
| Diameter | Aneurysm size | Higher risk if >5.5 cm |
| Rate of Expansion | Rate at which the aneurysm grows | Increased risk with rapid expansion |
| Smoking Status | Current smoking | Increases rupture risk |
| Symptoms | Presence of pain or tenderness | Indicates higher risk |
Indications for Intervention
Deciding to intervene depends on the risk of rupture versus the risks of the repair. Endovascular aneurysm repair (EVAR) is a less invasive option for those with the right anatomy. Interventions are needed for symptomatic aneurysms, fast growth, and sizes over the threshold.
We look at many things when deciding on intervention. This includes the patient’s health, the aneurysm’s details, and the procedure’s benefits and risks.
Patient Selection Criteria for EVAR Surgery Procedure
The success of EVAR surgery depends a lot on choosing the right patients. We look at many factors to see if EVAR is the best choice for each patient. This careful selection is key to a good outcome.
Anatomical Considerations and Contraindications
How well the patient’s body fits the EVAR procedure is very important. We check the size and shape of the aneurysm. We also look at the health of the neck and iliac arteries.
- Aneurysm Size and Shape: The size and shape of the aneurysm are key to deciding if EVAR is right.
- Neck Anatomy: The shape and size of the aortic neck are important for choosing and placing the stent-graft.
- Iliac Artery Disease: Any disease in the iliac arteries can affect if EVAR is possible and what stent-graft to use.
Comorbidity Assessment
Other health issues can also affect how well a patient does after EVAR surgery. We look at the patient’s medical history. This includes heart disease, diabetes, and COPD.
- Cardiac Evaluation: Checking the heart’s function is important to see if the patient is at risk for surgery.
- Pulmonary Function: We check how well the lungs work to see if the patient can handle the procedure.
- Renal Function: Kidney problems are important because they affect imaging choices and the patient’s risk.
Risk-Benefit Analysis: EVAR vs. Open Repair
We compare EVAR with open surgery for each patient. We look at the benefits of EVAR, like less risk of complications. But we also consider the risks, like endoleaks and the need for ongoing checks.
- Short-term Risks: EVAR usually has fewer risks in the short term than open surgery, like less chance of serious problems.
- Long-term Considerations: The long-term success of EVAR and the chance of needing more surgery are important in making a decision.
By carefully thinking about these factors, we can choose the best treatment for each patient. This ensures they get the best care possible.
Pre-Operative Planning and Imaging
For a successful EVAR procedure, thorough pre-operative planning is key. This phase is vital to ensure the stent-graft fits right. It also makes sure the procedure matches the patient’s unique anatomy.
CT Angiography Protocol
CT angiography is a main part of pre-operative planning for EVAR aortic aneurysm repair. It gives detailed images of the aorta and its branches. This helps us get precise measurements.
We follow a specific CT angiography protocol. It includes:
- Thin-slice imaging for detailed anatomy
- Contrast enhancement to see the lumen and wall of the aorta
- Image acquisition from the celiac trunk to the common femoral arteries
This protocol helps us check the aneurysm’s shape, the aortic wall’s quality, and any accessory renal arteries.
3D Reconstruction and Measurements
After getting CT angiography images, we do 3D reconstruction. This helps us understand the patient’s anatomy better. The process involves:
- Segmenting the aorta and its branches from the surrounding structures
- Creating a 3D model to see the aneurysm and its relation to nearby vessels
- Taking precise measurements of the aortic neck, aneurysm sac, and iliac arteries
These measurements are key for picking the right stent-graft size and shape.
Stent-Graft Selection and Sizing
The last step in pre-operative planning is stent-graft selection and sizing. We choose a stent-graft based on the 3D reconstruction measurements. It should:
- Match the patient’s anatomy
- Have enough sealing zones
- Ensure proper fixation to prevent migration
By carefully planning the EVAR procedure, we can lower the risk of complications. This detailed approach makes EVAR for aneurysm a reliable and effective treatment.
Operating Room Setup for EVAR Vascular Procedure
An efficiently organized operating room is key for EVAR vascular surgery success. It needs the right equipment and a well-coordinated team.
Equipment and Imaging Requirements
The EVAR procedure requires top-notch imaging for precise stent-graft deployment. We use a fixed imaging system or a high-quality mobile C-arm fluoroscopy unit. The imaging gear must produce clear images and support features like roadmapping and subtraction angiography.
Key Equipment:
- Fluoroscopy unit
- Ultrasound machine
- Angiography catheters and guidewires
- Stent-grafts and delivery systems
| Equipment | Purpose |
| Fluoroscopy Unit | Real-time imaging during the procedure |
| Ultrasound Machine | Assessing vascular access and possible complications |
| Angiography Catheters and Guidewires | Navigation and deployment of stent-graft |
Team Composition and Responsibilities
A multidisciplinary team is essential for EVAR success. It includes vascular surgeons, interventional radiologists, anesthesiologists, and specialized nursing staff. Each team member has specific duties, from patient preparation to managing imaging equipment.
Team Roles:
- Vascular Surgeon: Performs the EVAR procedure
- Interventional Radiologist: Assists with imaging and stent-graft deployment
- Anesthesiologist: Manages patient anesthesia and vital signs
- Nursing Staff: Assists with patient care and equipment preparation
Patient Positioning and Preparation
Proper patient positioning is vital for EVAR success. Patients are placed in a supine position on a radiolucent table for fluoroscopic imaging. Preparation includes sterile draping and the right anesthesia.
Preparation Steps:
- Patient is positioned on a radiolucent table
- Sterile draping is performed
- Anesthesia is administered as necessary
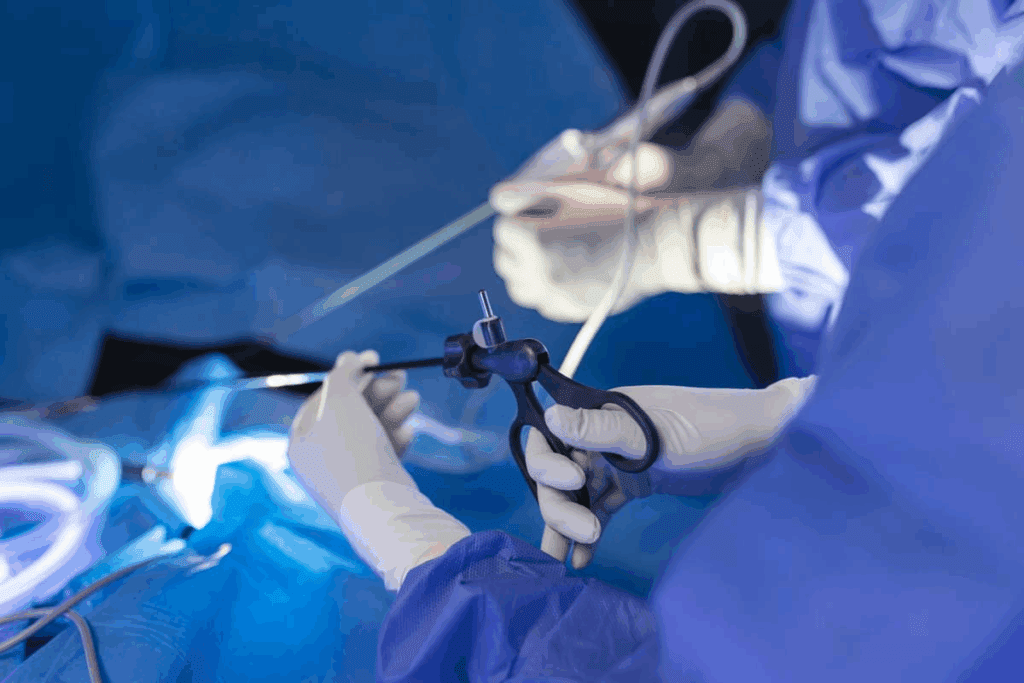
Step-by-Step EVAR Surgery Procedure
Performing EVAR surgery needs careful planning and skill. It’s a complex procedure with many important steps. Each step requires precision and expertise.
Anesthesia Considerations
The type of anesthesia for EVAR is key. It depends on the patient’s health and the aneurysm’s details. General anesthesia is common, but local anesthesia with sedation might be used in some cases. We choose the best anesthesia based on the patient’s condition.
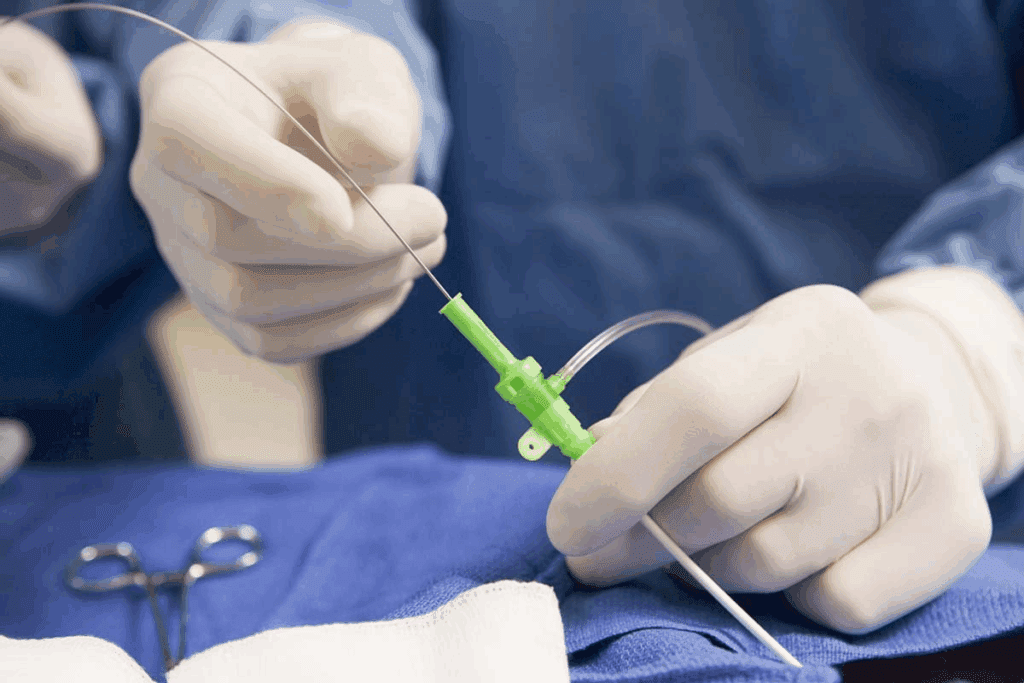
Vascular Access Techniques
Getting vascular access is a critical step. We usually use the femoral arteries. This can be done through a surgical cutdown or a percutaneous approach. The choice depends on the patient’s anatomy and the surgeon’s preference.
| Access Method | Description | Advantages |
| Surgical Cutdown | Direct exposure of the femoral artery | Control and direct access |
| Percutaneous Access | Minimally invasive, using a needle and wire | Less invasive, quicker recovery |
Guidewire and Catheter Navigation
After gaining access, we guide guidewires and catheters to the aneurysm. This step needs precise fluoroscopic guidance and knowledge of the patient’s anatomy. We use different catheters and guidewires, sometimes with roadmapping to help navigate.
Main Body Deployment
Deploying the stent-graft’s main body is a key moment. We place it carefully, making sure it’s right near the renal arteries and the aneurysm. Angiographic confirmation checks its position before we deploy it fully.
By following these steps and using advanced imaging and navigation, we can successfully do EVAR surgery. This offers patients a less invasive way to treat abdominal aortic aneurysms.
Managing Complex Anatomies and Variants
Success in EVAR procedures depends on handling complex anatomies. This includes dealing with tough necks, twisted iliac arteries, and extra renal arteries. Special techniques and plans are needed for these challenges.
Hostile Neck Anatomy Approaches
Dealing with tough necks in EVAR is a big challenge. We use suprenal stent-grafts and endovascular aneurysm sealing systems. These methods help seal the area well and prevent leaks.
Techniques for Iliac Tortuosity
Iliac twists make it hard to place stent-grafts in EVAR. We plan ahead with 3D models to tackle these twists. Using iliac artery straightening and stiff guidewires helps us place the stent-grafts correctly.
Accessory Renal Artery Management
Extra renal arteries can make EVAR tricky. We figure out if these arteries matter and use coil embolization or fenestrated stent-grafts to handle them. This balances keeping the kidneys working with the EVAR goals.
Hypogastric Artery Preservation Strategies
Keeping the hypogastric artery safe is key to avoid problems like buttock pain. We use iliac branch devices to keep blood flowing to this artery. This helps avoid ischemic issues and keeps the pelvic area well-perfused.
| Anatomical Challenge | Management Strategy | Benefits |
| Hostile Neck Anatomy | Suprenal stent-grafts, Endovascular aneurysm sealing | Secure seal, Reduced endoleak risk |
| Iliac Tortuosity | Preoperative 3D planning, Iliac artery straightening | Facilitated stent-graft deployment, Reduced complication risk |
| Accessory Renal Arteries | Coil embolization, Fenestrated stent-grafts | Preserved renal function, Effective aneurysm exclusion |
| Hypogastric Artery Preservation | Iliac branch devices | Maintained pelvic perfusion, Minimized ischemic risk |
Intraoperative Complications and Troubleshooting
EVAR surgery’s success depends on handling intraoperative complications well. Even with new tech and methods, problems can pop up. We need to spot and fix them fast.
Endoleaks: Identification and Management
Endoleaks are a big issue in EVAR. They happen when blood keeps flowing outside the stent-graft but inside the aneurysm sac. We divide endoleaks into five types, with Type I and Type III being the most serious because they can lead to rupture.
To tackle endoleaks, we use different approaches. These include adding more stent-grafts, using balloons, or embolization. The right treatment depends on the endoleak’s type and cause.
| Endoleak Type | Cause | Management Strategy |
| Type I | Inadequate seal at graft ends | Additional stent-grafting or ballooning |
| Type II | Retrograde flow from branch vessels | Embolization or observation |
| Type III | Graft defect or modular disconnection | Additional stent-grafting |
Access Site Complications
Problems at the access site, like bleeding or hematoma, can happen during EVAR. We reduce these risks by careful planning before surgery and choosing the right access methods.
When these issues come up, we use both surgery and endovascular methods. This includes using closure devices or stent-grafts to stop bleeding.
Deployment System Failures
Though rare, deployment system failures can be serious. We avoid these by carefully picking and preparing the devices.
If a failure happens, we have plans to fix it. This includes using other devices or switching to open repair.
Conversion to Open Repair: Indications and Technique
Open repair is considered when EVAR doesn’t work or complications can’t be fixed with endovascular methods. This includes big endoleaks, graft migration, or rupture.
Open repair involves a laparotomy, aortic clamping, and replacing the graft. We’re ready for this by having a detailed plan, including getting patient consent and making sure the surgical team is ready.
In summary, dealing with complications during EVAR needs preparation, skill, and smart decisions. Knowing the possible problems and having good solutions helps us improve results for patients having EVAR surgery.
Post-Operative Care and Follow-Up Protocol
EVAR surgery needs a detailed care plan for the best results. Good care after the surgery is key to avoid problems and help patients recover well.
Immediate Post-Operative Management
Right after EVAR surgery, patients are watched closely in the recovery unit. They look for signs like bleeding or endoleaks. It’s important to catch any issues early.
Key parts of early care include:
- Watching vital signs and brain function
- Keeping pain under control
- Looking for signs of endoleaks or other problems
Discharge Planning and Patient Education
Before leaving the hospital, patients learn a lot about caring for themselves. They learn about wound care, taking medicine, and when to come back for check-ups. It’s vital to follow these steps to avoid problems.
Discharge planning covers:
- Going over medicine and possible side effects
- Telling patients what activities they can and can’t do
- Setting up check-up times for imaging tests
Surveillance Imaging Schedule
Regular imaging tests are key to check if EVAR is working and to catch problems early. We suggest CT angiography at 1, 6, and 12 months after surgery, and then every year.
Imaging helps in:
- Finding endoleaks or graft movement
- Watching the size of the aneurysm sac
- Spotting problems early
Long-Term Follow-Up Considerations
Keeping up with follow-up care after EVAR is vital. It helps manage the patient’s condition and catch any late problems. We stress the need for ongoing monitoring to make sure the repair lasts.
Long-term care includes:
- Regular imaging tests
- Managing other health issues
- Acting fast if new problems arise
Conclusion: Outcomes and Future Directions in EVAR for Abdominal Aortic Aneurysms
EVAR has made big strides in treating abdominal aortic aneurysms (AAA). This method is now favored for its less invasive approach and good results. We’re working to make EVAR even better by improving how we choose patients and the success of the procedure.
EVAR has cut down on recovery time and lowered risks compared to open surgery. New research and tech are on the horizon to make EVAR even better. This will help more patients and improve their care.
Looking ahead, new stent-graft designs and better imaging will be key. These advancements will shape the future of EVAR. We expect to see better treatments for AAA, leading to better lives for patients.
The growth of EVAR technology and practice is vital for tackling AAA’s challenges. It shows how important EVAR is in today’s vascular surgery.
FAQ
What is EVAR surgery?
EVAR (Endovascular Aortic Aneurysm Repair) is a new way to fix a big bulge in the main artery. It’s done by putting a special mesh through the blood vessels. This mesh keeps the bulge from getting worse and bursting.
What are the benefits of EVAR over traditional open surgery?
EVAR is better because it uses smaller cuts and less blood loss. It also lowers the chance of serious problems. Patients usually stay in the hospital less time and heal faster than with open surgery.
How is patient selection done for EVAR surgery?
Doctors pick the right patients for EVAR by looking at their body and health. They weigh the risks and benefits to decide if EVAR or open surgery is best.
What imaging is required for pre-operative planning in EVAR?
Doctors use CT scans to plan EVAR. They make 3D pictures of the aorta to pick the right size and shape of the mesh.
What are the possible complications during EVAR?
EVAR can have problems like leaks, issues at the entry point, and mesh failures. Sometimes, it needs to turn into open surgery. Handling these issues is key to success.
What is the follow-up protocol after EVAR?
After EVAR, patients get close care and learn about their recovery. They have regular check-ups and scans to watch for any new problems. This helps make sure the repair works well over time.
How does EVAR manage complex aortic anatomies?
EVAR can handle tricky aortic shapes by using special techniques. It deals with hard-to-reach areas and keeps important arteries open. This means more people can get this treatment.
What is the significance of EVAR in treating abdominal aortic aneurysms?
EVAR has changed how we treat big artery bulges. It’s a safer option than open surgery, leading to better results and fewer deaths.
What advancements can be expected in EVAR technology and practice?
EVAR will keep getting better with new mesh designs and better imaging. These improvements will help more people and make the treatment even safer and more effective.
References:
- Kim, H. O. (2019). Endovascular aneurysm repair for abdominal aortic aneurysm. Korean Journal of Thoracic and Cardiovascular Surgery, 52(1), 1-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6658877/