Endovascular thrombectomy (EVT) is a revolutionary procedure for treating acute ischemic stroke by removing blood clots from blocked arteries in the brain. When it comes to EVT meaning medical, it refers to a minimally invasive technique that restores blood flow to the brain quickly and effectively.
This advanced procedure has shown significant promise in improving patient outcomes and reducing mortality rates. Recent studies have highlighted the benefits of EVT, making it a crucial treatment option for stroke patients.
At Liv Hospital, we are at the forefront of delivering innovative stroke treatments, guided by patient-centered values and global standards. Our expertise in EVT is transforming the landscape of stroke care. By understanding EVT meaning medical and its role in treating acute ischemic stroke, patients and healthcare providers can make informed decisions about the best course of treatment.
Key Takeaways
- Endovascular thrombectomy is a minimally invasive procedure for treating acute ischemic stroke.
- EVT improves functional outcomes and reduces mortality rates in stroke patients.
- Liv Hospital leads in delivering innovative EVT treatments guided by global standards.
- Understanding EVT is crucial for making informed decisions about stroke treatment.
- Recent studies have shown the benefits of EVT in stroke care.
EVT Meaning in Medical Terms: Decoding the Abbreviation
Decoding the EVT abbreviation reveals its significance in treating acute ischemic stroke. EVT stands for Endovascular Thrombectomy, a medical procedure used to remove blood clots from the brain’s blood vessels.
Definition and Full Terminology
Endovascular Thrombectomy, also referred to as cerebral thrombectomy or thrombectomy for stroke, is a minimally invasive procedure. It involves using a catheter to reach the occluded blood vessel and retrieve or remove the clot.
Key aspects of EVT include:
- Minimally invasive technique
- Use of catheters and clot retrieval devices
- Application in acute ischemic stroke treatment
Historical Development of EVT as a Medical Procedure
The historical development of EVT as a medical procedure has evolved significantly over the years. Initially, stroke treatment was limited to intravenous thrombolysis. However, with advancements in technology and technique, EVT has become a critical component of stroke care.
| Year | Milestone |
| 1990s | Introduction of first thrombectomy devices |
| 2010s | Advancements in stent retriever technology |
| 2015 | Multiple positive randomized controlled trials for EVT |
The evolution of EVT has transformed stroke treatment, offering new hope to patients with large vessel occlusions. As medical technology continues to advance, the procedure is likely to become even more effective and accessible.
Key Fact #1: How Endovascular Thrombectomy Treats Ischemic Stroke
Ischemic stroke treatment has been revolutionized by EVT, a procedure that directly addresses the cause of the stroke by removing blood clots from occluded arteries. This method has shown significant promise in restoring blood flow and reducing the risk of long-term disability.
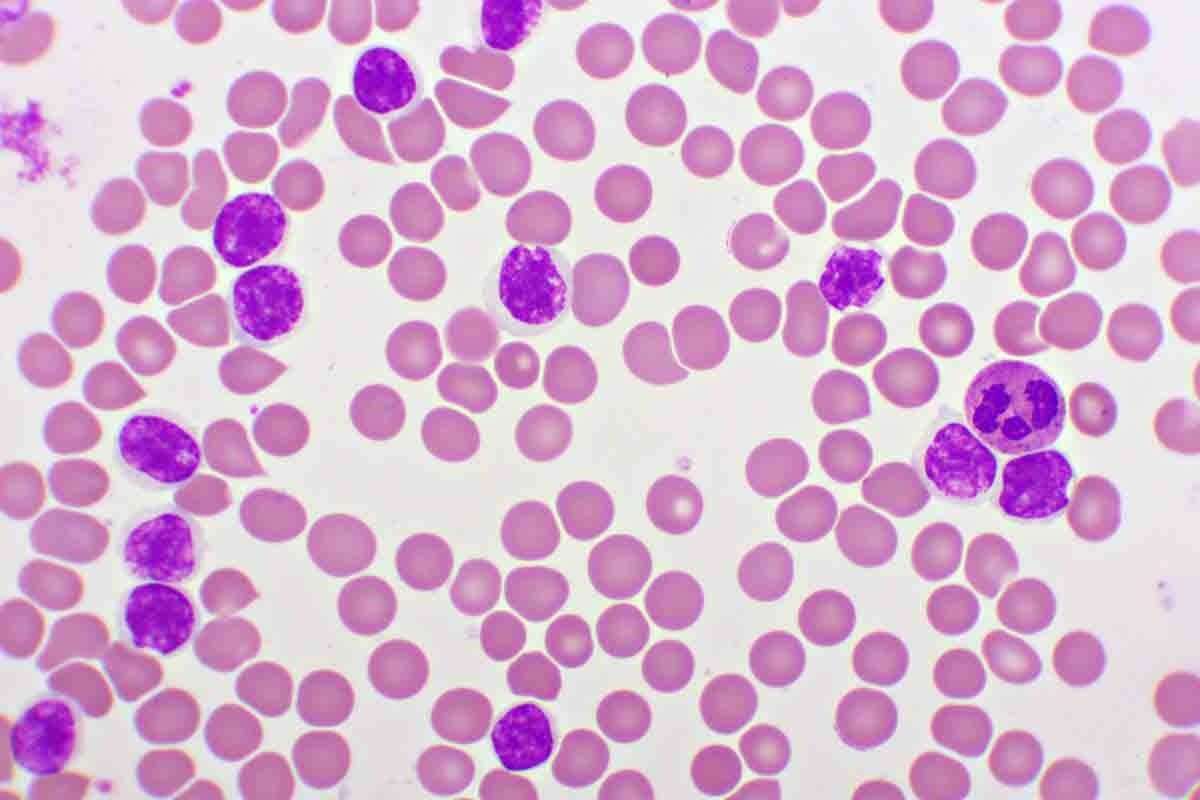
The Mechanism of Acute Ischemic Stroke
Acute ischemic stroke occurs when a blood clot obstructs a major artery in the brain, cutting off blood flow and oxygen supply to a specific area. This obstruction leads to cellular damage and can result in significant neurological deficits. The severity of the stroke is often correlated with the size and location of the occlusion.
“The timely restoration of blood flow is critical in minimizing brain damage,” as emphasized by recent studies on stroke management. Effective treatment strategies focus on quickly re-establishing normal blood circulation.
How EVT Addresses Blood Clot Blockages
EVT is a minimally invasive procedure that involves navigating a catheter through the vascular system to the site of the occlusion in the brain. Once in place, various techniques and devices can be employed to retrieve the clot, thus restoring blood flow. The success of EVT is largely dependent on the promptness of the intervention and the skill of the medical team.
Studies have shown that EVT improves functional outcomes and reduces mortality rates in patients with acute ischemic stroke. By mechanically removing the occluding clot, EVT can significantly enhance the chances of recovery for stroke patients.
The benefits of EVT are multifaceted, including reduced long-term disability and improved quality of life for patients. As medical technology continues to evolve, the role of EVT in stroke management is likely to expand, offering new possibilities for effective treatment.
Key Fact #2: The Step-by-Step EVT Procedure Process
Understanding the EVT procedure requires a breakdown of its multiple stages, from preparation to clot retrieval. The process involves a series of precise steps that are crucial for the effective treatment of ischemic stroke.
Pre-Procedure Preparation and Imaging
Before the EVT procedure begins, thorough preparation and imaging are essential. This includes:
- Conducting CT or MRI scans to assess the extent of the stroke and identify the location of the clot.
- Reviewing the patient’s medical history to identify any potential contraindications.
- Administering conscious sedation to ensure patient comfort during the procedure.
Catheter Insertion Through the Groin
The EVT procedure starts with the insertion of a catheter into the femoral artery in the groin. This step is critical as it provides access to the cerebral arteries.
Key steps include:
- Administering local anesthesia to minimize discomfort.
- Inserting a guidewire and catheter under fluoroscopic guidance.
Navigation to the Brain Arteries
Once the catheter is in place, it is navigated through the arterial system to the brain arteries. This requires:
- Using advanced imaging techniques to guide the catheter.
- Maneuvering through the arteries with precision to reach the occluded segment.
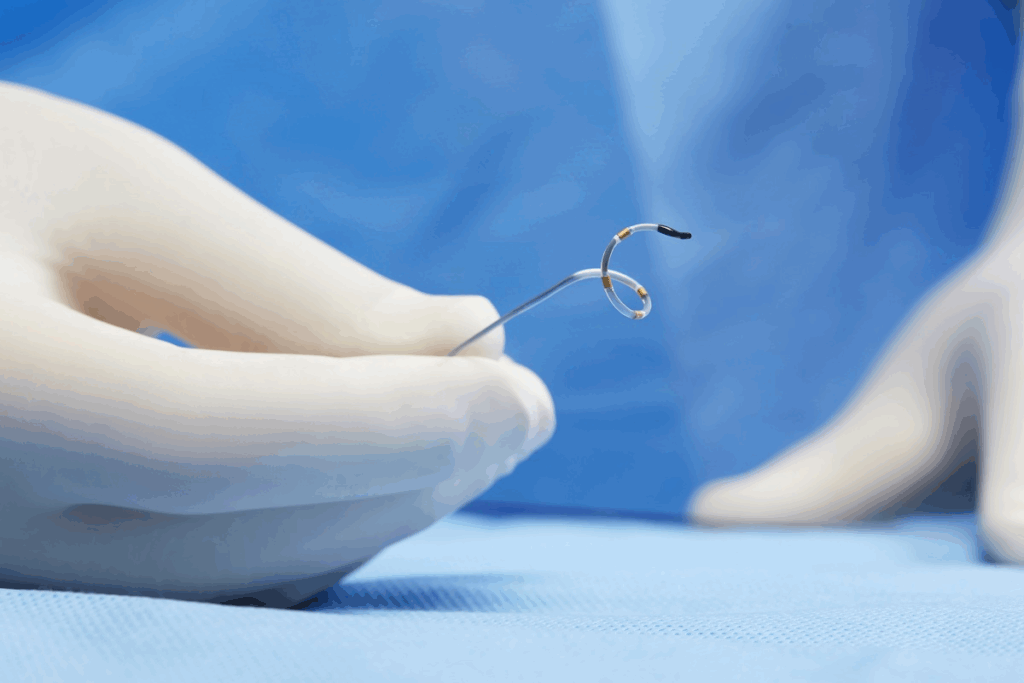
Clot Retrieval Techniques and Device Types
The final step involves retrieving the clot using specialized devices. Common techniques include:
- Stent retriever devices that capture the clot.
- Aspiration catheters that suction out the clot.
The choice of device depends on various factors, including the clot’s location and size.
Key Fact #3: Patient Selection Criteria for EVT
The effectiveness of EVT for stroke thrombectomy is significantly influenced by the careful selection of appropriate patients. EVT is a critical treatment for ischemic stroke, particularly for those with large vessel occlusions.
Large Vessel Occlusion Requirements
Patients eligible for EVT often present with large vessel occlusions, which are blockages in major arteries supplying blood to the brain. These occlusions are associated with severe strokes and poor outcomes if not promptly treated.
Large vessel occlusions are typically identified in the internal carotid artery or the M1 segment of the middle cerebral artery. The presence of such occlusions is a key factor in determining the suitability of EVT.
Neuroimaging Assessment Protocols
Neuroimaging plays a crucial role in patient selection for EVT. Advanced imaging techniques such as CT angiography (CTA) and MRI angiography (MRA) help identify large vessel occlusions and assess the extent of brain tissue at risk.
These imaging protocols provide essential information on the location and severity of the occlusion, guiding clinicians in their decision-making process.
| Imaging Modality | Information Provided | Clinical Utility |
| CT Angiography (CTA) | Detailed images of arterial anatomy, occlusion location | Identifies large vessel occlusions, guides EVT |
| MRI Angiography (MRA) | Assesses cerebral blood flow, tissue perfusion | Helps evaluate extent of ischemic damage |
Contraindications and Risk Evaluation
While EVT is a highly effective treatment, there are certain contraindications and risks that need to be evaluated. These include factors such as the patient’s overall health, the presence of other medical conditions, and the time elapsed since stroke onset.
A thorough risk assessment is necessary to determine the potential benefits and risks of EVT for each patient, ensuring that the treatment is tailored to their individual needs.
Key Fact #4: The Critical Time Window for Effective Treatment
In the management of acute ischemic stroke, the timing of EVT is a critical factor that determines patient outcomes. The procedure’s effectiveness is closely linked to how quickly it is performed after the onset of stroke symptoms.
Standard 6-8 Hour Treatment Window
The standard time window for EVT in treating ischemic stroke is generally considered to be within 6 to 8 hours from the onset of symptoms. Timely treatment within this window has been shown to significantly improve patient outcomes by restoring blood flow to the affected area of the brain. Studies have consistently demonstrated that patients treated within this timeframe have better chances of recovery and reduced risk of long-term disability.
Extended Time Windows for Select Patients
Recent research has indicated that select patients may benefit from EVT even when treated beyond the standard 6-8 hour window. Advanced neuroimaging techniques play a crucial role in identifying these patients by assessing the extent of brain tissue salvageability. According to a study published on PMC, certain patients with a favorable imaging profile may benefit from EVT up to 24 hours after stroke onset.
Impact of Treatment Delays on Outcomes
Delays in EVT treatment can have a profound impact on patient outcomes. Every minute counts in stroke treatment, as delayed treatment results in additional brain tissue damage due to prolonged ischemia. The importance of streamlined protocols and rapid patient assessment cannot be overstated in minimizing delays and optimizing the chances of a successful outcome. Efficient systems that facilitate quick decision-making and procedure initiation are essential in the effective management of stroke patients.
In conclusion, while the standard treatment window for EVT is 6-8 hours, the potential for extended windows in select patients highlights the need for individualized assessment and timely intervention. The impact of treatment delays underscores the importance of efficient stroke management systems.
Key Fact #5: EVT vs. Traditional Stroke Treatments
EVT has been shown to improve outcomes in patients with acute ischemic stroke, particularly those with large vessel occlusions, compared to traditional intravenous thrombolysis alone. This section compares EVT with traditional stroke treatments, highlighting the limitations of conventional methods and the benefits of EVT.
Limitations of Intravenous Thrombolysis Alone
Intravenous thrombolysis, typically administered with tissue plasminogen activator (tPA), has been the standard treatment for acute ischemic stroke. However, it has several limitations, including:
- A narrow therapeutic window, typically within 4.5 hours of stroke onset
- Reduced efficacy in patients with large vessel occlusions
- Risk of bleeding complications
These limitations underscore the need for alternative or complementary treatments like EVT.
Clinical Evidence Supporting EVT Superiority
Numerous clinical trials have demonstrated the superiority of EVT over intravenous thrombolysis alone in treating acute ischemic stroke, particularly in patients with large vessel occlusions. A study published on PMC highlights the benefits of EVT in improving patient outcomes.
The clinical evidence supporting EVT includes:
- Improved functional outcomes at 90 days post-stroke
- Higher rates of successful reperfusion
- Better outcomes in patients with large vessel occlusions
Combined Treatment Approaches
In many cases, EVT is used in conjunction with intravenous thrombolysis. The combination of these treatments can offer the best possible outcomes for patients. Combined treatment approaches may enhance the efficacy of stroke treatment by leveraging the strengths of both EVT and intravenous thrombolysis.
The benefits of combined treatment include:
- Rapid initiation of treatment with tPA while preparing for EVT
- Potential for improved outcomes through the synergistic effects of both treatments
Key Fact #6: Procedure Duration and Recovery Timeline
The EVT procedure, while critical for stroke treatment, varies in duration and has a specific recovery process. Understanding these aspects is vital for both patients and healthcare providers to manage expectations and optimize care.
Average Procedure Length of 1-2 Hours
Most EVT procedures typically last between 1 to 2 hours. The duration can vary based on factors such as the complexity of the occlusion, the patient’s vascular anatomy, and the experience of the medical team. Despite these variables, the procedure is generally efficient, with many patients benefiting from timely intervention.
Immediate Post-Procedure Care
After the EVT procedure, patients are closely monitored in a specialized stroke unit or intensive care unit. Immediate post-procedure care involves:
- Neurological status assessment
- Vital sign monitoring
- Imaging studies to evaluate the success of the procedure
Careful observation during this period is crucial to identify and address any potential complications early.
Long-term Recovery and Rehabilitation Needs
The recovery process following EVT can vary significantly among patients. While some may recover quickly, others may require extensive rehabilitation. Rehabilitation needs are assessed on an individual basis, taking into account the extent of the stroke and the patient’s overall health.
Long-term recovery often involves a multidisciplinary team, including physical therapists, occupational therapists, and speech therapists. The goal is to help patients regain as much independence as possible and improve their quality of life.
Studies have shown that patients undergoing EVT require careful post-procedure care and rehabilitation to achieve optimal outcomes. By understanding the procedure duration and recovery timeline, healthcare providers can better support patients through the recovery process.
Key Fact #7: Clinical Outcomes and Success Rates
The effectiveness of EVT in treating acute ischemic stroke is evident in its ability to significantly enhance patient functionality and reduce long-term disability. This section will explore the clinical outcomes and success rates associated with EVT, providing insights into its efficacy.
Statistical Improvement in Patient Functionality
Numerous studies have demonstrated that EVT leads to significant improvements in patient functionality. For instance, a study published in the New England Journal of Medicine found that EVT resulted in improved functional outcomes in patients with acute ischemic stroke due to large vessel occlusion.
- Improved functional outcomes in 46% of EVT-treated patients compared to 26.5% in the control group.
- Significant reduction in disability, with more patients achieving functional independence.
Reduction in Long-term Disability
EVT has been shown to reduce long-term disability in patients with acute ischemic stroke. The procedure’s ability to rapidly restore blood flow to the affected brain area minimizes tissue damage and promotes better recovery.
A meta-analysis of EVT trials revealed a significant reduction in long-term disability among patients treated with EVT compared to those receiving standard care alone.
Factors Affecting Treatment Success
Several factors influence the success of EVT, including:
- Time to treatment: Earlier intervention is associated with better outcomes.
- Patient selection: Careful selection based on imaging and clinical criteria.
- Operator experience: The skill and experience of the medical team performing EVT.
Understanding these factors is crucial for optimizing EVT outcomes and ensuring that patients receive the best possible care.
Conclusion: The Future of EVT in Stroke Management
Endovascular Thrombectomy (EVT) has revolutionized the treatment of acute ischemic stroke, offering new hope for patients with large vessel occlusions. As research continues to advance, the evt future looks promising, with ongoing studies and trials shaping the landscape of stroke management.
Recent data from clinical trials have demonstrated the efficacy and safety of EVT, leading to its increased adoption in clinical practice. The thrombectomy future is being shaped by advancements in device technology, imaging techniques, and patient selection criteria, all aimed at improving patient outcomes.
The future of EVT in stroke management will likely involve further refinements in procedure techniques, expanded treatment windows for select patients, and enhanced post-procedure care. As the medical community continues to explore the potential benefits and challenges of EVT, it is clear that this treatment modality will remain a critical component of stroke management.
By continuing to advance our understanding of EVT and its applications, we can improve the lives of patients affected by ischemic stroke, reducing long-term disability and improving overall outcomes.
FAQ
What does EVT stand for in medical terms?
EVT stands for Endovascular Thrombectomy, a medical procedure used to treat acute ischemic stroke by removing blood clots from the brain arteries.
What is EVT used for?
EVT is used to treat ischemic stroke by restoring blood flow to the brain, reducing long-term disability, and improving patient outcomes.
How long does an EVT procedure take?
The average EVT procedure length is between 1-2 hours, depending on the complexity of the case and the patient’s condition.
What are the patient selection criteria for EVT?
Patients with large vessel occlusion, as identified through neuroimaging assessment protocols, are typically eligible for EVT, provided they meet specific inclusion and exclusion criteria.
What is the critical time window for EVT treatment?
The standard treatment window for EVT is 6-8 hours from stroke onset, although extended time windows may be considered for select patients based on clinical evaluation and imaging findings.
How does EVT compare to traditional stroke treatments?
EVT has been shown to be superior to intravenous thrombolysis alone in treating ischemic stroke, particularly for patients with large vessel occlusion, and is often used in combination with other treatments.
What are the clinical outcomes and success rates of EVT?
EVT has been associated with significant improvements in patient functionality, reduction in long-term disability, and improved outcomes, although treatment success can be influenced by various factors, including timely treatment and patient selection.
What is cerebral thrombectomy?
Cerebral thrombectomy, also known as EVT, is a medical procedure that involves removing a blood clot from the brain arteries to restore blood flow and reduce damage caused by ischemic stroke.
What is thrombectomy for stroke?
Thrombectomy for stroke, or EVT, is a procedure that removes a blood clot from the brain arteries to treat ischemic stroke and improve patient outcomes.
How long does it take to recover from a thrombectomy?
Recovery from a thrombectomy, or EVT, can vary depending on the individual patient’s condition, but typically involves immediate post-procedure care and long-term rehabilitation needs.
References
- Saver, J. L., Goyal, M., van der Lugt, A., Menon, B. K., Majoie, C. B., Dippel, D. W., Campbell, B. C., Nogueira, R. G., Demchuk, A. M., Tomasello, A., Cardona, P., Devlin, T. G., Frei, D. F., du Mesnil de Rochemont, R., Berkhemer, O. A., Jovin, T. G., Siddiqui, A. H., van Zwam, W. H., Davis, S. M., … HERMES Collaborators. (2016). Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA, *316*(12), 1279-1288. https://pubmed.ncbi.nlm.nih.gov/27673305/