At Liv Hospital, we know how fast and important it is to treat stroke quickly. Endovascular Thrombectomy (EVT) is a new, less invasive way to treat this serious condition.
EVT is now the top choice for treating stroke caused by big blockages in the brain. It works by removing the clot in a major artery. This helps blood flow back to the brain, which greatly improves patient results.
Our team of experts uses the latest medical knowledge and dedication to perform EVT stroke procedures. They bring new hope and better results for patients.
Key Takeaways
- Endovascular Thrombectomy (EVT) is a minimally invasive procedure for treating acute ischemic stroke.
- EVT is the gold standard intervention for large-vessel occlusion (LVO).
- The procedure involves removing the blood clot blocking a major cerebral artery.
- EVT significantly improves patient outcomes by restoring blood flow to the brain.
- Liv Hospital’s team of experts is committed to excellence in performing EVT procedures.
The Science Behind EVT Stroke Treatment

Understanding EVT stroke treatment is key to seeing its benefits. We’ll look at how it tackles blood flow blockages in the brain.
Acute Ischemic Stroke: When Blood Flow Is Blocked
An acute ischemic stroke happens when a blood clot blocks a brain artery. This cuts off oxygen and nutrients, causing brain damage or death. Large vessel occlusions are very dangerous because they harm a big part of the brain.
The evt procedure is made to tackle these big blockages. It uses a catheter to reach the clot and remove it. This helps restore blood flow to the brain.
How EVT Addresses Large Vessel Occlusions
EVT is a thrombectomy procedure aimed at the clot causing the stroke. Studies show it works better when combined with standard medical treatment (SMT) for big infarcts. This combo leads to better results than SMT alone.
In the evt procedure, a specialist guides a catheter to the blocked artery. They use a stent retriever or aspiration to clear the clot. This method greatly improves outcomes and lowers death rates in stroke patients.
What Is EVT? Decoding the Medical Abbreviation
EVT stands for Endovascular Thrombectomy, a key stroke treatment. It’s vital for patients with large vessel blockages.
To grasp EVT, let’s dive into its meaning and importance. EVT stands for Endovascular Thrombectomy. It’s a surgery that removes brain blood clots without a big cut.
EVT Meaning: Endovascular Thrombectomy Explained
Endovascular Thrombectomy, or EVT, is a detailed term. “Endovascular” means it’s done inside the blood vessels. “Thrombectomy” is about removing blood clots. Neurointerventionalists use special tools and imaging to do this.
The EVT process includes:
- Accessing the blocked blood vessel through a small incision in the groin
- Navigating a catheter to the site of the occlusion in the brain
- Using devices such as stent retrievers or aspiration catheters to remove the clot
- Restoring blood flow to the affected area of the brain
Other Names: Cerebral Thrombectomy and Stroke Thrombectomy
EVT is also called Cerebral Thrombectomy and Stroke Thrombectomy. These names show its purpose and where it’s done.
These names all point to the same thing: removing brain clots to treat strokes. The different names show the focus on brain clots and stroke treatment.
The Evolution of Stroke Treatment: From tPA to EVT
Stroke care is evolving, with EVT becoming key for those not helped by tPA. This change is due to new medical tech and better understanding of strokes.
Traditional Stroke Treatments and Their Limitations
Tissue plasminogen activator (tPA) has long been a main stroke treatment. Given intravenously, it breaks up blood clots. But, it only works well within 4.5 hours and not always for big clots.
The need for better treatments grew as tPA’s limits became clear. Big clots, linked to severe strokes, are a big challenge for tPA.
How EVT Changed the Landscape of Stroke Care
Endovascular Thrombectomy (EVT) has changed stroke treatment, mainly for big clots. It’s a minimally invasive method where a doctor uses a catheter to remove the clot.
Research shows EVT works better for big clots, leading to better outcomes. It’s now a key part of stroke care, giving hope to those not helped by tPA.
EVT’s success is leading to more use. This shows growing recognition of its benefits in improving patient results.
| Treatment | Time Window | Efficacy in Large Vessel Occlusions |
| tPA | Up to 4.5 hours | Limited |
| EVT | Up to 24 hours in some cases | High |
This table shows why EVT is now often the first choice for eligible patients.
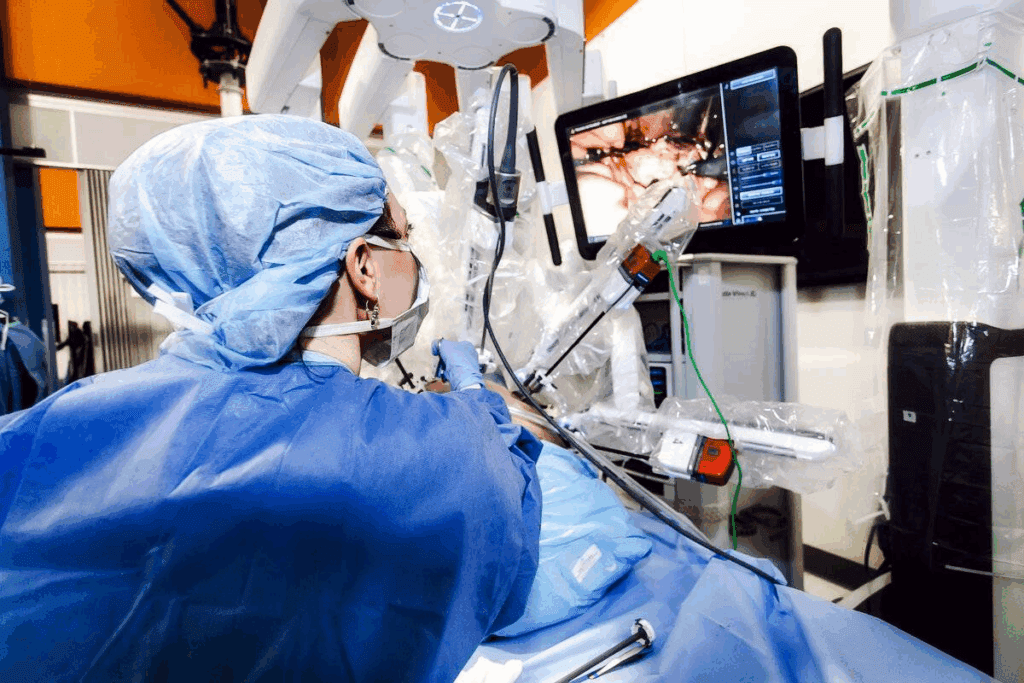
The EVT Procedure: A Complete Guide
The EVT procedure is a detailed medical process aimed at restoring blood flow to the brain. It’s a specialized treatment for acute ischemic stroke. We will dive into its critical steps.
Patient Preparation and Anesthesia Considerations
Before starting, patients get ready with imaging studies to confirm the blockage. Anesthesia is key, as it can be either conscious sedation or general anesthesia. This depends on the patient’s health and the team’s choice.
A study in the Journal of Neurointerventional Surgery highlights the importance of anesthesia. It shows that the right choice can greatly affect the outcome.
“The optimal anesthesia strategy for EVT remains a topic of debate, with some centers favoring conscious sedation and others preferring general anesthesia.”
Journal of Neurointerventional Surgery
Catheter Navigation Through the Arterial System
The procedure uses a catheter to reach the blocked vessel. It goes through the arterial system with advanced imaging. The access point is usually the femoral artery.
Real-time imaging guides the catheter’s path. This ensures accurate placement and reduces risks. The team’s skill and experience are vital in navigating the complex arteries.
| Navigation Step | Description | Imaging Guidance |
| 1. Access | Femoral artery access | Fluoroscopy |
| 2. Catheter Placement | Guiding catheter placement | Roadmapping |
| 3. Microcatheter Navigation | Microcatheter navigation to clot | Real-time fluoroscopy |
Clot Removal Techniques and Post-Procedure Care
With the catheter in place, the clot removal starts. Techniques like stent retrievers or aspiration thrombectomy are used. The choice depends on the clot and the team’s preference.
The whole procedure takes about 1 to 2 hours. After, patients are closely watched in a neuro-intensive care unit. This is to manage any complications and aid in recovery.
Post-procedure care is critical for preventing complications and ensuring the best outcomes. This includes monitoring the patient’s neurological status, managing blood pressure, and using antiplatelet therapy as needed.
In conclusion, the EVT procedure is complex and requires precise execution and careful patient management. Understanding the steps from preparation to post-care helps us appreciate this life-saving treatment.
Advanced EVT Techniques and Devices
Advanced EVT techniques have changed how we treat acute ischemic stroke. New devices and methods are being developed to better help patients. This is making a big difference in how we treat strokes.
Stent Retrievers: Capturing and Removing Clots
Stent retrievers are a big step forward in EVT technology. They are made to grab and remove blood clots from the brain’s blood vessels. By using a stent-like device through a catheter, doctors can pull out the clot. This helps blood flow back to the brain.
Studies show thatstent retrievers improve outcomes for patients with big blockages. They are now a key part of many EVT procedures.
Aspiration Thrombectomy: Vacuuming Blood Clots
Aspiration thrombectomy is another advanced EVT technique. It uses a catheter to suck out the clot. This method can be used alone or with stent retrievers for better results.
This technique is great for hard-to-remove clots or those in hard-to-reach places. It gives doctors another tool to use in EVT.
Combination Approaches for Complex Cases
For some cases, using more than one EVT technique is needed. Doctors might use stent retrievers and aspiration thrombectomy together. This mix can help tackle tough clots better.
Using different techniques lets doctors tailor treatment to each patient. This personal touch is key to improving EVT results.
Clinical Benefits of EVT for Stroke Patients
EVT for stroke patients offers many benefits, improving their lives and saving them. As medical technology advances, knowing these benefits is key for doctors and patients.
Improved Functional Outcomes and Reduced Mortality
Research shows EVT greatly helps stroke patients. It removes clots and brings blood back to the brain. This reduces damage and boosts recovery chances.
Also, EVT lowers death rates in stroke patients. Quick clot removal saves brain tissue and lowers severe complication risks. This is a big step forward in stroke care, giving hope to patients and their families.
Quality of Life Improvements After Successful EVT
Successful EVT not only saves lives but also improves quality of life. It helps patients regain independence and return to daily activities. This means a better life for them, with more activity and social interaction.
Also, EVT reduces healthcare costs over time. It cuts down on the need for long-term rehab and lowers the risk of complications. This makes EVT a cost-effective treatment for acute ischemic stroke.
In summary, EVT brings many benefits to stroke patients. It improves their function, lowers death rates, and enhances their quality of life. As we continue to improve this technique, we can expect even better care for stroke patients.
Time Considerations: How Long Does a Thrombectomy Take?
Knowing how long a thrombectomy takes is key for doctors and patients. Quick action is vital in treating strokes. EVT (Endovascular Thrombectomy) works best when done fast.
Typical Procedure Duration from Start to Finish
The EVT procedure usually lasts 1 to 2 hours. But, it can change based on the blockage’s complexity, the patient’s health, and the team’s skill.
Here’s a look at the EVT steps and how long they take:
| Procedure Step | Estimated Duration |
| Patient Preparation | 15-30 minutes |
| Catheter Navigation | 30-60 minutes |
| Clot Removal | 15-45 minutes |
| Post-Procedure Care | 15-30 minutes |
| Total Procedure Time | 1-2 hours |
The Critical Time Window for Effective Treatment
The best time for thrombectomy is within 6 to 8 hours after symptoms start. Research shows EVT works best in this time, improving patient results.
Quick treatment leads to better results and lower death rates. So, it’s important for patients to get help right away if they have stroke symptoms.
In summary, knowing the time frame for thrombectomy is key for better care and results. Quick action helps patients get the treatment they need.
Patient Selection: Who Qualifies for EVT Stroke Treatment?
Choosing the right patients for EVT stroke treatment is key. We look at many factors to see if the treatment is safe and will help. This makes sure the treatment is a good choice for each patient.
We use advanced imaging and a detailed check-up to decide. Imaging criteria help us find the best candidates for treatment.
Imaging Criteria and Clot Location Requirements
To get thrombectomy for stroke, patients must meet certain imaging standards. We use CT scans or MRI to see where the clot is and how big it is. We also check how much brain tissue is affected.
Where the clot is located is also important. Those with big clots in main blood vessels are usually treated. This is because these clots can cause a lot of damage if not treated quickly.
- CT scans help identify the clot’s location and size.
- MRI assesses the extent of brain tissue damage.
- Vessel imaging determines the presence of large vessel occlusions.
Understanding Why Only 10% of Stroke Patients Are Eligible
Only about 10 percent of stroke patients can get EVT stroke treatment. There are several reasons for this.
One big reason is the time needed for treatment. Patients must get help quickly after their stroke symptoms start. This can be hard because of delays in getting to a hospital or a treatment center.
Other reasons include the type of stroke, where and how big the clot is, and the patient’s health. These strict rules help make sure EVT is given to those who will benefit the most.
By carefully picking patients, we can make thrombectomy for stroke more effective. This helps improve the lives of those affected.
Potential Risks and Complications of Thrombectomy Brain Procedures
While EVT has changed stroke treatment, it’s important to know the risks. These procedures carry dangers that doctors must manage well. This ensures the best results for patients.
Procedural Complications
During EVT, several complications can happen. These include:
- Bleeding: This can occur due to the puncture site or during the procedure itself.
- Vessel damage: The catheter navigation through the arterial system can sometimes cause damage to the blood vessels.
- Embolism: There’s a risk of dislodging parts of the clot, which can travel to other parts of the brain, causing further occlusion.
To reduce these risks, doctors use advanced imaging and precise catheter systems.
Post-Procedure Risks and Management Strategies
After the procedure, patients face several risks. These include:
| Complication | Description | Management Strategy |
| Re-occlusion | The treated vessel re-blocks | Close monitoring, anticoagulant therapy |
| Hemorrhagic transformation | Bleeding into the infarcted area | Careful blood pressure management, avoiding anticoagulants |
| Infection | Infection at the puncture site or systemic | Prophylactic antibiotics, wound care |
Managing these risks requires a team effort. Neurologists, interventional radiologists, and intensive care specialists work together. This approach helps improve patient outcomes.
It’s important to remember that while complications can happen, EVT’s benefits often outweigh the risks. Careful patient selection and precise technique are key.
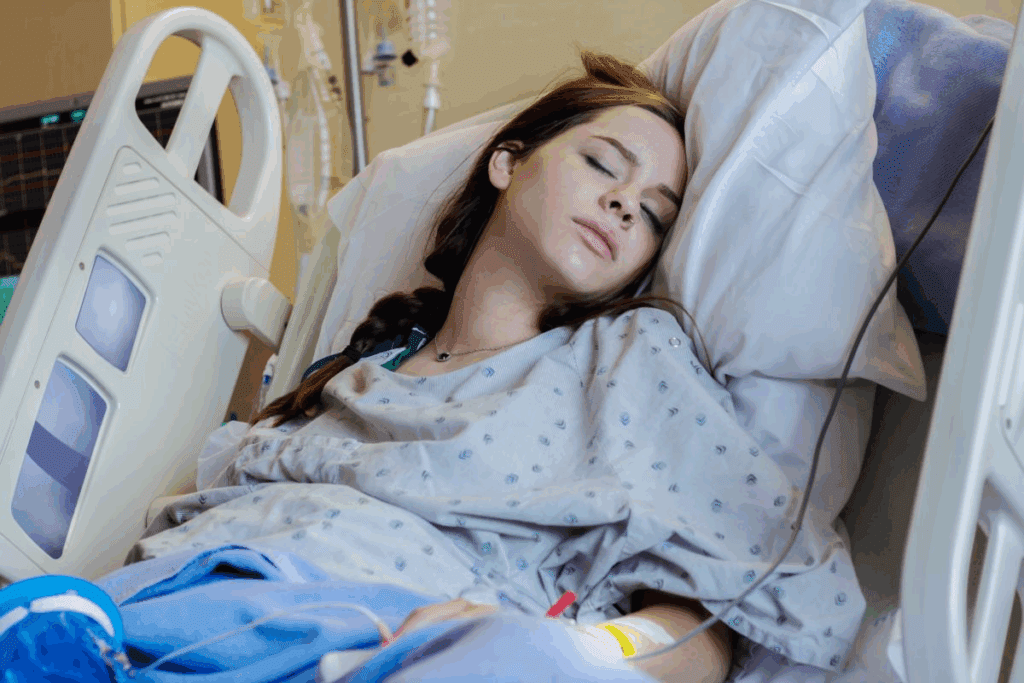
Recovery Journey After an EVT Procedure
The recovery path after an EVT procedure has many steps. It starts with hospital care and then moves to rehabilitation. Understanding these stages is key for patients.
Immediate Hospital Recovery Phase
Right after an EVT, patients stay in the ICU or a stroke unit. We focus on their immediate care to keep them stable. The team watches their vital signs and brain health closely.
In this time, managing pain and comfort is very important. Patients might feel some pain or drowsiness. But, this usually goes away in a few hours. We aim to keep them as comfortable as possible.
Rehabilitation Process and Timelines
When patients are stable, they start rehab. This includes physical, occupational, and speech therapy. Our goal is to help them regain independence and improve their skills.
The rehab time varies based on the stroke’s severity and the patient’s health. It can last from weeks to months. We help set realistic goals and support patients and their families every step of the way.
Long-term Follow-up and Secondary Prevention
After rehab, patients get ongoing care. We stress the need for secondary prevention to avoid future strokes. This includes managing blood pressure, diabetes, and cholesterol, and living a healthy lifestyle.
Our team helps create a care plan for the long term. This includes regular check-ups and monitoring. By focusing on prevention, we help patients stay healthy and avoid future strokes.
The Future of Endovascular Thrombectomy
New technologies and better techniques will make EVT better for stroke patients. As we keep improving in endovascular thrombectomy, we see better results for patients.
Advancements in Technology and Techniques
The future of EVT depends on new tech and better methods. Stent retrievers and aspiration catheters are getting better. They help remove clots more effectively and safely.
New devices are coming out to help EVT work better. These include thrombectomy devices with advanced clot retrieval mechanisms and improved imaging technologies for better views during the procedure.
Expanding Access to EVT
We need to make EVT available to more people. This means training more specialists and equipping more centers with the right tools and tech.
By doing this, more patients can get EVT, no matter where they are. This is key for areas that don’t have many EVT facilities.
We’re excited to see how far we can take EVT. We’re looking forward to the future and the better care we’ll be able to give our patients.
Conclusion
Endovascular Thrombectomy (EVT) has changed how we treat acute ischemic stroke. It has greatly improved patient outcomes. Studies show EVT can help more patients live independently at 90 days.
The DAWN trial found 49% of patients in the EVT group could live independently. This is compared to 13% in the control group. The DEFUSE 3 trial also showed good results, with 45% of the treatment arm achieving good outcomes. This is compared to 17% in the medical arm.
Getting EVT quickly is key. Every hour delay lowers the chance of a good outcome by 7.7%. Recent studies, like the RESCUE-Japan LIMIT and ANGEL-ASPECT studies, support EVT’s benefits.
We are working to make more patients eligible for EVT. Currently, less than 20% of patients get EVT. By expanding eligibility and improving techniques, we can improve stroke patients’ lives. Our goal is to provide top-notch healthcare and support to patients worldwide.
FAQ
What does EVT stand for in medical terms?
EVT stands for Endovascular Thrombectomy. It’s a procedure to treat acute ischemic stroke by removing blood clots from the brain.
What is the EVT procedure for stroke treatment?
The EVT procedure uses a catheter to reach the blocked vessel in the brain. A stent retriever or aspiration device then removes the clot. This restores blood flow to the brain.
How long does a thrombectomy procedure typically take?
A thrombectomy procedure usually takes 1-2 hours. This time can vary based on the case’s complexity and the patient’s condition.
What are the benefits of EVT in treating acute ischemic stroke?
EVT improves outcomes and reduces mortality in stroke patients. It quickly restores blood flow, minimizing brain damage and promoting recovery.
Who is eligible for EVT stroke treatment?
Eligibility for EVT depends on imaging criteria and clot location. Only about 10% of stroke patients qualify due to the need for timely intervention.
What are the potentials risks and complications of thrombectomy brain procedures?
Risks include bleeding and vessel damage during the procedure. Post-procedure risks can be managed with proper care and monitoring.
What is the recovery process like after an EVT procedure?
Recovery starts with immediate hospital care. It then moves to a rehabilitation phase lasting weeks or months. Long-term follow-up is also necessary to monitor progress and prevent future strokes.
How has EVT changed the landscape of stroke care?
EVT has revolutionized stroke care. It offers a highly effective treatment for acute ischemic stroke, improving outcomes for eligible patients and expanding treatment possibilities.
What is the future of endovascular thrombectomy?
The future of EVT looks promising. Emerging technologies and technique refinements will continue to improve outcomes for stroke patients worldwide.
What other names are used to refer to EVT?
EVT is also known as cerebral thrombectomy and stroke thrombectomy. These names reflect its focus on removing brain clots to treat acute ischemic stroke.
References
- Saver, J. L., Goyal, M., van der Lugt, A., Menon, B. K., Majoie, C. B., Dippel, D. W., Campbell, B. C., Nogueira, R. G., Demchuk, A. M., Tomasello, A., Cardona, P., Devlin, T. G., Frei, D. F., du Mesnil de Rochemont, R., Berkhemer, O. A., Jovin, T. G., Siddiqui, A. H., van Zwam, W. H., Davis, S. M., … HERMES Collaborators. (2016). Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA, *316*(12), 1279-1288. https://pubmed.ncbi.nlm.nih.gov/27673305/



































