Last Updated on November 25, 2025 by Ugurkan Demir

Urinary incontinence is a common problem worldwide, hitting older adults and women hard. The NIDDK says over 60% of women deal with it. This can really cut down on their physical activity and lower their quality of life.
Recent research shows that specific exercise programs are very effective as a first treatment. Studies prove that pelvic floor exercises can lessen urinary incontinence symptoms. They also boost bladder control. At Liv Hospital, we offer care that’s backed by science and focused on the patient. We mix proven exercises with full medical support exercises for bladder incontinence.
Getting to know urinary incontinence is key to managing it well. It’s a complex issue that affects many people worldwide.
Urinary incontinence hits people of all ages, but it’s more common as we get older. About 30% of older adults deal with it. Women, after childbirth, and men, after prostate surgery, are more likely to experience it.
It’s important to spread awareness about urinary incontinence. It affects everyone, not just the elderly. Pregnancy, menopause, and prostate issues raise the risk.
Urinary incontinence can really change someone’s life. It affects not just physical health but also emotional well-being and social interactions. It can lead to anxiety, depression, and a lower quality of life.
It makes everyday tasks hard. Going to the gym, traveling, or attending social events becomes a challenge. Knowing about urinary incontinence is the first step to managing it.
By trying exercises and natural treatments, people can lessen the impact of urinary incontinence. We’ll look into these options next.
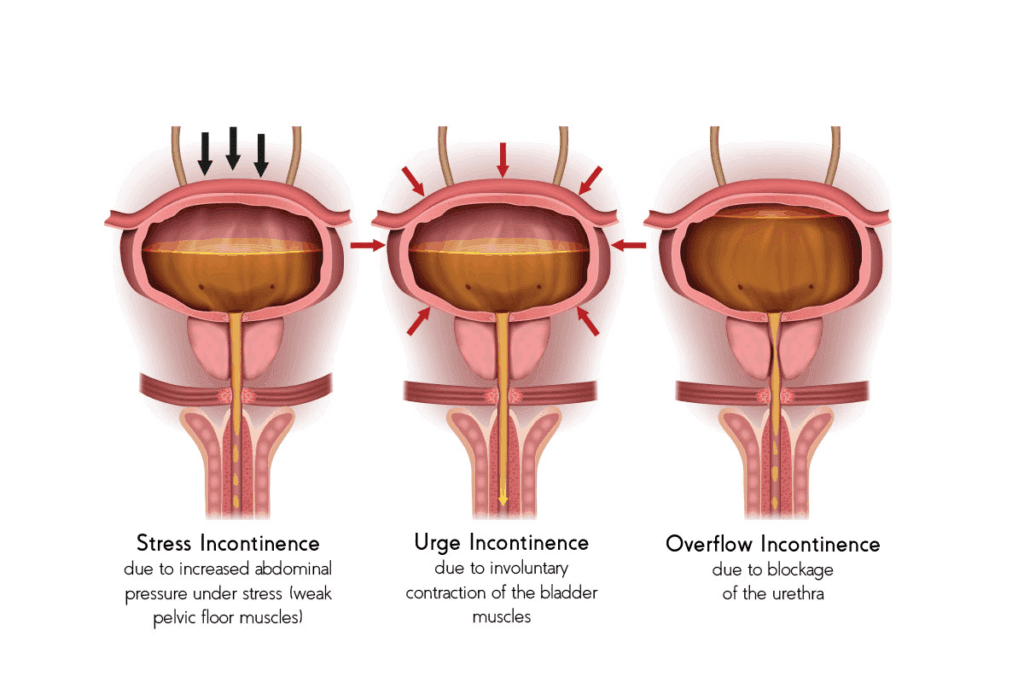
Urinary incontinence comes in different forms, each with its own causes and symptoms. Knowing these differences is key to finding the right treatment.
Stress incontinence happens when moving or pressure on the bladder makes you leak urine. It’s common when you cough, sneeze, laugh, or exercise. It’s usually because the pelvic floor muscles or urethral sphincter are weak.
Symptoms include:
Urge incontinence, also known as overactive bladder, is when you suddenly feel the need to urinate. This can lead to involuntary leakage. The bladder muscles contract too often or at the wrong times.
Symptoms include:
Mixed incontinence is when you have symptoms of both stress and urge incontinence. This makes diagnosis and treatment harder. But knowing it’s mixed helps in creating a better treatment plan.
Symptoms include a mix of:
Overflow incontinence happens when the bladder doesn’t empty fully. This leads to constant or frequent dribbling. It’s often due to obstruction or weak bladder muscles.
Symptoms include:
Knowing the type of urinary incontinence you have is the first step to managing it. By understanding the causes and symptoms, you can find the right treatments. This can include exercises and lifestyle changes to improve your life.
Recent studies have shown that exercises can help manage urinary incontinence. This offers new hope for those dealing with it. The research has given us insights into how certain exercises can strengthen the muscles that control urination. This can improve bladder control.
Studies from 2024-2025 have shown great promise in using exercises for urinary incontinence. A study found that 12 weeks of low-impact exercise reduced daily incontinence episodes by about 60 percent. This shows that exercise could be a good treatment for urinary incontinence.
“Pelvic floor muscle exercises have proven effectiveness in elderly populations, highlighting their importance as a non-invasive treatment for urinary incontinence.”
Recent research also highlights the role of pelvic floor muscle exercises in managing incontinence. These exercises, known as Kegel exercises, strengthen the muscles that support bladder control. This leads to fewer incontinence episodes.
Exercises for bladder incontinence strengthen the pelvic floor muscles, which are key for bladder control. Weak muscles can lead to incontinence. Regular pelvic floor exercises can make these muscles stronger and more enduring. This improves bladder control.
While results can differ, most people see improvements in bladder control in 6 to 8 weeks of regular exercise. It’s important to be patient and keep practicing. The success of these exercises depends on consistent effort and proper technique.
| Exercise Regimen | Expected Improvement Timeline | Notable Benefits |
| Pelvic Floor Exercises (Kegel) | 6-8 weeks | Strengthens pelvic floor muscles, improves bladder control |
| Low-Impact Exercises | 12 weeks | Reduces daily incontinence episodes by approximately 60% |
Before starting bladder control exercises, it’s important to prepare well. This preparation makes the exercises more effective and avoids problems.
Talking to a doctor before starting any exercise is key, more so for those with health issues. It’s wise to discuss your plans with your doctor to find out if there are any issues. For example, people with severe pelvic organ prolapse or certain neurological conditions might need to adjust their routine.
Telling your doctor about any medicines you’re taking is also important. Some medicines can affect bladder control or interact with the exercises. This ensures a safe and effective start to your program.
Key points to discuss with your healthcare provider:
Having a regular exercise schedule is key to success. Try to set a specific time each day for your exercises. Doing it at the same time every day makes it a habit.
Here are some tips for a good schedule:
Tracking your progress and any incidents is very important. Using the right tools can help you see patterns, monitor improvements, and adjust your routine if needed.
Some good tools include:
By getting medical advice, sticking to a schedule, and using tracking tools, you can greatly improve your chances of success. Remember, success takes time and effort. With the right preparation, you can reach your goals.
Kegel exercises are a simple yet effective way to strengthen the muscles that support bladder control. They target the pelvic floor muscles. This can greatly improve bladder control and reduce urinary incontinence.
The first step is to find your pelvic floor muscles. Try stopping urine flow midstream. The muscles you use are your pelvic floor muscles. Remember, only do this occasionally to avoid incomplete bladder emptying.
To do Kegel exercises right, follow these steps:
A common mistake is using the wrong muscles, like those in the abdomen, thighs, or buttocks. Focus on the muscles around your urethra and anus. Try Kegels in different positions to find what works best for you.
As you get better, increase your training by:
Consistency is key. Regular practice strengthens your pelvic floor muscles. This improves bladder control over time. Try to do Kegels daily, like while brushing your teeth or waiting in line.
Bridge exercises focus on the glutes and core. They help keep the pelvic floor stable. This can reduce bladder incontinence symptoms.
To start, lie on your back with knees bent and feet flat, hip-width apart. Lift your hips towards the ceiling, squeezing your glutes and lower back. Hold for a few seconds, then lower back down.
When you’re ready, try lifting one leg off the ground while bridging. This makes the exercise harder by requiring more core and glute strength. Lift one foot straight out, then your hips, as in a standard bridge. Switch legs with each rep for balanced strengthening.
Tips for Single-Leg Bridges:
Bridge exercises are great for bladder control because they strengthen the glutes and core. These muscles are key to a stable pelvic floor. A strong pelvic floor can better handle pressures that cause incontinence.
Doing bridge exercises regularly, along with other pelvic floor exercises, can greatly improve bladder control over time.
Incorporating squat variations into your workout can boost pelvic strength and lower body stability. Squats work many muscles, including those important for bladder control.
Wall squats are great for newbies or those needing extra support. Here’s how to do them:
Wall squats strengthen your quadriceps, hamstrings, and glutes. These muscles support your pelvic floor.
When you’re ready, move to free-standing squats. This version requires balance and works your core more.
Free-standing squats boost lower body strength and stability. This helps with better bladder control.
Pulsing squats involve small movements in and out of a squat. It’s great for endurance in your lower body and pelvic floor.
Pulsing squats are tough on your muscles. They improve muscle memory, helping with long-term bladder control.
| Squat Variation | Benefits | Target Muscles |
| Wall Squats | Supports beginners, improves strength | Quadriceps, Hamstrings, Glutes |
| Free-Standing Squats | Enhances balance, engages core | Quadriceps, Hamstrings, Glutes, Core |
| Pulsing Squats | Builds endurance, improves muscle memory | Quadriceps, Hamstrings, Glutes, Pelvic Floor |
Bladder training is a useful way to lessen urgency and boost urinary health. It involves a structured plan to better control the bladder. This can lead to fewer incontinence episodes.
A scheduled voiding protocol sets a routine for when to go to the bathroom. It’s based on the idea that by increasing the time between bathroom visits, the bladder can hold more urine.
Urge suppression is key in bladder training. It’s about managing and suppressing the urge to urinate.
Key strategies include:
Increasing the time between bathroom visits is vital for better bladder capacity. This is done by:
By using these methods, people can effectively reduce urgency and enhance bladder control.
Strengthening our pelvic floor and improving bladder control is possible with dynamic neuromuscular stabilization. This method focuses on the core muscles. It boosts stability and helps with bladder control.
Diaphragmatic breathing is key in dynamic neuromuscular stabilization. It engages the diaphragm, improving core activation and relaxation. Here’s how to do it:
Core activation isn’t just for exercises. It’s also for daily activities. For example, when lifting or standing up, engage your core by:
This helps improve stability and reduces incontinence risk.
As you get better at dynamic neuromuscular stabilization, try more challenging exercises. These can improve core integration and bladder control. Some examples include:
| Exercise | Description | Benefit |
| Single-leg bridges | Lie on your back, lift one leg towards the ceiling, and bridge your hips. | Enhances core stability and pelvic floor strength. |
| Plank variations | Hold a plank position with variations such as lifting one leg or arm. | Improves overall core strength and stability. |
| Dynamic planks | Move from a plank to a squat or other positions, engaging your core throughout. | Challenges core stability and enhances functional strength. |
Adding these challenges to your routine can help you reach advanced levels of core integration. This will also improve your bladder control.
Therapeutic yoga is a great way to manage incontinence. It strengthens the pelvic floor and promotes relaxation. Adding specific yoga poses to your daily routine can improve bladder control and overall well-being.
Child’s Pose, or Balasana, is a restorative yoga pose. It relaxes the pelvic muscles and reduces stress. To do this pose, kneel on the mat with knees wide apart, then sit back onto your heels. Stretch your arms out in front and lower your forehead to the ground, breathing deeply.
Malasana, or Squat Pose, is great for increasing pelvic floor awareness and strength. Stand with feet wider than hip-width apart, then squat down. Keep your back straight and your hands in a prayer position. This pose opens up the pelvic area and engages the pelvic floor muscles.
Happy Baby Pose is a gentle stretch. It relaxes the lower back and pelvis. Lie on your back, grab your knees, and gently pull them towards your chest. This pose promotes flexibility and relaxation in the pelvic area.
To manage incontinence with yoga, a consistent daily practice is key. Here’s a simple 15-minute routine:
| Pose | Duration | Benefits |
| Child’s Pose | 5 minutes | Relaxes pelvic muscles, reduces stress |
| Malasana (Squat Pose) | 3 minutes per side | Increases pelvic floor awareness and strength |
| Happy Baby Pose | 3 minutes | Stretches lower back and pelvis, promotes flexibility |
| Deep Breathing | 4 minutes | Enhances relaxation, reduces anxiety |
By dedicating just 15 minutes a day to this therapeutic yoga routine, you can take a significant step towards managing incontinence and improving your quality of life.
Pilates exercises help improve core and pelvic floor strength. This is key for managing incontinence. They use controlled movements and breathing to strengthen muscles that help control the bladder.
Pelvic tilts and curls are basic Pilates moves that work the pelvic floor. To do a pelvic tilt, lie on your back with knees bent and feet flat. Engage your core and tilt your pelvis up, then slowly go back down. For pelvic curls, lift your hips off the floor, squeezing your pelvic floor as you lift.
The Hundred is a classic Pilates move that strengthens the core and promotes deep breathing. For newbies, a modified version keeps the legs bent and feet on the floor. Focus on your breath, inhaling for five counts and exhaling for five, while keeping your core and pelvic floor muscles tight.
Toe taps help improve coordination between your abdominal and pelvic floor muscles. Lie on your back with knees bent and feet lifted. Slowly tap your toes on the ground, one at a time, keeping your core and pelvic floor muscles engaged.
Breath control is key in Pilates, making exercises more effective. Synchronizing your breath with movements helps engage your core and pelvic floor muscles more. Practice deep, diaphragmatic breathing to support your pelvic floor.
| Exercise | Primary Benefit | Tips for Beginners |
| Pelvic Tilts | Strengthens pelvic floor muscles | Start with slow movements |
| Modified Hundred | Engages core and promotes deep breathing | Keep legs bent for support |
| Toe Taps | Enhances abdominal and pelvic floor coordination | Focus on slow, controlled movements |
Adding these Pilates exercises to your routine can improve your core and pelvic floor integration. This leads to better management of urinary incontinence.
Creating a detailed bladder control plan is key to managing incontinence well. We’ve looked at many exercises and methods to help you control your bladder better.
A good plan includes exercises, lifestyle changes, and sometimes other treatments. It’s important to be consistent and patient. By doing the 7 exercises we talked about, you can make your pelvic floor muscles stronger and control your bladder better.
Managing incontinence well means having a plan for bladder training and tracking your progress. You should also make changes as needed. It’s a good idea to talk to a healthcare professional to make a plan that fits you.
With a good bladder control plan, you can live a better life and do more things without worrying about incontinence. Start working on your bladder control today.
Urinary incontinence means you can’t control when you pee. It’s very common, affecting millions worldwide. It’s more common in women and older people.
There are five main types. These include stress incontinence, urge incontinence, mixed incontinence, overflow incontinence, and functional incontinence.
Exercises like Kegel strengthen the muscles around your bladder. This helps control your bladder better and reduces leaks.
Studies show you can see improvements in 6-8 weeks. This is if you do the exercises regularly and train your bladder.
First, talk to a doctor. Then, make a schedule for your exercises. Use tools to track your progress and any leaks.
Kegels target the muscles around your bladder. To do them right, find the right muscles, squeeze, and then release. Start with simple exercises and add more as you get stronger.
Techniques like scheduled voiding and urge suppression can help. They help you control your bladder better and reduce urgency.
It involves breathing exercises and core activation. It helps improve your core stability and bladder control.
Yes, they can. Yoga and Pilates strengthen your core and pelvic muscles. They also improve flexibility and help you relax.
Mix Kegels, bridges, and squats with bladder training and lifestyle changes. This will give you a full plan for managing your bladder.
While exercises and training are key, some natural remedies can help. Changes in diet and stress management might ease symptoms.
Kegels, core stability, and bladder training can help. They strengthen your muscles and improve bladder control during activities.
Yes, exercises like Kegels can help men. They improve the muscles that control your bladder and urethra.
National Center for Biotechnology Information. (2025). How to Stop Bladder Incontinence 7 Exercises for. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8743604/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!