Rheumatoid arthritis is known for its impact on joints, but it can also affect the eyes. Research shows that many people with rheumatoid arthritis face eye problems.What is eyeball arthritis? This essential guide explains how arthritis can affect your eyes, the symptoms, and treatment.
Understanding the connection between arthritis and eye health is key. The National Rheumatoid Arthritis Society says about 25% of those with rheumatoid arthritis may have eye issues. These can range from dry eye to serious inflammation that threatens vision.
At Liv Hospital, we stress the need for early detection and full care for eye problems linked to arthritis. Our focus is on the patient, making sure those with rheumatoid arthritis get the best care for their joints and eyes.
Key Takeaways
- Rheumatoid arthritis can significantly affect eye health.
- Approximately 25% of individuals with rheumatoid arthritis may experience eye symptoms.
- Early detection and full management are key for eye health.
- Ocular complications can range from dry eye to sight-threatening inflammation.
- Integrated care addressing both joint and eye health is essential.
The Connection Between Arthritis and Eye Health
Rheumatoid arthritis (RA) is more than just joint pain. It can also harm eye tissues. This autoimmune disorder affects not just the joints but also other parts of the body, including the eyes.
RA makes the immune system attack healthy tissues. This leads to inflammation that can harm other organs, like the eyes. This is why understanding the link between arthritis and eye health is so important.
How Systemic Inflammation Affects Eye Tissues
Inflammation from RA can cause eye problems. When the immune system attacks eye tissues, it can lead to dry eye syndrome, episcleritis, and scleritis. These conditions are caused by RA’s inflammatory effects on the eyes.
Inflammation can affect different parts of the eye, like the sclera, cornea, and lacrimal gland. For example, scleritis affects the sclera, causing pain, redness, and vision problems.
Statistics on Eye Problems in Arthritis Patients
People with RA are more likely to have eye problems than others. Eye issues linked to RA can greatly affect a person’s quality of life. This makes regular eye exams very important.
Research shows many RA patients face eye-related complications. Dry eye syndrome is a big problem for many. Knowing this, it’s clear why eye health is so critical for those with arthritis.
Understanding Eyeball Arthritis: What You Need to Know
Eyeball arthritis is closely tied to rheumatoid arthritis and can harm your eye health if not treated. We’ll explore what it is, its medical terms, and risk factors. This will help you understand it better.
Definition and Medical Terminology
Eyeball arthritis, also known as scleritis, is an inflammatory eye condition. It affects the sclera, the white outer eye wall. It causes intense pain, redness, and can lead to vision loss if not treated.
The term “scleritis” comes from the Greek word “scleros,” meaning hard. This refers to the tough outer eye layer. Knowing this term helps patients understand how serious it is and why they need quick medical help.
Risk Factors for Developing Eye Complications
Several factors can increase the risk of eye problems from eyeball arthritis. These include the severity of rheumatoid arthritis, how long you’ve had it, and other health conditions.
In the United Kingdom, about 25% of people with RA may have eye symptoms. This shows the importance of watching for signs and acting fast to avoid lasting damage.
Knowing these risk factors helps patients and doctors take steps to prevent and manage symptoms.
Common Eye Conditions Associated with Rheumatoid Arthritis
Rheumatoid arthritis (RA) can affect your eyes in many ways. We’ll look at the main eye problems linked to RA. We’ll talk about their symptoms, causes, and what they mean for your health.
Dry Eye Syndrome (Keratoconjunctivitis Sicca)
Dry eye syndrome is common in RA patients, affecting 16 to 28 percent. Dry eyes happen when inflammation damages tear glands. This leads to dryness, irritation, and grittiness. It can make daily life hard.
Episcleritis and Scleritis
Episcleritis and scleritis are eye problems caused by inflammation. Episcleritis makes your eyes red and irritated. Scleritis is more serious and can cause pain and vision loss if not treated.
Peripheral Ulcerative Keratitis
Peripheral ulcerative keratitis (PUK) is a serious eye issue. It involves inflammation and thinning of the cornea. PUK can cause vision loss if not treated quickly. It’s often linked to RA.
Retinal Vasculitis and Uveitis
Retinal vasculitis and uveitis affect the retina and uvea. These conditions can cause vision problems like blurred vision and floaters. Uveitis, in particular, is linked to RA and needs careful treatment.
It’s important to know about these eye problems linked to RA. Early treatment can help prevent vision loss. Both patients and doctors need to be aware of these issues.
Secondary Sjögren’s Syndrome and Its Impact on Eye Health
Rheumatoid arthritis and secondary Sjögren’s syndrome are closely linked, affecting eye care. About one-third of people with rheumatoid arthritis get secondary Sjögren’s. This condition makes the immune system attack glands that produce moisture.
Understanding the Connection with Rheumatoid Arthritis
Secondary Sjögren’s syndrome happens when rheumatoid arthritis patients also get this autoimmune condition. Sjögren’s syndrome damages glands that make tears and saliva. This leads to dry eyes and mouth.
This makes managing rheumatoid arthritis even harder. It adds more symptoms to deal with.
Tear Gland Dysfunction and Its Consequences
The lacrimal glands, which make tears, are often hit by secondary Sjögren’s syndrome. Tear gland dysfunction means less tear production. This causes dry, irritated eyes.
This condition, known as dry eye syndrome or keratoconjunctivitis sicca, can be painful. It can also blur vision and raise the chance of eye infections.
People with secondary Sjögren’s syndrome may have:
- Dryness and grittiness in the eyes
- Blurred vision
- Sensitivity to light
- Eye fatigue
Long-term Complications of Untreated Dry Eye
Untreated dry eye from secondary Sjögren’s syndrome can cause serious problems. Chronic dry eye can damage the cornea, which might lead to vision loss. It also raises the risk of eye infections and other eye problems.
It’s important to keep an eye on and treat dry eye. This helps avoid long-term damage and keeps eyes healthy in patients with secondary Sjögren’s syndrome.
Recognizing the Symptoms of Arthritis-Related Eye Conditions
Eye arthritis symptoms can start off subtle but catching them early is vital. Arthritis can affect the eyes in many ways. We’ll cover the common signs to help you know when to see a doctor.
Early Warning Signs You Shouldn’t Ignore
There are several early signs of arthritis-related eye issues. These include:
- Dryness or a gritty feeling in the eyes
- Redness or inflammation
- Itchiness or irritation
- Swelling around the eyes
- Changes in vision, such as blurriness or double vision
These signs might point to problems like dry eye, episcleritis, or scleritis. These are common in people with rheumatoid arthritis.
When to Seek Emergency Medical Attention
Some eye symptoms need quick action, while others can be treated at home. Get emergency help if you have:
- Sudden vision loss or severe eye pain
- Increased sensitivity to light
- Severe redness or swelling
- Eye discharge or pus
These severe signs might mean serious problems like retinal vasculitis or acute uveitis. They need fast treatment to avoid permanent vision loss.
Symptom Patterns for Different Eye Conditions
Different arthritis-related eye conditions have unique symptoms. For example:
- Dry Eye Syndrome causes constant dryness and irritation.
- Episcleritis and scleritis lead to redness, pain, and tenderness.
- Uveitis results in eye pain, light sensitivity, and vision problems.
Knowing these patterns helps in diagnosing and treating the condition well.
Spotting and treating arthritis-related eye issues early is key. It helps keep your vision and quality of life good. By catching symptoms early and getting medical help when needed, you can avoid lasting damage and keep your eyes healthy.
Diagnostic Approaches for Arthritis-Related Eye Problems
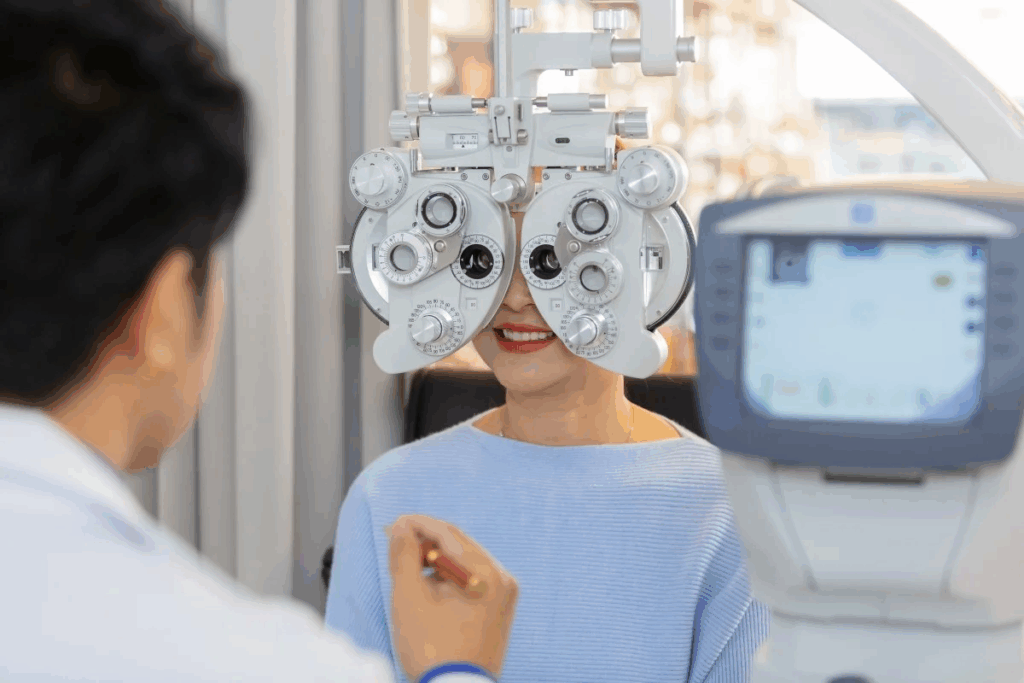
Diagnosing eye problems linked to arthritis needs a detailed plan. This includes regular eye exams and special tests. Early detection by an eye doctor can stop serious issues.
Comprehensive Eye Examinations and Specialized Tests
First, a thorough eye check is key. It looks at how well you see, the eye’s parts, and the tear film. Tests like the slit-lamp exam, OCT, and fluorescein angiography give more info.
Key Diagnostic Tests:
Test | Purpose |
Slit-lamp examination | Examines the anterior segment of the eye for signs of inflammation or damage |
Optical Coherence Tomography (OCT) | Provides detailed images of the retina and its layers |
Fluorescein Angiography | Highlights blood vessels in the retina, useful for detecting vasculitis |
The Role of Ophthalmologists in Arthritis Care
Ophthalmologists are vital in treating eye problems linked to arthritis. They team up with rheumatologists for better care. Early action helps a lot.
Good treatment for eye issues in rheumatoid arthritis needs teamwork. Rheumatologists and ophthalmologists work together. This way, they can tackle both joint and eye problems, making life better for patients.
Medical Treatments for Arthritis-Related Eye Conditions
Dealing with arthritis-related eye issues needs a mix of treatments to fight inflammation and stop damage. It’s key to manage rheumatoid arthritis (RA) well to avoid eye problems.
Prescription Eye Drops and Lubricants for Dry Eye
Dry eye is common in people with rheumatoid arthritis. Eye drops and lubricants are important for dry eye relief. They include:
- Cyclosporine eye drops to reduce inflammation
- Lifitegrast eye drops to increase tear production
- Artificial tears to lubricate the eyes
Anti-inflammatory Medications for Scleritis and Uveitis
Scleritis and uveitis are eye problems linked to RA. Anti-inflammatory meds are used to treat them.
Doctors might prescribe eye drops, ophthalmic, or systemic corticosteroids for eye inflammation. Sometimes, non-steroidal anti-inflammatory drugs (NSAIDs) are used too.
Condition | Treatment Options |
Scleritis | Oral NSAIDs, Corticosteroids |
Uveitis | Corticosteroid eye drops, Immunosuppressive therapy |
Immunosuppressive Therapies That Target Both Joint and Eye Inflammation
When arthritis and eye inflammation happen together, immunosuppressive therapies can help. They work by controlling the immune system’s overactive response.
This reduces inflammation in both joints and eyes.
Biologics and Their Role in Preventing Eye Complications
Biologic meds have changed how we treat RA and eye issues. They target specific molecules to fight inflammation and prevent eye problems.
Biologics like TNF-alpha inhibitors and other targeted therapies are used.
By using these treatments, we can manage arthritis-related eye conditions better. This improves patients’ quality of life.
Surgical Interventions for Severe Eye Complications
For people with arthritis, severe eye problems can be treated with surgery. When other treatments don’t work, surgery is needed. We’ll look at surgeries for dry eye, corneal transplant, and retinal issues.
Punctal Plugs and Other Procedures for Dry Eye
Punctal plugs are a common treatment for dry eye in arthritis patients. These small devices block tear drainage, keeping tears on the eye. Other treatments, like tear duct cauterization, also help reduce tear loss.
These methods help keep tears in, easing dry eye symptoms. Punctal plugs are a simple solution that greatly improves life for those with severe dry eye.
Corneal Transplantation for Advanced Keratitis
When keratitis gets worse, a corneal transplant might be needed. This surgery replaces the damaged cornea with healthy tissue from a donor. It can fix vision and stop pain from advanced keratitis.
The success of this surgery depends on the patient’s eye health and other conditions. Advances in surgery have made corneal transplants more successful, giving hope to those with severe keratitis.
Surgical Procedure | Indication | Benefits |
Punctal Plugs | Dry Eye Syndrome | Conserves tears, alleviates dry eye symptoms |
Corneal Transplantation | Advanced Keratitis | Restores vision, alleviates pain |
Vitrectomy | Retinal Complications | Removes vitreous gel, addresses retinal detachment or inflammation |
Vitrectomy and Other Surgeries for Retinal Complications
Vitrectomy is a surgery for retinal problems in arthritis patients. It removes the vitreous gel to treat detachment, inflammation, or other issues.
Vitrectomy can be very effective in treating retinal problems. It helps keep vision and prevents more damage. The choice to have vitrectomy comes after trying other treatments.
Self-Care Strategies for Managing Eye Symptoms
Arthritis patients can ease eye symptoms with simple self-care routines. Taking care of your eyes is key to feeling good, even with arthritis.
Daily Eye Care Routines for Arthritis Patients
Starting a daily eye care routine can help manage arthritis-related eye symptoms. Warm compresses can clear blockages in the meibomian glands. Gently cleaning the eyelids with special products can prevent infections and boost tear production.
Also, regularly blinking and taking breaks from reading or screens can prevent eye strain. Using lubricating eye drops can keep tears flowing all day.
Environmental Modifications to Reduce Eye Strain
Changing your environment can also help manage eye symptoms. Adjusting the lighting to reduce glare on screens can ease eye strain. Using a humidifier can add moisture, helping with dry eye.
Positioning digital devices at a comfortable distance and angle can also reduce eye strain. These changes can make your environment more eye-friendly.
Nutritional Approaches to Support Eye Health
Eating a balanced diet is essential for eye health. Foods rich in omega-3 fatty acids, like salmon and flaxseeds, fight inflammation. This can help with arthritis and eye health.
Adding antioxidant-rich foods like leafy greens, berries, and nuts to your diet can protect your eyes. Drinking plenty of water is also important for tear production and eye health.
By following these self-care tips, people with arthritis can manage their eye symptoms better. This can greatly improve their quality of life.
Quality of Life Impact and Emotional Aspects
Managing rheumatoid arthritis (RA) means taking care of your joints and eyes. Eye problems can really affect how you feel. They can change your daily life, making it harder to be independent and enjoy life.
Coping with Vision Changes and Limitations
Dealing with vision changes from RA eye problems needs a big effort. You have to adjust to new challenges while keeping your spirits up. Simple things can become hard, causing frustration and feeling left out.
To handle these changes well, consider the following:
- Seeking support from family and friends
- Engaging in low-vision rehabilitation programs
- Using assistive devices to aid daily tasks
Support Resources for Patients with Eye Complications
It’s important to have the right support when dealing with RA eye problems. These resources offer emotional help, practical tips, and medical advice.
Some great resources include:
Resource | Description |
Patient Support Groups | Online or in-person groups where patients can share experiences and advice |
Ophthalmological Services | Specialized eye care services for diagnosis and treatment of eye complications |
Low-Vision Rehabilitation | Programs to help patients adapt to vision loss and maintain independence |
Communicating Eye Symptoms to Healthcare Providers
Talking clearly with your healthcare team is key to managing RA eye problems. Be ready to share your symptoms in detail.
Key points to discuss with your healthcare provider:
- Any changes in vision or eye comfort
- Symptoms such as redness, pain, or discharge
- Any medications or treatments currently being used for eye care
By keeping the lines of communication open and using available support, patients can manage the effects of RA eye problems better. This helps improve their quality of life.
Conclusion: Living Well with Arthritis and Protecting Your Vision
Managing arthritis means taking care of your joints and your eyes. Knowing how rheumatoid arthritis (RA) affects your eyes is key. This knowledge helps you protect your vision.
Spotting eye problems early and treating them right is important. Regular eye checks and special tests help catch issues before they get worse.
There are many ways to keep your eyes healthy. Simple eye care, making your environment better for your eyes, and eating right are all helpful. Working with your doctor helps you manage your arthritis and keep your life good.
Looking after your vision is a big part of living well with arthritis. We urge patients to stay up to date with their health, see doctors often, and take steps to keep their eyes and overall health in top shape.
FAQ
Can rheumatoid arthritis cause eye problems?
Yes, rheumatoid arthritis can lead to eye issues. These include dry eye, episcleritis, scleritis, and other inflammatory conditions. These can affect your vision and eye health.
What are the symptoms of arthritis in the eyes?
Symptoms include dryness, redness, and pain. You might also feel sensitive to light or have blurred vision. In severe cases, vision loss can occur.
How is arthritis-related eye disease diagnosed?
Doctors use eye exams to diagnose. They check your vision and use a slit-lamp to examine your eyes. They might also do tests to see how much your eyes are affected.
What treatments are available for arthritis-related eye conditions?
Treatments vary. For dry eye, you might get eye drops. For more serious conditions, doctors might prescribe anti-inflammatory drugs or biologics. In some cases, surgery is needed.
Can arthritis in the eyes be prevented?
While prevention is not complete, managing rheumatoid arthritis well can help. A healthy lifestyle and regular eye exams can also reduce eye risks.
How does secondary Sjögren’s syndrome affect eye health?
Secondary Sjögren’s syndrome can cause dry eye due to tear gland problems. This can lead to severe complications if not treated.
What self-care strategies can help manage eye symptoms?
Daily eye care routines and environmental changes can help. Using humidifiers and taking breaks from screens are good. Eating foods rich in omega-3 fatty acids also supports eye health.
When should I seek emergency medical attention for eye symptoms?
Get help right away for sudden vision loss, severe pain, or increased light sensitivity. Any sudden and severe eye symptoms need immediate attention.
How can I communicate my eye symptoms effectively to my healthcare provider?
Describe your symptoms in detail. Talk about when they started and how they affect you. Keeping a symptom journal can help.
Are there support resources available for patients with arthritis-related eye complications?
Yes, many resources are available. Patient organizations, online forums, and counseling services offer support. They help with managing eye complications and daily life.
References
National Center for Biotechnology Information. Epiretinal Membrane Surgery: Retinal Peeling for Macular Pucker. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7127775/








