Knowing the facial nerve and its five branches is key for doctors and those recovering from face injuries.facial nerve branchesCarotid Procedure: 7 Key Facts About CEA Surgery & Risks
The facial nerve is a marvel of nature. It controls movement, senses, and autonomic functions all in one nerve.
The five branches – temporal, zygomatic, buccal, marginal mandibular, and cervical – control the muscles of human expression and sensation.
Understanding these branches helps us diagnose and treat facial nerve disorders better.
Key Takeaways
- The facial nerve has five terminal branches.
- These branches innervate muscles of facial expression.
- Understanding the anatomy is key for diagnosis and treatment.
- The facial nerve combines motor, sensory, and autonomic functions.
- Disorders related to the facial nerve can be effectively managed with proper knowledge.
The Facial Nerve: Structure and Function
It’s key to know about the facial nerve’s structure and function. This helps us understand its role in our facial expressions and health. The facial nerve, or cranial nerve VII, is complex and vital for many facial functions.
Cranial Nerve VII Classification
The facial nerve is known as cranial nerve VII. It’s one of the 12 cranial nerves from the brain. It’s special because it has both motor and sensory fibers.
Motor, Sensory, and Parasympathetic Components
The facial nerve has three main parts: motor, sensory, and parasympathetic. The motor component controls facial muscles. This lets us show emotions through our face. The sensory component sends taste signals from the tongue’s front two-thirds. The parasympathetic component helps control gland secretions, like saliva.
Role in Facial Expression and Physiological Functions
The facial nerve is key for facial expressions, which are important for communication. It also helps with taste and gland secretions. This shows how complex and important the facial nerve is for our health.
Learning about the facial nerve’s structure and function helps us see its value in our lives. It’s why keeping it healthy is so important.
Anatomical Course of the Facial Nerve
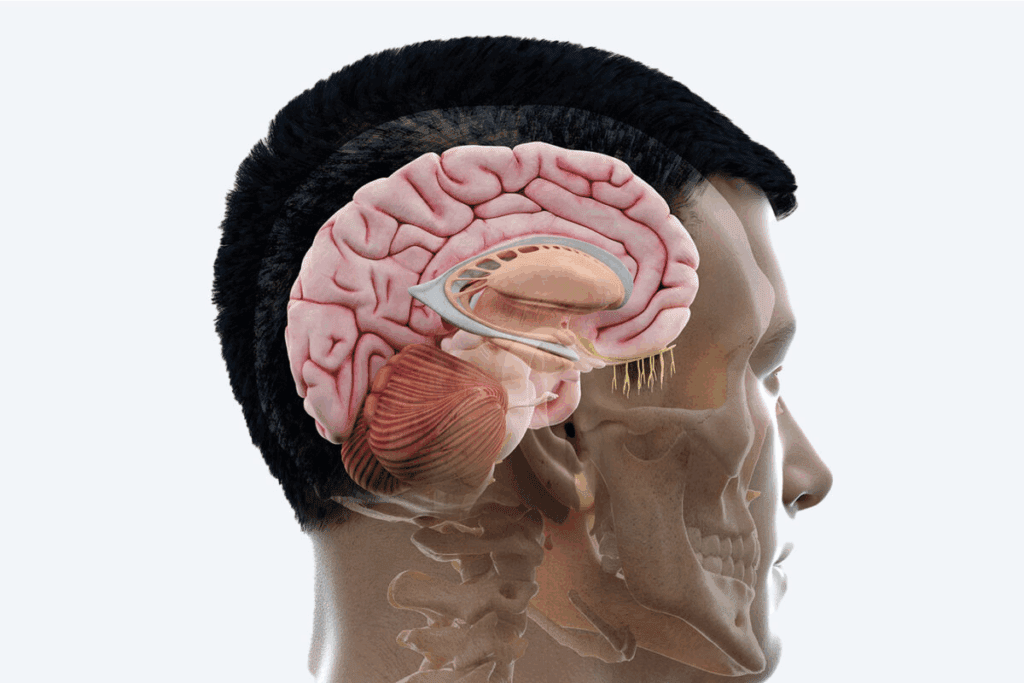
The facial nerve’s path is complex, spanning from the brainstem to the face. It goes through several segments. Knowing this helps us understand its role and where problems might occur.
Intracranial Segment
The facial nerve starts at the brainstem, at the pontomedullary junction. This intracranial segment is the first part of its journey. It’s near other cranial nerves. Then, it goes into the internal auditory canal, starting its journey through the temporal bone.
Intratemporal Segment
The nerve then moves into the intratemporal segment. It goes through the facial canal in the temporal bone. This part is key because the nerve is close to bones and can get damaged or compressed. It also branches off, including the greater petrosal nerve, which helps the lacrimal gland and nasal mucosa.
The nerve’s path through the temporal bone is complex. It has several bends or geniculations. The first geniculum is near the geniculate ganglion, where the nerve’s sensory fibers are found.
Extracranial Segment
After leaving the skull through the stylomastoid foramen, the nerve enters its extracranial segment. Here, it branches off to the muscles of facial expression. This part is more exposed and can easily get hurt, like in the parotid gland area.
The nerve’s branching in this segment is complex. It has many branches that work together to create facial expressions. Knowing this is key for doctors and surgeons to treat facial nerve problems.
In conclusion, the facial nerve’s path is complex, with intracranial, intratemporal, and extracranial segments. Each part has its own features and importance. Understanding the nerve’s anatomy is vital for health and treating diseases.
Facial Nerve Branches: Distribution and Innervation
The facial nerve branches are key to our facial expressions. Knowing how they spread out and what they connect to is vital. The facial nerve, or cranial nerve VII, splits into several branches. These branches reach out to different muscles and glands in our face.
Branching Pattern Overview
The facial nerve splits into five main branches: temporal, zygomatic, buccal, marginal mandibular, and cervical. These branches come from the parotid plexus, a network of nerve fibers. They emerge from the stylomastoid foramen.
The way the facial nerve branches out varies from person to person. Knowing this is important for doctors and surgeons. They need to understand this when they operate on the face.
Innervation of Facial Expression Muscles
The main job of the facial nerve branches is to control the muscles of facial expression. These muscles let us move our face. The facial nerve connects to muscles like the frontalis, orbicularis oculi, and zygomaticus major.
Branch | Muscles Innervated |
Temporal | Frontalis, orbicularis oculi |
Zygomatic | Orbicularis oculi, zygomaticus major |
Buccal | Buccinator, muscles of the upper lip |
Marginal Mandibular | Muscles of the lower lip |
Cervical | Platysma |
Topographical Anatomy of Distribution
The facial nerve branches’ paths are complex. Each branch has its own route and area it covers. For example, the temporal branch goes up to reach the frontalis muscle. The cervical branch goes down to reach the platysma.
Knowing the facial nerve branches’ paths is key for diagnosing and treating face problems. Doctors need to understand where damage can happen. They also need to know what problems such damage can cause.
Temporal Branch: Anatomy and Function
Knowing how the temporal branch works is key to spotting facial nerve problems. This branch is a part of the facial nerve and helps control our facial expressions. It mainly affects the forehead and eye area.
Anatomical Course and Relations
The temporal branch starts in the parotid gland and goes up. It crosses the zygomatic arch to reach the forehead and eye muscles. The path of the temporal branch is complex and can change, which might affect its work and how it gets hurt.
“The temporal branch of the facial nerve is at risk during surgeries in the temporal area,” medical texts say. This is because it’s close to the surface and not very big.
Muscles Innervated
The main muscles the temporal branch controls are the frontalis, orbicularis oculi, and sometimes the procerus and corrugator supercilii. These muscles help us show different facial expressions, like raising our eyebrows or closing our eyes.
- Frontalis muscle: raises the eyebrows
- Orbicularis oculi muscle: helps close the eyes and blink
- Procerus and corrugator supercilii muscles: help us frown and move our eyebrows
Clinical Significance of Temporal Branch Injury
Damage to the temporal branch can cause big problems. It can make the muscles it controls weak or paralyzed. This can make it hard to close our eyes fully or lift our eyebrows, which affects how we look and can lead to eye problems.
Checking how well the temporal branch works is important. Doctors look at how well patients can move their face, like raising their eyebrows or closing their eyes tight. Knowing how serious a temporal branch injury is helps doctors plan the best treatment.
As experts, we know how important it is to understand the temporal branch. This knowledge helps us diagnose and treat facial nerve issues better. It lets us give our patients the best care possible.
Zygomatic Branch: Anatomy and Function
The facial nerve’s zygomatic branch is key for controlling facial expressions around the eye. It innervates the orbicularis oculi muscle. We will look at its anatomy, the muscles it affects, and what happens if it’s damaged.
Anatomical Course and Relations
The zygomatic branch starts from the facial nerve after it leaves the stylomastoid foramen. It moves forward, crossing the zygomatic bone to get to the orbicularis oculi muscle. “Knowing the zygomatic branch’s path is key to understanding its role and how it can be hurt,” say facial anatomy experts.
Muscles Innervated
The main muscle the zygomatic branch controls is the orbicularis oculi. This muscle closes the eye and is vital for facial expressions. The branch’s nerve supply ensures the eye’s movements are smooth and controlled.
Clinical Significance of Zygomatic Branch Injury
Damage to the zygomatic branch can weaken or paralyze the orbicularis oculi muscle. This makes it hard to close the eye and can harm eye protection. Checking the zygomatic branch’s function is key in diagnosing and treating facial nerve problems. Knowing how important it is helps doctors plan the best treatment to avoid lasting damage to facial expressions and eye safety.
The zygomatic branch is a vital part of the facial nerve. Its problems can lead to serious issues. By understanding its role, we can better manage facial expressions and treat injuries or diseases effectively.
Buccal Branch: Anatomy and Function
The buccal branch of the facial nerve is key for facial expressions, mainly in the cheek. It’s one of the five branches of the facial nerve. It helps control muscles for different facial movements.
Anatomical Course and Relations
The buccal branch starts from the facial nerve in the parotid gland and moves forward. It runs along the masseter muscle’s surface. It’s near the parotid duct and the buccal fat pad. Knowing its path is important for surgeons to avoid mistakes.
Muscles Innervated
The buccal branch controls muscles like the buccinator muscle. This muscle helps press the cheek against the teeth and is used when blowing. It also helps in making facial expressions like smiling and puckering.
As “The buccal branch is critical for the motor innervation of the buccinator and other facial muscles”, shows its vital role in facial functions (1).
Clinical Significance of Buccal Branch Injury
An injury to the buccal branch can cause muscle weakness. This makes it hard to blow or whistle. It can also lead to facial asymmetry during expressions.
A study found that
“Damage to the buccal branch of the facial nerve can lead to significant morbidity, including facial asymmetry and functional impairments”
. This highlights the need for careful diagnosis and treatment of such injuries (2).
Understanding the buccal branch’s role in facial expressions is key when dealing with facial nerve issues. Knowing its anatomy and function helps in creating effective treatment plans.
Marginal Mandibular Branch: Anatomy and Function
The marginal mandibular branch is a key part of the facial nerve. It controls muscles in the lower lip and chin. This branch is vital for making facial expressions like smiling and frowning.
Anatomical Course and Relations
The marginal mandibular branch starts from the facial nerve. It goes forward, below the jaw, to reach the muscles of the lower lip and chin. Its path is close to the jaw and the platysma muscle.
Muscles Innervated
This branch controls several important muscles. These include the depressor anguli oris, depressor labii inferioris, and mentalis muscles. These muscles help move the lower lip and chin, allowing for different facial expressions.
Clinical Significance of Marginal Mandibular Branch Injury
An injury to this branch can cause serious facial problems. It can lead to weakness or paralysis of the muscles it controls. This makes it hard to move the lower lip and affects how we show emotions.
Knowing how the marginal mandibular branch works is key for doctors. They need to understand the risks of injury during neck and face surgeries.
Cervical Branch: Anatomy and Function
The cervical branch is the last part of the facial nerve. It’s key for controlling the platysma muscle. This muscle helps with facial expressions and neck movements.
Anatomical Course and Relations
The cervical branch starts in the parotid gland and goes down. It crosses or goes through the sternocleidomastoid muscle. It then reaches the platysma muscle, which it controls.
Knowing the cervical branch’s path is vital for neck surgeries. Damage can cause serious problems. Its path shows how complex facial nerve anatomy is. This makes precise knowledge during surgeries important.
Muscles Innervated
The main muscle the cervical branch controls is the platysma. This muscle helps with facial expressions, like the lower lip. It also helps with neck skin tension.
The platysma’s role is often overlooked, but it’s key for facial and neck movements. Its connection to the cervical branch shows how important this nerve is for facial functions.
Clinical Significance of Cervical Branch Injury
Damage to the cervical branch can weaken the platysma muscle. This can change facial expressions and the neck’s look. Knowing about the cervical branch’s importance is key for treating facial nerve injuries or neck surgeries.
“Damage to the cervical branch can have lasting effects on a patient’s quality of life, stressing the need for careful consideration during surgical planning and execution.” – This shows why keeping the cervical branch safe during surgeries is critical.
Injuries to the cervical branch have big clinical implications. Understanding its anatomy and function is essential. This knowledge helps healthcare providers manage facial nerve issues and improve patient care.
Clinical Assessment and Pathologies
Understanding facial nerve damage is key for good patient care. The facial nerve’s complex role and wide reach make it prone to many problems. These issues can greatly affect a patient’s life quality.
Facial Nerve Examination Techniques
We employ several methods to check the facial nerve. We look at facial muscle strength, taste, and the corneal reflex. A detailed check helps us see how much and what kind of nerve damage there is.
Facial muscle strength is tested by asking patients to make different facial expressions. This shows if there’s weakness or paralysis.
Common Facial Nerve Pathologies
Many conditions can harm the facial nerve, like Bell’s palsy, injuries, and infections like Ramsay Hunt syndrome. Each one brings its own set of challenges in finding and treating the problem.
Pathology | Characteristics | Management |
Bell’s Palsy | Idiopathic facial paralysis | Corticosteroids, antiviral therapy |
Traumatic Injury | Facial paralysis due to trauma | Surgical repair, rehabilitation |
Ramsay Hunt Syndrome | Herpes zoster infection | Antiviral therapy, pain management |
Surgical Considerations and Anatomical Variations
When we operate on facial nerve problems, knowing the nerve’s anatomy is vital. We plan carefully before surgery and watch closely during it to ensure success.
There can be variations in the facial nerve’s anatomy, like extra branches. We must think about these when we plan surgery. This helps us avoid complications.
Conclusion
The facial nerve is complex and vital for our facial expressions and other functions. We’ve looked at its anatomy and how it spreads out. It has five main branches: temporal, zygomatic, buccal, marginal mandibular, and cervical.
Knowing about the facial nerve’s branches is key for diagnosing and treating nerve disorders. Each branch has its own role and injury can have serious effects. This shows how important it is to understand this well.
In summary, knowing the facial nerve and its branches is essential for good patient care. We’ve seen how its structure and spread are linked to its function. This knowledge helps doctors in their work. By reviewing the main points, we highlight the facial nerve’s role in our expressions and other functions. This stresses the need for ongoing learning and research in this area.
FAQ
What are the 5 branches of the facial nerve?
The facial nerve has five main branches. These are the temporal, zygomatic, buccal, marginal mandibular, and cervical. They control the muscles of facial expression.
What is the function of the facial nerve?
The facial nerve controls our facial expressions. It also transmits taste and regulates gland secretions. This is through its motor, sensory, and parasympathetic fibers.
Where does the facial nerve exit the skull?
The facial nerve leaves the skull through the stylomastoid foramen.
What is the role of the temporal branch of the facial nerve?
The temporal branch controls muscles for eyebrow movement and eye closure. It has other functions too.
What is the clinical significance of the zygomatic branch?
The zygomatic branch is key for facial expressions, mainly around the eye. Damage can cause big facial problems.
What muscles are innervated by the buccal branch?
The buccal branch controls facial expressions in the cheek area. It innervates specific muscles.
What is the function of the marginal mandibular branch?
The marginal mandibular branch manages lower lip and chin movements. Damage can lead to facial dysfunction.
What is the role of the cervical branch?
The cervical branch controls the platysma muscle. This muscle is involved in neck and facial movements.
How is facial nerve function assessed clinically?
Clinicians check facial nerve function by examining facial expressions, muscle strength, and reflexes.
What are some common pathologies affecting the facial nerve?
Facial nerve problems include Bell’s palsy, paralysis, and injuries from trauma.
What are the surgical considerations for facial nerve surgery?
Surgery for the facial nerve must consider anatomical variations and nerve injury. It also looks at post-operative risks.
What is the innervation of the face?
The face is innervated by the facial nerve. It controls facial muscles and provides sensory innervation.
What is the distribution of the facial nerve branches?
Facial nerve branches spread across the face. Each branch controls specific facial muscles.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/15368081/