Many women around the world face dyspareunia, or pain during or after sex. If you’re wondering if it’s normal to hurt after sex, you’re not alone.
Talking about pain after sex can be tough. But it’s a key step to feeling better. The reasons for this pain vary, from hormonal issues to infections and structural problems.
We’re dedicated to providing top-notch healthcare info, including support for international patients. In this guide, we’ll look at why pain occurs after sexual intercourse. We’ll cover the medical reasons and offer help to those affected.
Female pain after intercourse is alarming. Discover 7 shocking causes, from simple issues to serious conditions, and learn how to get relief.
Key Takeaways
- Dyspareunia, or pain during or after sex, is a common issue affecting millions worldwide.
- The causes of pain after sex are varied, including hormonal, infectious, and structural factors.
- Understanding the underlying cause is key to finding the right treatment.
- Talking about pain after sex with a healthcare provider is a big step towards relief.
- Comprehensive support is available for international patients seeking healthcare solutions.
Understanding Female Pain After Intercourse (Dyspareunia)
Pain during or after sex, known as dyspareunia, is more common than you might think. It affects a big number of women worldwide. This condition impacts their sexual health and overall well-being.
What Is Dyspareunia?
Dyspareunia is when you feel persistent or recurring pain before, during, or after sex. This pain can happen in different places. It might be at the vaginal entrance, deep in the pelvis, or inside the vaginal canal.
How Common Is Post-Coital Pain?
Research shows that dyspareunia affects 10 to 28 percent of women globally. The exact number can change based on age, health, and other factors. There are two main types of dyspareunia. Superficial dyspareunia causes pain at the vaginal entrance. Deep dyspareunia leads to deep pelvic pain during sex.
Prevalence of Dyspareunia | Age Group |
10-15% | 18-30 years |
15-20% | 31-45 years |
20-28% | 46-60 years |
When to Seek Medical Attention
If you have persistent or severe pain during or after sex, you should see a doctor. Signs that mean you need to see a doctor include:
- Pain that lasts for more than a few days
- Pain with bleeding or unusual discharge
- Pain that gets worse over time
- Difficulty getting aroused or reaching orgasm
Getting diagnosed and treated early can greatly improve your sexual health and life quality.
Physical Causes of Pain After Sex
Pain after sex is more common than you might think. There are several physical reasons for this. We will explore these causes in detail to help you understand your discomfort.
Vaginal Dryness and Inadequate Lubrication
Vaginal dryness is a big reason for pain during and after sex. It can happen due to hormonal changes, like during menopause, or because of certain medicines. Inadequate lubrication also causes friction, leading to discomfort or pain.
To help with vaginal dryness, using lubricants is a good idea. There are many types, like water-based, silicone-based, and oil-based. It’s important to pick one that fits your needs and likes.
Vaginal Infections and Inflammation
Vaginal infections are another common cause of pain after sex. Infections like yeast infections and bacterial vaginosis can cause inflammation and irritation. This leads to discomfort.
- Yeast infections are known for itching, burning, and a thick, white discharge.
- Bacterial vaginosis causes a thin, gray or white discharge with a fishy smell.
Both conditions need medical attention for proper diagnosis and treatment. Yeast infections are treated with antifungal meds. Bacterial vaginosis is treated with antibiotics.
Structural Issues in the Reproductive System
Structural issues in the reproductive system can also cause pain after sex. Conditions like endometriosis, fibroids, or abnormalities in the uterus or vagina can cause discomfort during or after sex.
If you think a structural issue is causing your pain, it’s important to see a healthcare provider. They can do a thorough examination and run tests to find the cause.
Hormonal Factors Contributing to Post-Coital Discomfort
Understanding how hormones affect female sexual health is key to solving post-coital pain. Hormonal changes can greatly impact a woman’s comfort during and after sex. These shifts happen at different life stages, like menopause, while using hormonal birth control, and after having a baby.
Menopause and Estrogen Deficiency
Menopause brings big changes in a woman’s hormones, mainly a drop in estrogen. Estrogen deficiency can cause vaginal dryness, known as vaginal atrophy. This leads to pain during and after sex. We’ll look into how hormone replacement therapy (HRT) and other treatments can help.
Hormonal Contraception Effects
Hormonal birth control is great for preventing pregnancy but can affect sexual comfort. Some women might see changes in their sex drive or vaginal lubrication because of the hormones. We’ll talk about the different types of hormonal birth control and their effects on sex health.
Postpartum Hormonal Changes
The postpartum period sees big hormonal shifts as the body adjusts after pregnancy. Decreased estrogen levels can cause vaginal dryness, and physical changes after childbirth can also lead to discomfort during sex. We’ll look into how postpartum women can manage these changes to feel better during sex.
Infections That Cause Pain After Intercourse
It’s important to know how infections can lead to pain after sex. We’ll look at common causes like Urinary Tract Infections (UTIs), Sexually Transmitted Infections (STIs), yeast infections, and bacterial vaginosis.
Urinary Tract Infections (UTIs)
UTIs happen when bacteria infect the urinary tract. Symptoms include burning while urinating, needing to urinate often, and pain in the lower abdomen. These infections can make sex painful because of the irritation and inflammation they cause.
Treatment: Doctors usually treat UTIs with antibiotics. Drinking lots of water and urinating after sex can help prevent them.
Sexually Transmitted Infections (STIs)
STIs, like chlamydia and gonorrhea, can cause pain during sex. They can also lead to serious problems like pelvic inflammatory disease if not treated. Symptoms include abnormal discharge, painful urination, and pelvic pain.
Treatment: STIs are treated with antibiotics or antiviral medications. It’s important to practice safe sex and get regular STI checks to prevent them.
Yeast Infections and Bacterial Vaginosis
Yeast infections happen when there’s too much Candida fungus. They cause itching, burning, and a thick, white discharge. Bacterial vaginosis is caused by an imbalance of vaginal bacteria, leading to discharge and odor. Both can make sex uncomfortable.
Treatment: Yeast infections are treated with antifungal medications, while bacterial vaginosis is treated with antibiotics. Keeping good hygiene and avoiding douching can help prevent these infections.
Infection | Common Symptoms | Treatment |
UTIs | Burning during urination, frequent urination, lower abdominal pain | Antibiotics |
STIs | Abnormal discharge, painful urination, pelvic pain | Antibiotics or antiviral medications |
Yeast Infections | Itching, burning, thick, white discharge | Antifungal medications |
Bacterial Vaginosis | Discharge, odor | Antibiotics |
Gynecological Conditions Associated with Post-Sex Pain
Pain after sex can be a sign of many gynecological issues. These issues can affect sexual health, causing discomfort. We will look at some of these conditions and their effects.
Endometriosis
Endometriosis is when tissue like the uterus lining grows outside the uterus. This causes pain and discomfort. The misplaced tissue can lead to inflammation and scarring, making sex painful.
Symptoms of endometriosis include:
- Pelvic pain or cramping
- Painful periods
- Pain during or after sex
- Infertility or difficulty getting pregnant
Pelvic Inflammatory Disease (PID)
PID is an infection of the female reproductive organs. It’s often caused by bacteria from sexual contact. PID can cause pain during and after sex, along with symptoms like abnormal vaginal discharge and fever.
Risk factors for PID include:
- Having multiple sexual partners
- Having a history of STIs
- Using an intrauterine device (IUD) for contraception
Ovarian Cysts and Fibroids
Ovarian cysts are fluid-filled sacs on the ovaries. Fibroids are non-cancerous growths in or around the uterus. Both can cause pelvic pain, which can get worse during sex.
Condition | Common Symptoms | Potential Complications |
Endometriosis | Pelvic pain, painful periods, pain during sex | Infertility, ovarian cysts |
PID | Pelvic pain, abnormal discharge, fever | Infertility, chronic pelvic pain |
Ovarian Cysts | Pelvic pain, bloating, irregular periods | Cyst rupture, torsion |
Fibroids | Heavy or painful periods, pelvic pressure | Infertility, pregnancy complications |
It’s important to understand these gynecological conditions to address post-sex pain. Each condition has its own symptoms and complications. This highlights the need for proper diagnosis and treatment.
Psychological and Emotional Factors
The link between sex and pain is complex, involving both physical and deep emotional aspects. While physical reasons are often looked at, the emotional and psychological sides also play a big role in pain after sex.
Anxiety and Stress
Anxiety and stress can make sex uncomfortable or painful. When we’re stressed or anxious, our body tightens up, causing pain in the pelvic area.
Stress and anxiety can also change our hormone levels, leading to vaginal dryness. This dryness can make sex uncomfortable. Relaxation techniques like deep breathing or meditation can help manage stress and reduce pain.
Key Points to Consider:
- Stress management techniques can help reduce anxiety-related pain during sex.
- Open communication with partners about stress and anxiety can improve sexual comfort.
- Seeking professional help for anxiety can be beneficial in addressing related sexual health issues.
Past Trauma and Vaginismus
Past traumatic experiences, like sexual abuse, can cause pain after sex. This is due to the emotional and psychological impact on a person’s sexual health. Vaginismus, a condition where the vaginal muscles tighten involuntarily, can also result from past trauma, making sex painful or impossible.
“Trauma can affect a person’s ability to relax and enjoy sex, leading to pain and discomfort.”
Dealing with past trauma often needs professional help, like therapy and counseling. Techniques such as cognitive-behavioral therapy (CBT) and desensitization exercises can help manage vaginismus and reduce pain from past trauma.
Condition | Symptoms | Treatment Options |
Vaginismus | Involuntary vaginal muscle tightening, pain during sex | Physical therapy, CBT, desensitization exercises |
Past Trauma | Pain during sex, flashbacks, anxiety | Therapy, counseling, support groups |
Relationship Issues Affecting Sexual Comfort
Relationship dynamics are key to sexual health. Problems like poor communication, trust issues, or emotional distance can cause tension and stress, leading to pain during or after sex.
Improving communication and tackling relationship issues can greatly enhance sexual comfort. Couples therapy can help resolve these problems and improve overall sexual health.
Strategies for Improvement:
- Practice open and honest communication with your partner.
- Engage in couples therapy to address underlying issues.
- Focus on building emotional intimacy and trust.
Pain in Different Locations: What It Might Mean
Pain after sex can show up in various spots, each hinting at a different issue. Knowing where the pain is helps figure out what’s causing it and how to treat it.
Deep Pelvic or Uterine Pain
Pain in the deep pelvic or uterine area can point to several gynecological problems. Endometriosis, where uterine lining grows outside, is a common culprit. Other possible causes include adenomyosis and fibroids, which are non-cancerous growths in or around the uterus.
These issues can lead to inflammation, scarring, and adhesions. This can cause pain during deep penetration. If you’re experiencing this pain, seeing a healthcare provider for a detailed check-up is key.
Vaginal Entrance Pain
Pain at the vaginal entrance, also known as vulvar pain or vaginismus, can stem from many sources. Infections like yeast infections or bacterial vaginosis can irritate and cause discomfort. Vulvodynia, a condition with chronic pain in the vulvar area without a clear cause, is another possible cause.
Allergic reactions to soaps, lotions, or latex condoms can also lead to pain at the vaginal entrance. A healthcare provider can identify the cause through a physical exam and tests.
Pain in Surrounding Areas
Sometimes, pain after sex can spread to areas around the reproductive organs, like the bladder or rectum. Urinary tract infections (UTIs) can cause pain or discomfort in the bladder or urethra. Conditions like hemorrhoids or anal fissures affecting the rectum can also cause pain.
Location of Pain | Possible Causes |
Deep Pelvic or Uterine | Endometriosis, Adenomyosis, Fibroids |
Vaginal Entrance | Vaginismus, Yeast Infections, Bacterial Vaginosis, Vulvodynia |
Surrounding Areas (Bladder, Rectum) | UTIs, Hemorrhoids, Anal Fissures |
Understanding the location and nature of pain after sex is key to finding its cause and the right treatment. If you’re experiencing ongoing or severe pain, it’s vital to talk to a healthcare provider for a proper diagnosis and care.
Diagnosing the Cause of Post-Intercourse Pain
To find out why you might feel pain after sex, doctors use a few key steps. They look at your medical history and run some tests. This helps them figure out what’s causing the pain and how to treat it.
Medical History and Physical Examination
First, doctors will ask you lots of questions about your health and sex life. They want to know about any past health issues or surgeries. Then, they’ll do a physical check to see if there’s anything wrong with your reproductive system.
Understanding your medical history is key. It helps doctors spot things like hormonal problems or past infections. They’ll also check your reproductive organs for any tenderness or abnormalities.
Laboratory Tests and Imaging
If the initial steps don’t give a clear answer, doctors might suggest more tests. These could include:
- Urine tests to check for infections
- Blood tests to check hormone levels or look for infections
- Swab tests to find out if you have a sexually transmitted infection
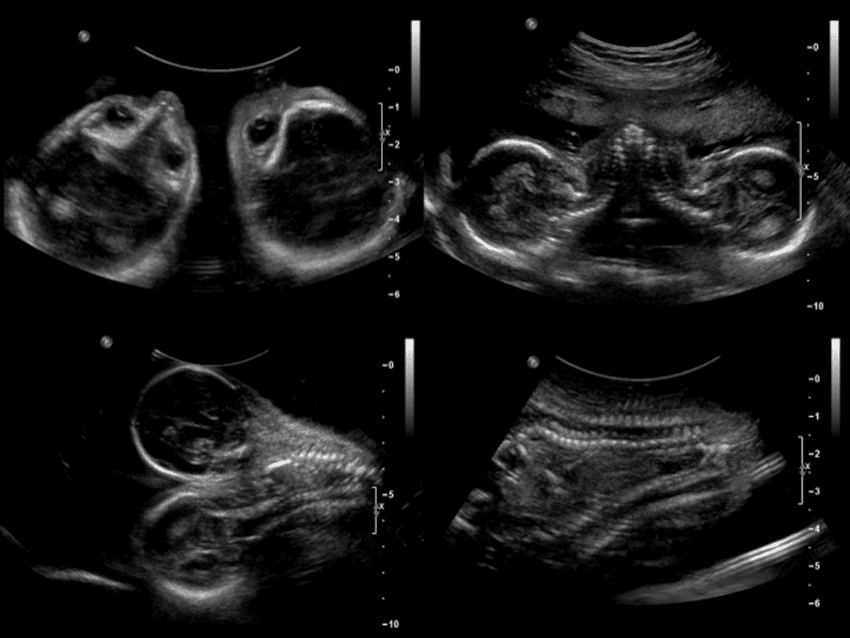
- Ultrasound or MRI to get a closer look at your reproductive organs
These tests help doctors confirm what’s going on and rule out other possibilities. For example, an ultrasound can spot things like cysts or fibroids.
Diagnostic Tool | Purpose |
Urine Test | Detects urinary tract infections |
Blood Test | Checks hormone levels and looks for infections |
Ultrasound | Looks at reproductive organs for any issues |
When to See a Specialist
If you’re in a lot of pain after sex, you should see a doctor right away. They might send you to a gynecologist if they need more information or if you need special care.
“Pain after sex is not normal and should be evaluated by a healthcare provider to determine the underlying cause and appropriate treatment.”
Getting a diagnosis and treatment early can really help. It can make you feel better and reduce your pain. By knowing what’s causing your pain, doctors can create a treatment plan just for you.
Treatment Options for Female Pain After Intercourse
Finding the right treatment for pain after sex starts with figuring out the cause. Once we know what’s causing the pain, we can create a plan to help. This plan aims to ease symptoms and improve life quality.
Medical Treatments
Medical treatments for pain after sex depend on the diagnosis. For example, if an infection is the cause, antibiotics or antifungal medications might be needed. Hormonal imbalances could require hormone replacement therapy (HRT) or estrogen therapy to balance hormones.
Women with endometriosis or pelvic inflammatory disease might need more specific treatments. These could include pain management medications, surgical interventions to remove lesions or repair tissues, and other therapies to lessen pain.
- Antibiotics for bacterial infections
- Antifungal medications for yeast infections
- Hormone therapy for hormonal imbalances
- Pain management medications for chronic pain
Self-Care Strategies
Self-care can also help with pain after sex. Using lubricants can reduce friction and discomfort, which is helpful for vaginal dryness. Practicing relaxation techniques like deep breathing, yoga, or meditation can also help by reducing anxiety and tension.
Changing your lifestyle can also help. This includes maintaining a healthy weight, exercising regularly, and avoiding irritants like scented soaps or douches that can irritate the vagina.
- Use lubricants to reduce friction
- Practice relaxation techniques to reduce anxiety
- Maintain a healthy lifestyle through diet and exercise
- Avoid irritants that can cause vaginal dryness or irritation
Combining medical treatments with self-care can help women find relief from pain after sex. It’s important to work with a healthcare provider to find the best treatment plan for your specific situation.
Prevention Strategies for Reducing Post-Coital Pain
To avoid pain after sex, it’s important to talk openly, try new ways of being intimate, and get regular health checks. These steps can greatly lower the chance of pain and improve your sex life.
Communication with Partners
Talking openly with your partner is key to avoiding pain after sex. It’s important to share what feels good and what doesn’t. Mutual understanding and respect help make sure both partners feel safe and comfortable.
Here are some tips for better communication:
- Discuss what feels good and what doesn’t
- Share any discomfort or pain during or after sex
- Try different sexual techniques and positions together
Sexual Techniques and Positions
Choosing comfortable sexual techniques and positions can help avoid pain. Trying different positions can help find what works best for you and your partner. For example, positions that let you control the depth and angle can be very helpful.
Sexual Position | Benefits |
Female-on-top position | Allows for control over depth and angle of penetration |
Spooning position | Can be comfortable for those experiencing deep pelvic pain |
Missionary position with a pillow under the hips | Can help adjust the angle of penetration |
Regular Gynecological Check-ups
Regular visits to the gynecologist are vital for preventing pain after sex. These visits help catch and treat problems like infections and hormonal imbalances early.
Talking about any symptoms or worries with your doctor can lead to quick help. Regular check-ups are a smart way to keep your sex life healthy and pain-free.
Conclusion: Addressing Pain After Sex for Better Sexual Health
It’s important to tackle pain after sex to boost sexual health and overall well-being. We’ve looked at why women might feel pain after sex. This includes physical, hormonal, and psychological reasons. Knowing these causes is the first step to finding the right treatment.
By understanding the complexity of pain after sex, we can help each other more. Talking openly with doctors and partners is vital. We urge everyone to look after their sexual health by getting medical help when needed and using prevention methods.
Fixing pain after sex is key to healthy relationships and a better life. We stress the need for a full approach to sexual health. This includes medical care, self-care, and open talks.
FAQ
What is dyspareunia?
Dyspareunia is a medical term for pain during or after sex. It’s a common issue for many women worldwide. Knowing what it is helps you find the right help.
Is it normal to experience pain after sex?
Some discomfort after sex is normal. But, if the pain is constant or very bad, you should see a doctor. They can find out why you’re feeling pain.
What are the common physical causes of pain after sex?
Physical reasons include vaginal dryness and infections like UTIs and STIs. Also, issues like endometriosis and fibroids can cause pain.
How do hormonal changes affect sexual health?
Hormonal shifts during menopause or after pregnancy can cause vaginal dryness. This can make sex uncomfortable. Knowing about these changes helps manage symptoms.
Can psychological factors contribute to pain after sex?
Yes, stress, anxiety, past trauma, and relationship problems can affect sex. They can cause pain during or after sex.
How is the cause of pain after sex diagnosed?
Doctors use a detailed medical history and physical exam. They might also do tests and imaging to find the cause.
What are the treatment options for pain after sex?
Treatment depends on the cause. It can include medicine, like hormones or antibiotics. Self-care like using lubricants and relaxing also helps.
How can pain after sex be prevented?
To prevent pain, talk openly with your partner. Try different positions and go to regular check-ups. This can help avoid pain after sex.
Why does it hurt after having intercourse?
Pain can come from physical issues, hormonal changes, or emotional factors. Knowing the cause helps find a solution.
What does pain in different locations during or after sex indicate?
Pain location can point to different problems. For example, deep pain might mean endometriosis. Vaginal pain could be from dryness or infections.
When should I seek medical attention for pain after sex?
See a doctor if the pain is ongoing, severe, or with other symptoms like unusual discharge or fever. These signs might mean you need medical help.
References
National Center for Biotechnology Information. Dyspareunia: Common Causes of Pain After Intercourse. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK562159/