Dealing with aortic aneurysm treatments can feel overwhelming. That’s why we’re here to help you understand the FEVAR procedure. It’s a modern, less invasive method. Learn 7 key facts about the FEVAR procedure, aortic stents, EVAR surgery, and endoleaks.
The FEVAR procedure uses special stent grafts with fenestrations. These fit with the arteries branching from the aorta. They make sure blood keeps flowing to important organs like the kidneys, small bowel, and liver.
At places like Liv Hospital, we focus on top-notch vascular care. We put our patients first, making the treatment process as easy as possible.
It’s important to know the risks of aortic aneurysms to get medical help quickly. Aneurysms in the abdomen are a big threat to heart health.
An abdominal aortic aneurysm (AAA) is a swelling of the main blood vessel leading from the heart to the abdomen. It happens when the aorta’s wall weakens and bulges outward.
Many things can raise your risk of getting an AAA. These include being over 65, smoking, high blood pressure, and a family history of aneurysms. Knowing these risks helps find and manage the problem early.
Prevalence: AAAs are more common in men than women. They often come with other vascular diseases.
Not treating an AAA can lead to serious and life-threatening problems. The biggest risk is rupture, which needs emergency surgery.
The risk of rupture grows with the aneurysm’s size. This shows why quick diagnosis and treatment are key.
Historically, treating aortic aneurysms mainly used open surgery. But now, endovascular techniques have changed this. These new methods have greatly improved how we treat aortic aneurysms, making it safer for patients.
Open surgery was once the main way to fix aortic aneurysms. It involved a big cut in the belly to reach the aorta. Then, a vascular graft replaced the bad part. But, it was risky, with high chances of serious problems.
This led to looking for safer ways. The start of endovascular aneurysm repair (EVAR) was a big step forward.
EVAR surgery changed the game with its less invasive approach. It uses small cuts in the groin to put in a stent graft. This method cuts down on recovery time and risks compared to open surgery.
Another big step is fenestrated endovascular aneurysm repair (FEVAR). It keeps blood flowing to important organs. “Fenestrated” means the stent graft has special holes for arteries like the renal or visceral arteries.
Today, we have many ways to treat aortic aneurysms, depending on the patient. TEVAR surgery, or thoracic endovascular aortic repair, is used for thoracic aorta aneurysms. It’s another minimally invasive option.
| Treatment Option | Description | Indications |
| Open Surgical Repair | Traditional method involving a large incision and graft replacement | Suitable for younger patients or those with complex anatomy not amenable to EVAR |
| EVAR Surgery | Minimally invasive endovascular stent graft placement | Ideal for patients with infrarenal aneurysms and suitable anatomy |
| FEVAR | Fenestrated EVAR for complex aneurysms with fenestrations to preserve vital organ perfusion | Used for juxtarenal and pararenal aneurysms |
| TEVAR Surgery | Thoracic EVAR for aneurysms in the thoracic aorta | Indicated for thoracic aortic aneurysms |
The way we treat aortic aneurysms has changed a lot. Now, we choose treatments based on what each patient needs. As technology gets better, we’ll find even better ways to treat aortic aneurysms.
The Fenestrated Endovascular Aneurysm Repair (FEVAR) is a new way to treat tough aortic aneurysms. It’s a less invasive method that has changed how we treat complex aortic problems. It gives hope to those who can’t have traditional surgery.
FEVAR is for aortic aneurysms that can’t be treated with standard EVAR. It uses a special stent graft with fenestrations. These openings match the patient’s arteries, keeping blood flowing to important organs.
The main goal of FEVAR is to block the aneurysm from blood flow. But it keeps blood flowing to vital areas. This is done with detailed imaging and custom stent grafts.
Doctors suggest FEVAR for patients with:
In these cases, FEVAR is a less invasive option. It may cut down on recovery time and lower the risk of complications.
FEVAR’s success depends on the advanced tech of fenestrated stent grafts. These grafts are made to fit the patient’s arteries perfectly, thanks to detailed scans.
The fenestrations are designed to keep blood flowing to key organs. This makes FEVAR different from standard EVAR.
Key benefits of fenestrated stent grafts include:
The FEVAR procedure has changed how we treat complex aortic aneurysms. It offers a less invasive way to tackle these tough cases. FEVAR is made for complex aneurysms, giving them a precise treatment.
Juxtarenal and pararenal aneurysms are hard to treat because they’re close to important blood vessels. The FEVAR procedure uses custom-made stent grafts with special holes. These holes help keep blood flowing to vital organs.
This method helps patients who can’t have traditional surgery. It keeps blood flowing to important arteries. This lowers the chance of problems and improves how patients do.
Fenestrations are key in the FEVAR procedure. They let us place stent grafts just right to keep blood flowing. These special holes are planned carefully to make sure the graft fits perfectly.
Using fenestrations in FEVAR works well to keep blood flowing to important arteries. This reduces the risk of problems like organ damage during aneurysm treatment.
One big plus of FEVAR is using custom-made grafts. These grafts are made just for each patient. They fit better and work more effectively than standard grafts.
With custom grafts, we can make sure the FEVAR procedure works best for each patient. This leads to better results and fewer complications.
FEVAR and standard EVAR surgery are two key ways to treat aortic aneurysms. Each has its own benefits and uses. Knowing the differences helps doctors and patients choose the best treatment.
Standard EVAR is a minimally invasive method for treating abdominal aortic aneurysms (AAAs). It uses a stent graft placed through small groin incisions. The graft is guided by imaging to the aneurysm site. It’s then expanded to fit the aortic walls, excluding the aneurysm from blood flow.
Key components of EVAR include:
Standard EVAR works for patients with aneurysms that have a good “neck” below the renal arteries. But, those with complex aneurysms near or involving the renal arteries might not qualify for standard EVAR. This is because it could harm blood flow to the kidneys.
FEVAR is for these complex cases. It uses custom-made fenestrated stent grafts. These grafts have holes that match the renal and sometimes superior mesenteric arteries. This preserves blood flow to these vital areas.
Both EVAR and FEVAR have high success rates in treating aortic aneurysms. The complexity of the aneurysm and patient selection are key in choosing the right technique.
| Procedure | Success Rate | Complication Rate |
| EVAR | 90-95% | 5-10% |
| FEVAR | 85-90% | 10-15% |
EVAR generally has a higher success rate and lower complication rate than FEVAR. This is mainly because FEVAR treats more complex cases. FEVAR allows treatment of patients not suitable for standard EVAR, expanding treatment options.
In conclusion, both EVAR and FEVAR are important in treating aortic aneurysms. The choice depends on the aneurysm’s anatomy, patient health, and other factors. Understanding these differences is key for the best patient outcomes.
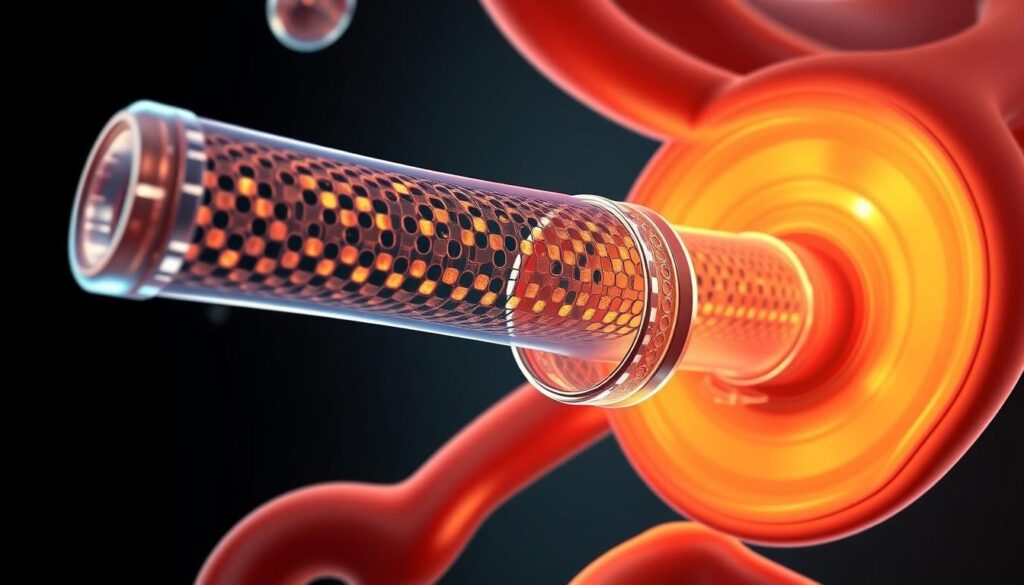
Aortic stents play a key role in fixing damaged blood vessels. They help stop aneurysms from getting worse. These stents are made to support weak aortic walls, lowering the chance of rupture.
The technology behind these stents has grown a lot. Now, patients have a less invasive way to deal with complex aortic aneurysms.
Aortic stents are placed inside the aorta to strengthen weak spots. They act like a scaffold, keeping the aortic wall from expanding or rupturing. This is vital for patients with complex aneurysms, where surgery is too risky.
To place a stent, a small incision is made in the groin. Imaging technology guides it to the right spot in the aorta. Once there, the stent expands to fit the aortic walls, sealing off the aneurysm.
The materials used for aortic stents are very important. Most are made from strong materials like nitinol or stainless steel, sometimes with a fabric graft. The choice depends on the patient’s needs and the aneurysm’s location.
Designs vary, including the stent’s size and how many fenestrations it has. Fenestrated stents are made to fit around vital arteries, keeping them open after the stent is placed.
Modern aortic stents last longer and are more durable. Advances in materials and design have made them better fit for each patient’s body.
| Feature | Description | Benefit |
| Material | Nitinol or Stainless Steel with Fabric Graft | Durability and Biocompatibility |
| Customization | Fenestrations for Visceral Arteries | Preserves Blood Flow to Vital Organs |
| Delivery System | Low Profile for Minimally Invasive Procedure | Reduced Risk and Faster Recovery |
There’s been a big drop in problems with stent grafts, like endoleaks and migration. Regular check-ups and scans are key to seeing how well the stent and aneurysm are doing.
The FEVAR procedure needs careful planning and the right patient selection for the best results. We know that this complex procedure requires a detailed approach to check and prepare patients.
When choosing patients for FEVAR, we look closely at their aortic anatomy. We check the size and location of the aneurysm, if there are branch vessels, and the overall vascular anatomy. These factors are very important.
Accurate anatomical assessment is key to designing the right stent graft and planning the procedure. We use CT scans and other imaging to create a detailed model of the patient’s aortic anatomy.
Advanced imaging is vital for planning FEVAR. We use high-resolution CT scans and 3D modeling to understand the patient’s anatomy well. This helps us design a customized stent graft that fits the patient’s needs.
3D modeling lets us see the aortic anatomy and plan the procedure more precisely. This technology helps us simulate the stent graft deployment and prepare for any challenges during the procedure.
Assessing risks is a big part of preoperative planning for FEVAR. We check the patient’s health, including any conditions that might affect the procedure or recovery. This helps us find and plan for any risks.
Preparing patients involves a team effort, including cardiovascular checks, anesthesia consultations, and other tests. We make sure patients are ready for the procedure and know what to expect during recovery.
By carefully selecting patients, using advanced imaging, and doing thorough risk assessments, we can improve outcomes for FEVAR patients.
The FEVAR procedure is a specialized treatment for complex aortic aneurysms. It’s a minimally invasive surgery designed for juxtarenal and pararenal aneurysms. This approach offers a tailored solution for their repair.
Success in the FEVAR procedure starts with detailed preoperative preparation. We assess the patient’s health and use advanced imaging to understand the aneurysm’s anatomy. Techniques like 3D modeling and CT angiography help us plan the procedure accurately.
By planning carefully, we aim to reduce risks and improve outcomes for our patients.
The FEVAR procedure is a complex, multi-step process. We start by accessing the femoral arteries in the groin. Then, we introduce the fenestrated stent graft under fluoroscopic guidance.
The fenestrations are carefully aligned with the renal and visceral arteries. This allows us to treat aneurysms near or involving the renal arteries, a challenge with traditional EVAR.
After the FEVAR procedure, patients are monitored in a specialized unit. We manage any complications and ensure their comfort and safety. Immediate care includes:
We provide thorough care throughout the FEVAR process. Our goal is to achieve the best outcomes, reduce recovery time, and improve long-term health.
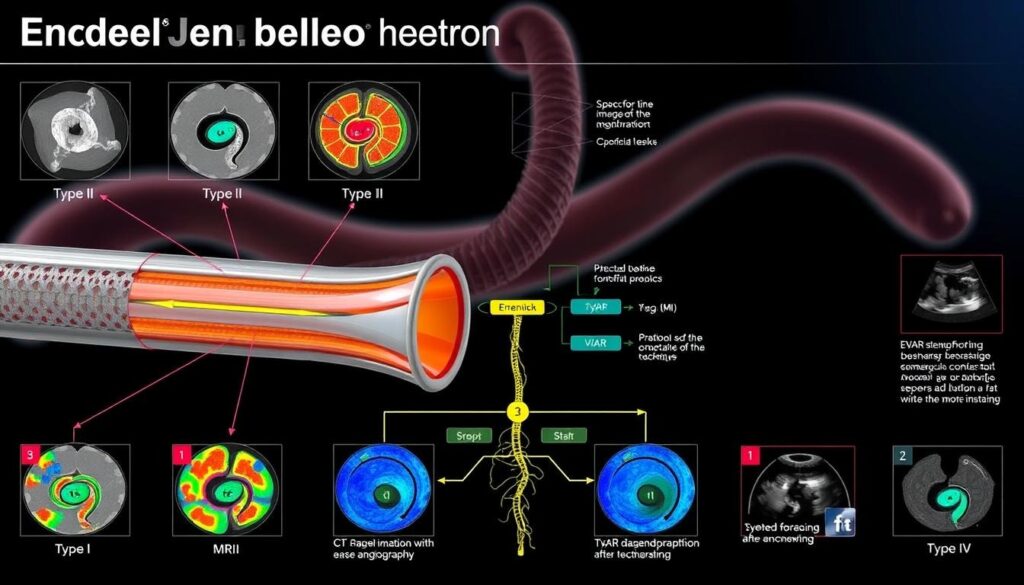
Endoleaks are a possible issue after endovascular aneurysm repair. They need a careful approach for detection and treatment. It’s key to know what they are, how they’re classified, and how to find and treat them.
An endoleak is when blood keeps flowing into the aneurysm sac after a graft is put in. There are five types, each with its own signs and what they mean for treatment.
Finding endoleaks uses different imaging methods. The main one is contrast-enhanced CT scans, which show the graft and nearby areas well. Other methods include ultrasound and angiography.
| Detection Method | Advantages | Limitations |
| Contrast-enhanced CT | High sensitivity and specificity | Contrast use, radiation exposure |
| Ultrasound | Non-invasive, no radiation | Operator-dependent, limited detail |
| Angiography | Detailed vascular imaging | Invasive, possible complications |
Treatment for endoleaks depends on the type and cause. Type I and III endoleaks often need quick action, like more endovascular procedures. Type II endoleaks might be watched or treated with embolization. Type IV is usually managed without surgery, and Type V needs close monitoring.
It’s vital to understand and manage endoleaks well for the best results after EVAR and FEVAR. A detailed approach to finding and treating them helps reduce risks.
The FEVAR technique is a minimally invasive method for treating aortic aneurysms. It greatly reduces recovery time for patients. We will look at the typical recovery time, the need for follow-up imaging, and FEVAR’s success rates.
Patients usually recover from FEVAR in a few weeks. This method causes less tissue trauma and less pain than open surgery. Most can go back to their usual activities in 4 to 6 weeks.
Regular check-ups and imaging are key to tracking FEVAR’s success. We suggest a follow-up plan that includes:
These steps help us make sure the aneurysm is being properly treated. They also catch any signs of endoleaks or graft movement early.
Research shows FEVAR has high long-term success rates. It greatly lowers the risk of aneurysm rupture. Patients often see an improvement in their quality of life, returning to their pre-aneurysm activities.
The long-term success of FEVAR comes from better stent graft technology and careful patient selection and follow-up.
FEVAR and TEVAR are two advanced endovascular methods for treating aortic aneurysms. Each has its own use. Knowing their differences and similarities helps us see how they treat aortic problems.
TEVAR surgery is a less invasive method for thoracic aortic aneurysms. It uses a stent graft in the thoracic aorta. This stops the aneurysm from growing and reduces the risk of rupture.
Key aspects of TEVAR include:
Choosing between FEVAR and TEVAR depends on the aneurysm’s location and the patient’s anatomy. FEVAR is for complex abdominal aortic aneurysms near the renal arteries. TEVAR is for thoracic aortic aneurysms.
| Procedure | Aneurysm Location | Key Considerations |
| FEVAR | Abdominal aorta, involving renal arteries | Complex anatomy, need for fenestrations |
| TEVAR | Thoracic aorta | Thoracic aortic pathology, precise stent graft placement |
Both FEVAR and TEVAR use stent grafts. But, they differ because they treat different parts of the aorta.
“The technical nuances between FEVAR and TEVAR highlight the need for specialized training and expertise in endovascular aortic repair.”
Understanding these differences is key to improving patient care in endovascular surgery.
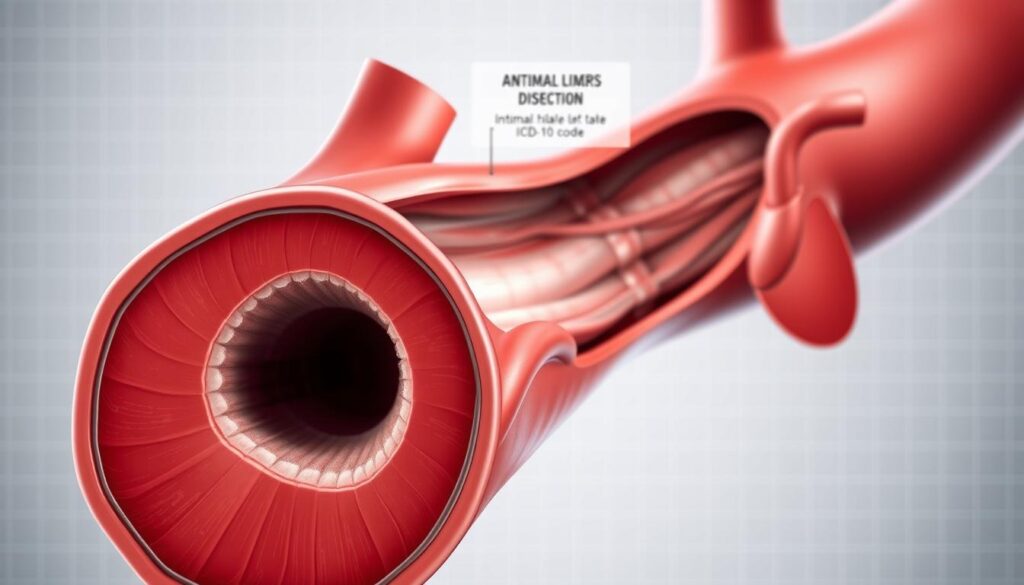
Medical coding is key in classifying aortic procedures. It’s vital for both clinical and administrative needs. This includes insurance claims and patient records.
Aortic dissection is a serious issue needing precise coding. The ICD-10 system has specific codes for different dissections. For example, I71.00 is for a dissection of the aorta, unspecified.
It’s important to know the details of these codes for accurate records. This helps in patient care and research on aortic dissections.
Infrarenal abdominal aortic aneurysms (AAA) need accurate ICD-10 coding. The code I71.4 is for abdominal aortic aneurysm without rupture. It’s key to tell the difference between ruptured and non-ruptured aneurysms.
Correct coding helps in managing AAA patients. It’s also important for studies and planning in healthcare.
Proper medical coding is vital for insurance claims. Wrong or unclear coding can cause denied claims or delayed payments. So, it’s important to keep up with ICD-10 codes and guidelines.
Healthcare providers should document aortic procedures well. This includes details of the condition, treatment, and follow-up care. It supports accurate coding and improves patient care and communication.
Looking ahead, the FEVAR procedure and endovascular aortic repair are set to change how we treat complex aortic aneurysms. New technologies and techniques will lead to better patient outcomes. They will also make minimally invasive treatments more common.
New advancements in fenestrated stent grafts and endovascular systems will make these procedures more precise and effective. Ongoing research and clinical trials will help prove the safety and success of FEVAR. This could make it useful for more patients.
Advanced imaging and personalized graft design will be key in the future of endovascular aortic repair. These innovations will lead to better long-term results and a higher quality of life for patients. They will make a big difference in how we treat aortic aneurysms.
By adopting these new trends and technologies, healthcare providers can offer more personalized and effective treatments. This will move vascular surgery forward and improve care for patients all over the world.
The FEVAR (Fenestrated Endovascular Aneurysm Repair) is a new way to treat big aortic aneurysms. It uses special stent grafts with holes to keep blood flowing to important organs.
FEVAR is a more advanced version of EVAR surgery. It’s for complex aneurysms near or involving the renal arteries. FEVAR uses custom-made grafts with holes for the arteries.
FEVAR is less invasive, leading to quicker recovery and fewer complications. It’s also good for complex aneurysms that EVAR or open surgery can’t handle.
An endoleak is when blood leaks into the aneurysm sac around the stent. It’s a complication of EVAR or FEVAR. Doctors manage it with more treatments, like embolization or stenting.
Choosing the right patient for FEVAR involves detailed checks and 3D models. This ensures the procedure is right for the patient and plans it well.
After FEVAR, most patients get back to normal in a few weeks. Long-term, the success rate is high, with few complications.
FEVAR treats abdominal aortic aneurysms, while TEVAR tackles thoracic ones. Both use stent grafts but differ in approach and design.
Aortic procedures like FEVAR and TEVAR get specific ICD-10 codes. Accurate coding is key for insurance and medical records.
Untreated aortic aneurysms can cause serious issues like rupture. Other risks include organ failure, embolism, and dissection.
Fenestrations in FEVAR grafts keep blood flowing to vital organs. They align with arteries, making it possible to treat complex aneurysms.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us