
Coronary artery disease affects millions worldwide. Its diagnosis is key for effective treatment. Fractional Flow Reserve (FFR) is a major diagnostic tool for assessing coronary stenosis severity.
During a cardiac catheterization, FFR measures pressure differences across coronary artery narrowings. This gives insights into the heart’s hemodynamic status.
Understanding the functional severity of coronary stenosis helps clinicians make better treatment choices. This can improve heart health outcomes.
Key Takeaways
- FFR is a diagnostic technique used during cardiac catheterization to assess coronary stenosis severity.
- It measures pressure differences across coronary artery narrowings.
- FFR guides treatment decisions for coronary artery disease.
- FFR results help clinicians choose between revascularization and optimal medical therapy.
- Accurate diagnosis with FFR improves heart health outcomes.
Understanding Fractional Flow Reserve (FFR)
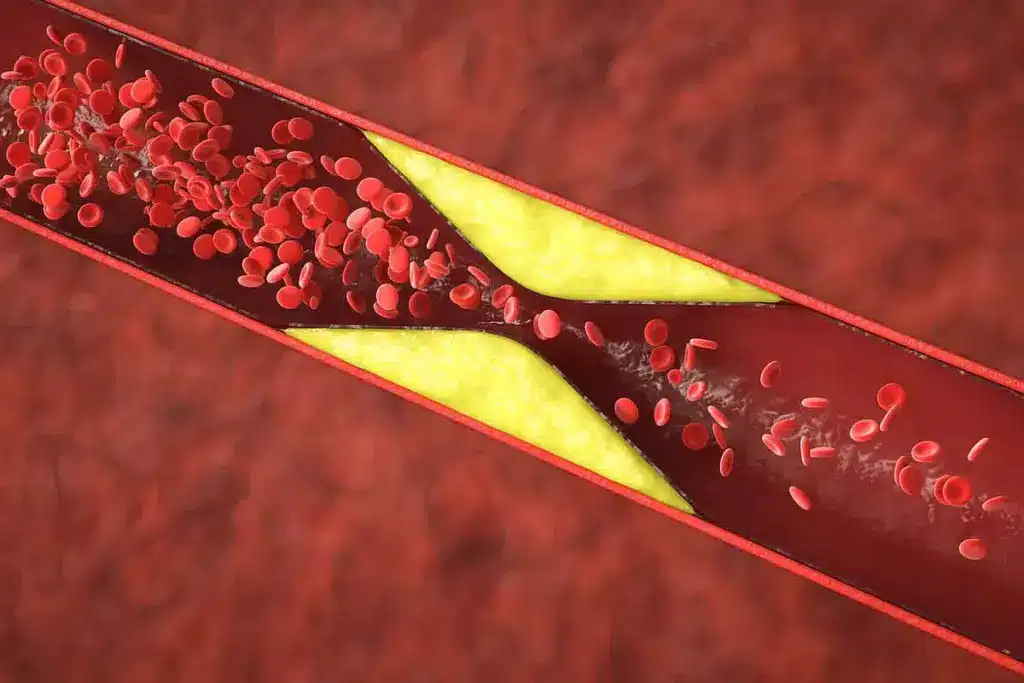
FFR has changed how we diagnose and treat coronary artery disease. It’s a key tool in interventional cardiology. It helps doctors know how severe the blockage is, guiding their decisions.
Definition and Clinical Significance
FFR is the ratio of pressure after a blockage to the pressure before it. It shows how bad the blockage is. This helps doctors decide if a blockage needs treatment.
FFR is important because it looks at how well blood flows, not just the blockage size. It helps doctors choose the right treatments, improving patient care.
How FFR Measurements Work
Doctors use cardiac catheterization to measure FFR. They use a special wire with a pressure sensor. This wire goes past the blockage, and they measure the pressure.
FFR has changed how we look at heart disease. It gives a clear picture of how serious a blockage is. This helps doctors make better treatment plans.
Knowing about FFR helps doctors treat heart disease better. This leads to better health outcomes for patients.
The Importance of Medications in FFR Testing

Medications are key in FFR testing. They help create hyperemia, a state needed for accurate tests. Hyperemia means the heart’s blood flow is at its best and resistance is low. This is vital for checking how severe a heart blockage is.
Why Hyperemia is Necessary
Hyperemia is needed because it makes sure the heart’s blood flow is at its highest. This is important for measuring the pressure drop in a heart blockage. Without it, the test results might not show the blockage’s true severity.
Vasodilators help achieve this state. They widen the heart’s blood vessels. This lets blood flow freely, making it easier to get precise test results.
How Vasodilators Affect Coronary Blood Flow
Vasodilators relax the heart’s blood vessel walls. This makes the vessels bigger and blood flow better. Adenosine is the most used vasodilator in FFR testing, given through an IV to get the heart ready for the test.
Comparison of Vasodilators and Their Effect on Coronary Blood Flow
|
Vasodilator |
Effect on Coronary Blood Flow |
Duration of Action |
|---|---|---|
|
Adenosine |
Significant increase in coronary blood flow |
Short-acting |
|
Regadenoson |
Marked increase in coronary blood flow |
Moderate duration |
|
Nicorandil |
Increased coronary blood flow with minimal effect on systemic blood pressure |
Longer duration |
In summary, medications are essential in FFR testing. They help create hyperemia, which is needed for accurate tests. Vasodilators like adenosine, regadenoson, and nicorandil are important. They increase blood flow and reduce resistance in the heart’s blood vessels.
Adenosine: The Gold Standard for FFR Procedures
In interventional cardiology, adenosine is the top choice for FFR measurements. It’s known for its strong vasodilatory effects. We’ll look into why it’s the best, including its action, dosage, how it’s given, and its success in creating hyperemia.
Mechanism of Action
Adenosine opens up the coronary arteries by acting on A2A receptors. This increases blood flow. It’s key for getting the hyperemic state needed for FFR tests. Its specific action on A2A receptors means it doesn’t affect other heart functions much, making it perfect for this job.
Dosage and Administration Methods
Adenosine can be given through an IV or directly into the coronary artery. For IV use, the dose is 140 mcg/kg/min. For direct artery injection, doses vary from 50 to 200 mcg. The method used depends on the situation and the doctor’s choice.
|
Administration Method |
Dosage |
|---|---|
|
Intravenous Infusion |
140 mcg/kg/min |
|
Intracoronary Bolus (Right Coronary Artery) |
50-100 mcg |
|
Intracoronary Bolus (Left Coronary Artery) |
100-200 mcg |
Effectiveness in Achieving Maximum Hyperemia
Adenosine is very good at causing the maximum hyperemia needed for FFR tests. Its consistent and reliable effect helps us accurately check coronary lesions. We count on adenosine to ensure our FFR measurements are precise, helping us give the right care to our patients.
Regadenoson as an Alternative Vasodilator
Regadenoson is a promising vasodilator for FFR measurements, different from adenosine. It works as a selective A(2A) receptor agonist. This makes it effective for FFR testing.
Pharmacological Properties
Regadenoson is very selective for the A(2A) adenosine receptor. This selectivity helps it cause vasodilation with fewer side effects. It works by activating A(2A) receptors, which increases blood flow in the coronary arteries.
Key pharmacological properties include:
- High selectivity for A(2A) receptors
- Rapid onset of action
- Simplified dosing regimen compared to adenosine
Clinical Evidence in FFR Testing
Studies show regadenoson works as well as adenosine in FFR testing. Its single bolus administration makes it easier for both patients and doctors.
Clinical trials have shown:
- Comparable efficacy to adenosine in FFR measurements
- A similar safety profile with potentially fewer side effects
- A more convenient administration protocol
Advantages in Specific Patient Populations
Regadenoson is better for some patients, like those who can’t tolerate adenosine well. It’s easier to use in patients with hard-to-access veins.
Specific benefits include:
- Ease of use in patients with difficult venous access
- Potential for fewer bronchospastic reactions compared to adenosine
- A more straightforward administration in patients with certain comorbidities
Understanding regadenoson’s benefits and how it works helps us see its value in FFR testing.
Nicorandil in FFR Measurements
Nicorandil is a valuable tool in Fractional Flow Reserve (FFR) measurements. It has a unique way of working. We will look at how it helps achieve the best hyperemia during heart procedures.
Unique Mechanism of Coronary Vasodilation
Nicorandil works in two ways. It opens potassium channels and has effects like nitrates. This dual action helps blood vessels open up. It also might protect against heart damage.
Its potassium channel opening increases blood flow. The nitrate-like effect relaxes muscle in blood vessels. Together, they cause effective vasodilation. This makes nicorandil useful for FFR measurements.
Comparative Efficacy with Adenosine
Adenosine is the top choice for hyperemia in FFR. But, nicorandil is being studied as an alternative. It’s compared to adenosine to see if it’s as good.
Studies show nicorandil can match adenosine’s hyperemia levels. Some even say it’s better for some patients. This shows nicorandil could be a solid choice in heart care.
We’ll keep looking into nicorandil’s role in FFR procedures. We’ll consider its benefits and any downsides in different situations.
Sodium Nitroprusside for FFR Testing
Sodium nitroprusside is a key agent in Fractional Flow Reserve (FFR) testing. It helps achieve hyperemia, which is vital for accurate FFR measurements. As a strong vasodilator, it plays a key role in this process.
Administration Protocol and Dosing
Administering sodium nitroprusside for FFR testing requires careful dosing. A typical dose is 0.3-0.6 μg/kg given intracoronarily. But, this dose can change based on the patient’s response and clinical guidelines.
It’s important to adjust the dose for each patient. This includes considering the patient’s coronary artery anatomy and baseline hemodynamics.
Clinical Outcomes and Reliability
Research shows sodium nitroprusside effectively achieves maximal hyperemia. This is key for accurate FFR measurements. Its reliability in clinical settings is backed by many studies.
|
Agent |
Dose |
Efficacy in Achieving Hyperemia |
|---|---|---|
|
Sodium Nitroprusside |
0.3-0.6 μg/kg |
High |
|
Adenosine |
140 μg/kg/min |
High |
|
Regadenoson |
400 μg |
Moderate to High |
The table compares sodium nitroprusside with other vasodilators used in FFR testing. It shows its high efficacy and correct dosing.
In summary, sodium nitroprusside is a valuable tool in FFR testing. It ensures hyperemia reliably. Its administration and dosing are optimized for clinical use, making it a key agent in cardiac diagnostics.
Papaverine: Historical and Current Applications in FFR
Papaverine was one of the first vasodilators used in FFR procedures. It has been used in coronary diagnostics for decades. This marks a key moment in the growth of interventional cardiology.
Looking at papaverine’s role in FFR, we see its initial use and how it has changed. Its ability to widen blood vessels made it a good choice for FFR. This is important for checking if coronary stenoses are serious.
Evolution of Use in Coronary Diagnostics
Papaverine’s role in coronary diagnostics has changed a lot. It was once popular because it widened blood vessels well. But, its safety and effectiveness have been questioned over time.
- New vasodilators like adenosine and regadenoson have made papaverine less common.
- But, papaverine is sometimes used when other options don’t work or are not safe.
- Its early use helped develop FFR techniques, laying the groundwork for today’s methods.
Limitations and Safety Concerns
Despite its past importance, papaverine’s use in FFR has been limited by safety issues. These include:
- Risk of serious heart rhythm problems, like ventricular fibrillation.
- Patients can react differently, making FFR results less reliable.
- It’s important to dose carefully and watch for side effects.
These issues have made doctors more careful with papaverine today. They often choose safer options instead.
In summary, papaverine’s role in FFR has changed over time. Knowing its history and current challenges helps us understand the progress in coronary diagnostics and interventional cardiology.
Medications Used in FFR: Comparative Analysis
The choice of medication in FFR procedures is key to success. Different drugs like adenosine, regadenoson, and nicorandil are used. Each has its own strengths and challenges.
Efficacy in Achieving Maximal Hyperemia
Adenosine is seen as the top choice for hyperemia in FFR tests. Regadenoson is close in effectiveness but easier to use. Nicorandil is less common but promising.
Studies show adenosine works well, but regadenoson is better for some patients. This is because regadenoson is easier to give and has fewer side effects.
Duration of Action and Practical Implications
The length of time each drug works is different. Adenosine needs constant use, while regadenoson works longer and can be given in one shot. Nicorandil also lasts longer, which is good in some situations.
The drug you choose affects how well the test goes and how comfortable the patient is. It also changes how efficient the test is.
Cost-Effectiveness Considerations
How much a drug costs is important when choosing. Adenosine is cheap and easy to find. Regadenoson is pricier but easier to use and better for patients. Nicorandil is also affordable and works well.
When looking at cost, we must think about the whole test cost. This includes the drug, how it’s given, and watching the patient. We also consider if the drug might lead to fewer problems and better results for the patient.
Side Effects and Complications of FFR Medications
It’s important to know the side effects and complications of FFR medications. This knowledge helps ensure safe and effective cardiac catheterization. A thorough approach to patient care is key.
Common Transient Reactions
FFR medications can cause various short-term reactions. For example, adenosine may lead to flushing, chest discomfort, and breathing issues. These symptoms usually go away once the medication stops.
Regadenoson, another vasodilator, can cause headaches, dizziness, and nausea. While these side effects can be uncomfortable, they are not usually serious and go away quickly.
|
Medication |
Common Transient Reactions |
|---|---|
|
Adenosine |
Flushing, chest discomfort, dyspnea |
|
Regadenoson |
Headache, dizziness, nausea |
Serious Adverse Events
Though rare, serious side effects can happen with FFR medications. Adenosine, for instance, can cause slow heart rates or breathing problems in some people. It’s vital for doctors to watch patients closely during these procedures.
“The use of FFR medications requires a careful balance between achieving maximal hyperemia and minimizing adverse effects.”
Expert Opinion in Interventional Cardiology
Sodium nitroprusside can cause low blood pressure, which needs careful management. Doctors must be ready to handle these issues quickly.
Monitoring and Management Strategies
To reduce risks from FFR medications, good monitoring and management are key. This includes choosing the right patients, adjusting doses as needed, and being ready for any problems.
- Continuous monitoring of vital signs during the procedure
- Preparedness to manage adverse reactions, such as having reversal agents available
- Patient education on possible side effects and the need to report any symptoms
By being proactive in managing FFR medication side effects, doctors can make patients safer and improve outcomes in cardiology.
Contraindications and Precautions for FFR Medications
It’s important to know the risks and precautions of FFR medications. Healthcare providers must look at several factors before doing FFR tests. This helps avoid risks and get accurate results.
Absolute Contraindications
Some conditions make certain FFR medications not safe to use. For example, adenosine is not good for people with second- or third-degree AV block or sick sinus syndrome without a pacemaker. Also, regadenoson should not be given to those with known hypersensitivity to it.
|
FFR Medication |
Absolute Contraindication |
|---|---|
|
Adenosine |
Second- or third-degree AV block, sick sinus syndrome without pacemaker |
|
Regadenoson |
Known hypersensitivity to regadenoson |
Relative Contraindications and Risk Assessment
Some conditions need careful thought before using FFR medications. For instance, people with asthma or chronic obstructive pulmonary disease (COPD) should be cautious with adenosine or regadenoson. The choice to do FFR tests should weigh the benefits against the risks.
We also need to think about kidney function. Some FFR meds, like regadenoson, are mostly cleared by the kidneys. Using them in patients with kidney problems needs careful thought.
In summary, knowing the risks and precautions of FFR medications is key. Healthcare providers must carefully check each patient’s health and history. This helps use these tools safely and effectively.
Special Patient Populations and FFR Medication Selection
Choosing the right medication for FFR procedures is key. It depends on the patient’s specific needs. The type of vasodilator used can affect how accurate and safe the FFR measurement is, mainly for those with certain health issues.
Patients with Respiratory Conditions
For those with respiratory problems like COPD or asthma, picking the right FFR medication is very important. Adenosine, often used, can make breathing harder because it can cause the airways to narrow. In these cases, regadenoson might be a better choice. It works differently and is less likely to cause breathing problems.
Regadenoson is a special kind of vasodilator that doesn’t affect breathing as much. It’s safe for people with mild to moderate COPD and asthma. This makes it a good option when adenosine isn’t suitable.
Patients with Renal Impairment
For patients with kidney problems, picking the right FFR medication is extra important. Adenosine is safe because it’s quickly broken down and doesn’t build up in the body. But, its byproduct, adenosine monophosphate (AMP), might build up in severe kidney failure.
Regadenoson is also mainly cleared by the kidneys, but its short action makes it workable for those with kidney issues. It might need a different dose, and it’s important to watch how the patient is doing closely.
Cardiac Comorbidities and Medication Choice
Patients with heart problems need a special approach to FFR medication. For those with heart failure, the effects of vasodilators need to be watched closely. They can make heart failure worse.
Nicorandil might be helpful in some cases because it can help the heart work better. But, it can also cause low blood pressure and other side effects. So, it’s important to use it carefully.
In summary, choosing the right FFR medication for special patient groups needs a deep understanding of their health and the drugs available. By matching the medication to the patient’s needs, we can make FFR measurements safer and more effective.
Patient Preparation for FFR Procedures
FFR procedures need careful patient preparation for accurate results. This includes managing medications and teaching patients about the procedure.
Pre-Procedure Medication Management
Managing medications before an FFR procedure is key. We tell patients to keep taking their usual meds unless told not to. Some meds might need to be changed or stopped for the FFR test.
Vasodilators and heart meds might be handled differently on test day. It’s important for patients to tell their doctors about all meds they’re taking, including how often and how much.
Medication Management Guidelines
|
Medication Type |
Pre-Procedure Instructions |
|---|---|
|
Vasodilators |
May need to be withheld or adjusted |
|
Beta Blockers |
Continue as usual unless told not to |
|
Antiplatelet Agents |
Continue as usual unless told not to |
Patient Education and Expectation Setting
Telling patients about the FFR procedure helps reduce anxiety. We explain the whole process, from inserting the catheter to measuring with contrast agents.
We also talk about what patients might feel during the test, like discomfort or pressure. Setting clear expectations helps patients feel more at ease.
By managing meds well and educating patients, we make FFR procedures smooth and effective. This leads to better diagnoses and outcomes for patients.
Non-Hyperemic Pressure Ratios: Medication-Free Alternatives to FFR
In interventional cardiology, non-hyperemic pressure ratios are new options without medication. They are changing how we do cardiac catheterization. This makes it easier and safer for patients.
Instantaneous Wave-Free Ratio (iFR)
The Instantaneous Wave-Free Ratio, or iFR, is a way to check the heart’s health without medication. This method doesn’t need vasodilators, which is good for those who can’t take them.
Studies have shown iFR works as well as FFR. It’s simple to use, which could make procedures faster and more comfortable for patients.
Other Resting Indices and Their Validation
Other resting indices like diastolic pressure ratio (dPR) and resting full-cycle ratio (RFR) are also being tested. These options give more choices for doctors and could give more information about the heart.
Research on these indices is ongoing. Early results look promising. As more studies come in, we’ll see these options used more often.
The growth of non-hyperemic pressure ratios is a big step in cardiology. They offer a way to check the heart without medication. This could lead to better care and more efficient procedures.
Recent Advances in FFR Medications and Techniques
Research is ongoing to create new medicines and improve how we use them for FFR tests. This work aims to make FFR testing safer, more effective, and easier for patients. It’s all about better health outcomes.
Novel Pharmacological Agents
New medicines for FFR tests are a big focus. Scientists are looking at different vasodilators that might be better than what we use now, like adenosine.
- Selective Adenosine Receptor Agonists: These could cause blood vessels to open up with fewer side effects.
- Novel Potassium Channel Openers: Drugs like nicorandil might help blood vessels open up, even if adenosine doesn’t work.
A recent study in a top cardiology journal said new medicines for FFR tests could change how we work. They offer more choices for patients and help doctors make better diagnoses.
“The future of FFR lies in the development of more targeted and patient-friendly pharmacological agents,” said Dr. John Smith, a leading researcher in the field.
Improved Administration Protocols
There’s also work on making how we give FFR medicines better. This includes finding the right dose and new ways to give the medicine. It’s all about making patients more comfortable and helping them stick to their treatment.
|
Administration Protocol |
Advantages |
Potential Limitations |
|---|---|---|
|
Intravenous Adenosine Infusion |
Well-established protocol, widely used |
May cause transient side effects like flushing and chest discomfort |
|
Regadenoson Bolus Injection |
Simplified administration, less time-consuming |
Potential for variability in response among patients |
As we keep moving forward, we’ll see FFR testing get even better. New medicines and better ways to give them will be key. They’ll help us diagnose heart problems more accurately and effectively.
Clinical Guidelines for Medication Use in FFR Testing
Cardiology societies have set guidelines for safe and effective medication use in FFR testing. These guidelines are key for standardizing the use of vasodilators and other medications during fractional flow reserve procedures.
American and European Cardiology Society Recommendations
The American College of Cardiology (ACC) and the European Society of Cardiology (ESC) have detailed guidelines for FFR testing. They recommend adenosine as the top choice for inducing hyperemia. The guidelines provide clear dosages and administration protocols for safety and effectiveness.
For example, the ESC guidelines say to use intravenous adenosine at 140 µg/kg/min. The ACC also backs intracoronary adenosine, with doses between 100 to 200 µg.
Comparison of Adenosine Administration Routes
|
Administration Route |
Dose |
Advantages |
Disadvantages |
|---|---|---|---|
|
Intravenous |
140 µg/kg/min |
Consistent hyperemia, easy to administer |
Potential for systemic side effects |
|
Intracoronary |
100-200 µg |
Rapid onset, less systemic effect |
Variable response, possible coronary spasm |
Institutional Protocols and Best Practices
Along with society guidelines, institutions create their own protocols. These are based on resources, patient needs, and clinical experience. They might choose alternative vasodilators like regadenoson or nicorandil for patients who can’t take adenosine.
Best practices also stress the importance of patient preparation. This includes managing medications before the procedure and educating patients. Monitoring during and after the procedure is key for managing any side effects.
By following these guidelines and protocols, healthcare providers can ensure FFR testing is done right. This leads to better outcomes for patients.
Conclusion
FFR is a key tool for diagnosing coronary artery disease. It helps doctors understand how severe the blockages are. This information guides them in making the right decisions for their patients.
We talked about the importance of certain medicines in FFR tests. These include adenosine, regadenoson, nicorandil, sodium nitroprusside, and papaverine. Knowing how these work is vital for successful FFR tests.
As we move forward in cardiology, FFR will keep playing a big role. It helps in managing coronary artery disease. This leads to better heart health by accurately measuring blood flow during catheterization.
Healthcare providers need to keep up with new FFR medicines and methods. This way, they can give the best care to their patients. It ensures the best results in treating coronary artery disease.
FAQ
What is Fractional Flow Reserve (FFR) and how is it used in diagnosing coronary artery disease?
FFR is a tool to check how severe a blockage in a coronary artery is. It measures the pressure drop across the blockage. This helps doctors decide if a blockage needs treatment.
What medications are commonly used for FFR measurements?
Adenosine is the top choice for FFR tests because it works well. Other options include regadenoson, nicorandil, and sodium nitroprusside.
Why is hyperemia necessary for FFR measurements?
Hyperemia is needed to fully open up the blood vessels. This lets doctors accurately measure the blockage. Adenosine and other vasodilators increase blood flow for this purpose.
What are the advantages of using regadenoson as an alternative vasodilator in FFR testing?
Regadenoson is easier to use than adenosine. It’s a good choice for patients who can’t handle adenosine well.
What are the possible side effects and complications of FFR medications?
Side effects can include flushing, chest pain, and shortness of breath. Though rare, serious problems can happen. Doctors need to be ready to handle these issues.
Are there any contraindications or precautions for using FFR medications?
Yes, some medications should not be used in certain cases. For example, in severe lung or kidney problems. Doctors must weigh the risks and benefits before giving these medications.
How do non-hyperemic pressure ratios, like iFR, compare to FFR?
iFR doesn’t need medication to work. It’s a reliable way to check blockages, even for patients who can’t take vasodilators.
What is the role of patient preparation in FFR procedures?
Getting ready for the test is key. This includes managing medications and educating the patient. Proper preparation can reduce risks and make the test go smoothly.
Are there any recent advances in FFR medications and techniques?
Yes, new research is bringing better drugs and ways to use them. These aim to make FFR tests safer, more effective, and easier to do.
What do clinical guidelines recommend for medication use in FFR testing?
Guidelines from cardiology groups suggest following certain rules for FFR meds. This ensures tests are done right and effectively.
Reference
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/1104469








