Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know that cardiomyopathy is a complex heart condition. It makes it hard for the heart to pump blood well. This disease affects the heart’s muscle, leading to different outcomes.
Discover the 5 main forms of cardiomyopathy, their symptoms, and how doctors diagnose each type.
We believe it’s important to understand the different types of cardiomyopathy. This knowledge helps in early detection and treatment. Cardiomyopathy is a big cause of heart problems and death around the world.
Our team focuses on our patients, using the latest medical knowledge. We aim to give reliable care for all cardiomyopathy types. By explaining cardiomyopathy and its types, we want to help our patients understand their condition and treatment options.
Key Takeaways
- Cardiomyopathy is a serious heart condition that affects the myocardium.
- There are several types of cardiomyopathy, each with different characteristics.
- Understanding the various types is key for effective diagnosis and treatment.
- Liv Hospital offers patient-centered care and advanced treatment options for cardiomyopathy.
- Early detection and management are vital for better outcomes in cardiomyopathy patients.
Understanding Cardiomyopathy and Its Impact

Cardiomyopathy is a complex heart muscle condition. It comes in many forms, each with its own traits. This condition can be passed down or develop over time, affecting people of all ages. The severity and symptoms of cardiomyopathy vary greatly among its types.
Definition and General Characteristics
Cardiomyopathy makes the heart muscle grow too big, get too thick, or become stiff. This hampers the heart’s ability to pump blood well. The main types are dilated, hypertrophic, restrictive, arrhythmogenic right ventricular cardiomyopathy, and left ventricular non-compaction. Each type has its own way of affecting the heart.
People with cardiomyopathy often have an enlarged or stiff heart. This can cause symptoms like shortness of breath, feeling tired, and irregular heartbeats. In severe cases, it can lead to heart failure or arrhythmias, greatly affecting one’s life quality.
Prevalence and Significance in Cardiac Health
Cardiomyopathy is a major cause of illness and death worldwide, affecting millions. The most common types are dilated cardiomyopathy and hypertrophic cardiomyopathy.
Cardiomyopathy is very important in heart health. It’s a top reason for heart failure and sudden death, mainly in the young. Knowing about cardiomyopathy helps in early diagnosis and treatment.
| Type of Cardiomyopathy | Prevalence | Key Characteristics |
| Dilated Cardiomyopathy | Most common form | Enlarged heart, reduced ejection fraction |
| Hypertrophic Cardiomyopathy | Common, often genetic | Thickened heart muscle, possible outflow blockage |
| Restrictive Cardiomyopathy | Rare | Stiff heart walls, poor filling |
| Arrhythmogenic Right Ventricular Cardiomyopathy | Rare, often genetic | Fatty tissue replaces right ventricular muscle, leading to arrhythmias |
| Left Ventricular Non-Compaction Cardiomyopathy | Rare | Deep recesses and prominent trabeculae in the left ventricle |
It’s key for doctors to know about the different cardiomyopathy types. This knowledge helps in diagnosing and treating the condition. Early treatment can greatly improve the lives of those with cardiomyopathy.
The Five Main Forms of Cardiomyopathy

Knowing the different types of cardiomyopathy is key for the right diagnosis and treatment. Cardiomyopathy is a group of heart muscle diseases. They cause various symptoms and outcomes.
Classification Overview
The main types of cardiomyopathy are dilated, hypertrophic, arrhythmogenic right ventricular cardiomyopathy (ARVC), restrictive, and left ventricular non-compaction cardiomyopathy (LVNC). Each type has its own signs and effects on the heart.
We sort these conditions by their look and how they work. For example, dilated cardiomyopathy makes the left ventricle big and weak. On the other hand, hypertrophic cardiomyopathy makes the heart muscle thick, which can block blood flow.
| Type of Cardiomyopathy | Key Characteristics |
| Dilated Cardiomyopathy | Left ventricular dilatation, systolic dysfunction |
| Hypertrophic Cardiomyopathy | Thickening of the heart muscle, possible obstruction |
| Restrictive Cardiomyopathy | Stiff ventricular walls, poor diastolic filling |
| Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) | Right ventricular replacement with fibrofatty tissue |
| Left Ventricular Non-Compaction Cardiomyopathy (LVNC) | Deep recesses and prominent trabeculae |
Diagnostic Approaches
Figuring out the exact type of cardiomyopathy needs a mix of doctor’s checks, imaging, and sometimes genetic tests. Echocardiography is a big help, showing how the heart looks and works.
A leading cardiology journal says, “Diagnosing cardiomyopathy needs a full check-up. This includes family history, ECG, and advanced imaging like MRI” (
Cardiomyopathy Diagnosis: A Complete Approach.
Journal of Cardiology
Epidemiology and Global Distribution
The spread of different cardiomyopathies changes around the world. It’s affected by genes, environment, and population. For example, hypertrophic cardiomyopathy is a big reason for sudden death in young athletes.
It’s important to know how cardiomyopathy spreads to plan for health and resources. We need to look at where these diseases are found to improve diagnosis, treatment, and prevention.
Dilated Cardiomyopathy: The Most Common Form
Dilated cardiomyopathy is the most common heart disease. It affects the heart’s main pumping chamber. This condition makes it hard for the heart to pump blood well.
Pathophysiology and Characteristics
Dilated cardiomyopathy mainly affects the left ventricle. It makes the ventricle enlarge and weaken. This can lead to heart failure.
The disease causes the ventricle to dilate and the ejection fraction to drop. These changes can cause symptoms like fatigue and shortness of breath.
Causes and Risk Factors
Dilated cardiomyopathy can be caused by many things. These include genetic factors, infections, toxins, and metabolic disorders. Genetic predisposition is a big factor, affecting the heart muscle’s structure and function.
Other risk factors include coronary artery disease, hypertension, and diabetes mellitus. Lifestyle factors like drinking too much alcohol and drug abuse also play a role.
Clinical Presentation and Symptoms
Patients with dilated cardiomyopathy often have symptoms of heart failure. These include dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea. As the disease gets worse, symptoms can get worse too.
Common signs include jugular venous distension, peripheral edema, and pulmonary congestion. Early diagnosis and treatment are key to better outcomes.
Treatment Approaches
Treatment for dilated cardiomyopathy aims to manage symptoms and slow disease progression. This includes medications like ACE inhibitors and beta-blockers. These help reduce the heart’s workload.
Lifestyle changes, such as dietary changes and regular exercise, are also recommended. In severe cases, device therapy like ICDs or CRT may be needed. Heart transplantation is an option for those with severe heart failure.
It’s important to understand the differences between dilated cardiomyopathy and other types. Each type has its own characteristics and needs specific treatment.
Hypertrophic Cardiomyopathy: Understanding the Genetic Link
Hypertrophic cardiomyopathy is a leading cause of sudden death in young people. It’s often inherited. This condition makes the heart muscle thick, blocking blood flow and raising the risk of arrhythmias.
Pathophysiology and Characteristics
The heart muscle cells grow too big in hypertrophic cardiomyopathy. This causes the heart walls to thicken. The heart then pumps blood less efficiently, leading to symptoms like chest pain and shortness of breath.
Key characteristics of HCM include:
- Asymmetrical septal hypertrophy
- Left ventricular outflow tract obstruction
- Myocardial disarray
- Potential for arrhythmias
Genetic Factors and Inheritance Patterns
Hypertrophic cardiomyopathy is linked to genetic mutations in the heart’s proteins. It’s often passed down in an autosomal dominant pattern. This means one copy of the mutated gene can cause the condition.
Genetic testing can spot those at risk early. This allows for early monitoring and treatment. Family members of those with HCM should get screened, including echocardiography and genetic tests.
Clinical Presentation and Symptoms
The symptoms of hypertrophic cardiomyopathy vary. Some people may not show symptoms at all. Others might experience:
- Chest pain or discomfort
- Shortness of breath
- Fainting or near-fainting spells
- Palpitations
These symptoms can get worse with dehydration, hard exercise, or certain medicines.
Treatment Strategies and Sudden Death Prevention
Treatment for hypertrophic cardiomyopathy aims to ease symptoms and prevent complications. It also tries to lower the risk of sudden death. Treatment options include:
- Medicines to help symptoms and improve heart function
- Lifestyle changes, like avoiding hard exercise
- Surgery to reduce obstruction
- ICD placement for those at high risk
Early diagnosis and proper treatment are key to preventing sudden death. They also improve life quality for those with HCM.
Restrictive Cardiomyopathy: The Rarest Form
Restrictive cardiomyopathy is the rarest heart condition. It makes the ventricular walls stiff. This stops the heart from filling with blood between beats.
Pathophysiology and Characteristics
Restrictive cardiomyopathy makes the ventricular walls stiff. This stops the heart from expanding and filling properly. It increases the heart’s filling pressures, leading to diastolic dysfunction.
This condition is different from hypertrophic cardiomyopathy. In hypertrophic cardiomyopathy, the walls thicken. But in restrictive cardiomyopathy, the walls stay the same thickness but become rigid. This makes it hard for the ventricles to relax and fill during diastole.
Causes and Associated Conditions
Restrictive cardiomyopathy can be caused by many things. These include diseases like amyloidosis, where proteins build up in the heart. It can also be caused by diseases like hemochromatosis, where iron builds up.
Other causes include radiation therapy to the chest and certain chemotherapy drugs. Some genetic conditions can also cause it. Often, the exact cause is unknown, making diagnosis and treatment hard.
Clinical Presentation and Symptoms
Symptoms of restrictive cardiomyopathy can be similar to other heart conditions. They include shortness of breath, fatigue, and swelling in the legs and abdomen.
As the condition gets worse, symptoms can get more severe. Patients may feel palpitations and chest pain, mostly during exertion.
| Symptom | Description |
| Shortness of Breath | Difficulty breathing, even when resting or doing light activities. |
| Fatigue | Feeling tired or weak, even after resting or doing light activities. |
| Swelling | Fluid buildup causing swelling in the legs, ankles, and abdomen. |
Management Approaches
Managing restrictive cardiomyopathy involves treating the cause and alleviating symptoms. This improves the patient’s quality of life.
Treatment may include medicines to reduce fluid, control heart rate, and manage arrhythmias. In severe cases, heart transplantation may be considered.
Comparing restrictive cardiomyopathy vs hypertrophic cardiomyopathy shows the need for accurate diagnosis. Each condition requires different management approaches.
Arrhythmogenic Right Ventricular Cardiomyopathy
We are going to explore arrhythmogenic right ventricular cardiomyopathy. This condition is when the right ventricle’s walls are replaced with fibro-fatty tissue. It mainly affects the right ventricle and can cause life-threatening arrhythmias.
Pathophysiology and Characteristics
ARVC is a heart condition where the right ventricle’s muscle is replaced with fatty tissue. This leads to abnormal heart rhythms. The condition involves the replacement of the ventricular myocardium with fibro-fatty tissue. This disrupts the heart’s normal electrical activity.
Genetic Basis and Risk Factors
ARVC often runs in families in an autosomal dominant pattern. This means one copy of the mutated gene can cause the condition. The genes involved are those that encode desmosomal proteins. Knowing the genetic basis helps identify those at risk and take preventive steps.
Clinical Presentation and Arrhythmias
The symptoms of ARVC can vary a lot. Some people may not show any symptoms, while others may experience palpitations, syncope, or even sudden cardiac death. The disease is often marked by ventricular tachycardia, which can happen during physical activity.
Treatment and Prevention of Sudden Cardiac Death
Treatment for ARVC aims to prevent sudden cardiac death and manage symptoms. It includes using anti-arrhythmic medications, implantable cardioverter-defibrillators (ICDs), and avoiding strenuous exercise.
| Characteristics | ARVC | Dilated Cardiomyopathy | Hypertrophic Cardiomyopathy |
| Primary Ventricle Affected | Right | Left | Left |
| Pathophysiology | Fibro-fatty replacement | Dilation and systolic dysfunction | Hypertrophy and diastolic dysfunction |
| Common Symptoms | Palpitations, syncope | Heart failure symptoms | Chest pain, dyspnea |
Left Ventricular Non-Compaction Cardiomyopathy
Left ventricular non-compaction cardiomyopathy is a rare heart condition. It affects the left ventricle’s walls. Advances in imaging have helped us recognize it as a distinct condition.
Pathophysiology and Unique Features
This condition happens when the left ventricle doesn’t develop properly. It looks like a sponge because of its structure. This can lead to heart problems and other issues.
It can cause heart failure, arrhythmias, and even blood clots. Finding this condition can be tricky because it looks like other heart problems on scans.
Diagnostic Criteria and Challenges
Diagnosing this condition needs a careful look at the heart and sometimes genetic tests. Doctors look for a specific ratio on heart scans. But, it can be hard to tell it apart from other heart issues.
Using different tests and looking at the heart’s structure helps confirm the diagnosis. Cardiac MRI is very helpful in showing how bad the condition is.
Clinical Presentation and Complications
People with this condition can have different symptoms. Some might not show any symptoms at all. Others might have severe heart problems or arrhythmias.
Complications include heart failure, irregular heartbeats, and blood clots. Early treatment is key to managing these problems.
Management Strategies
Treating this condition involves several steps. Doctors use medicines for heart failure and blood thinners to prevent clots. Sometimes, a device is implanted to prevent sudden death. Regular check-ups are also important.
In summary, left ventricular non-compaction cardiomyopathy is a complex condition. Understanding it helps us give better care to those affected.
Key Comparisons Between Different Forms of Cardiomyopathy
It’s important for doctors to know the differences between various cardiomyopathies. This knowledge helps them create better treatment plans. It can greatly improve how patients do.
Dilated vs. Hypertrophic Cardiomyopathy
Dilated cardiomyopathy (DCM) and hypertrophic cardiomyopathy (HCM) are common types. DCM makes the heart’s chambers big, but it can’t pump blood well. HCM makes the heart muscle thick, blocking blood flow.
DCM often shows symptoms like shortness of breath and tiredness. This is because the heart can’t pump blood well. HCM can cause chest pain, shortness of breath, and fainting. This is because the thickened muscle blocks blood flow and can cause irregular heartbeats.
| Characteristics | Dilated Cardiomyopathy | Hypertrophic Cardiomyopathy |
| Primary Feature | Enlargement of heart chambers | Thickening of heart muscle |
| Symptoms | Heart failure symptoms (e.g., shortness of breath, fatigue) | Chest pain, shortness of breath, fainting spells |
| Treatment Focus | Managing heart failure, improving pumping efficiency | Relieving obstruction, managing arrhythmias |
Restrictive vs. Hypertrophic Cardiomyopathy
Restrictive cardiomyopathy (RCM) and HCM are similar but different. RCM makes the heart walls stiff, making it hard to fill with blood. HCM makes the heart muscle thick, which can also make it hard to fill with blood.
Both can cause problems with filling the heart, but they have different causes and symptoms. HCM often comes from genetics and can cause many symptoms, including blockages and irregular heartbeats. RCM can come from many things, like amyloidosis, and can also cause symptoms related to filling problems.
“The differentiation between restrictive and hypertrophic cardiomyopathy is vital, as their treatment plans are different.”
— Expert in Cardiology
Dilated vs. Restrictive Cardiomyopathy
DCM and RCM are different in how they affect the heart. DCM makes the heart’s chambers big, leading to poor pumping. RCM makes the heart walls stiff, leading to filling problems.
Both can cause symptoms like shortness of breath and tiredness. But, the reasons and heart changes are different.
Distinguishing Features of ARVC and LVNC
Arrhythmogenic right ventricular cardiomyopathy (ARVC) and left ventricular non-compaction cardiomyopathy (LVNC) are less common. ARVC replaces the right ventricle with fat, causing arrhythmias and risk of sudden death. LVNC has deep grooves in the left ventricle, leading to poor pumping and arrhythmias.
Both have genetic links and need careful diagnosis and treatment. Knowing their unique features is key to improving patient care.
Diagnostic Approaches and Clinical Management
Diagnosing and managing cardiomyopathy needs a detailed plan. This plan includes many diagnostic tools and methods. We will look at how to diagnose and manage cardiomyopathy. This includes imaging, lab tests, genetic testing, and choosing the right treatment.
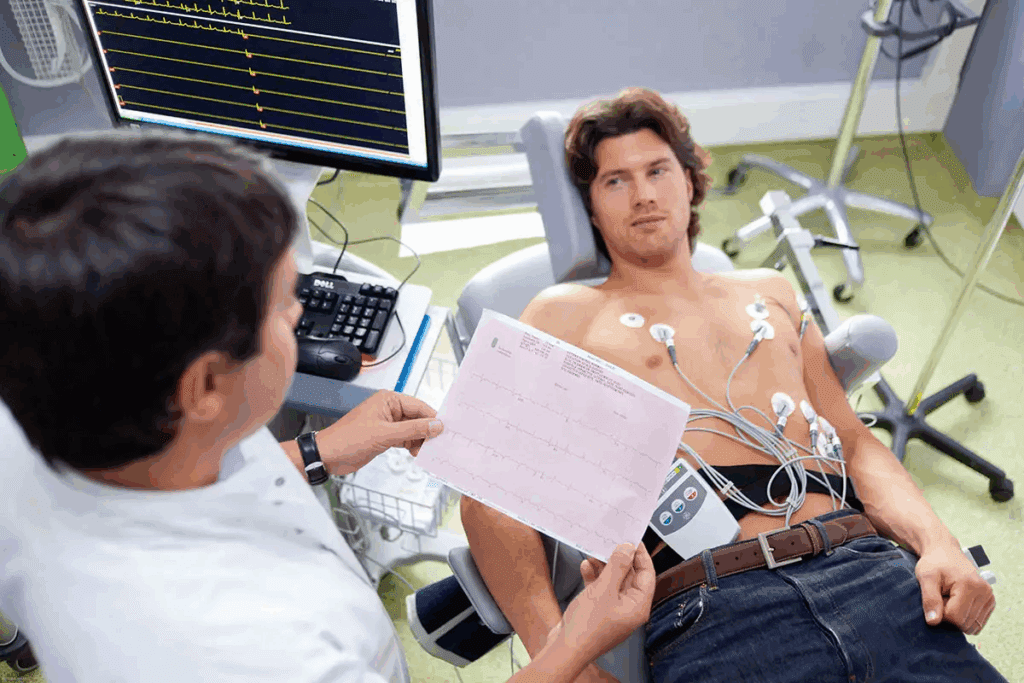
Imaging Techniques and Their Applications
Imaging is key in finding cardiomyopathy. We use echocardiography, cardiac magnetic resonance (CMR) imaging, and cardiac computed tomography (CT) scans. These help us see how the heart looks and works.
- Echocardiography shows the heart’s size, wall thickness, and how well it pumps.
- CMR imaging gives detailed views of the heart’s shape, tissue, and scarring.
- Cardiac CT scans help check for heart disease and look at the heart’s structure.
Laboratory Tests and Biomarkers
Lab tests and biomarkers are vital for diagnosing and managing cardiomyopathy. We use tests to find causes, see how severe the disease is, and check if treatments are working.
Some important lab tests include:
- Blood tests for heart failure signs, like BNP or NT-proBNP.
- Tests for underlying causes, such as thyroid function tests or genetic screening.
- Markers of heart damage, like troponin levels.
Genetic Testing and Family Screening
Genetic testing is key in diagnosing and managing cardiomyopathy, mainly for family forms. We suggest genetic testing for those with a family history of cardiomyopathy. This includes hypertrophic cardiomyopathy (HCM) and arrhythmogenic right ventricular cardiomyopathy (ARVC).
“Genetic testing can help identify individuals at risk of developing cardiomyopathy and facilitate early intervention to prevent complications.”
— American Heart Association
Treatment Selection Based on Cardiomyopathy Type
Treatment for cardiomyopathy depends on the type and how severe it is. We consider symptoms, disease progress, and risk of complications when choosing treatments.
For example:
| Cardiomyopathy Type | Treatment Approach |
| Dilated Cardiomyopathy | Medications for heart failure, ICDs for sudden death prevention. |
| Hypertrophic Cardiomyopathy | Beta-blockers or other medications for symptoms, septal reduction therapy in some cases. |
| Restrictive Cardiomyopathy | Managing underlying causes, like amyloidosis, and treating heart failure symptoms. |
By using a detailed diagnostic approach and tailoring treatment, we can improve patient outcomes and quality of life.
Conclusion: Advances in Understanding and Managing Cardiomyopathies
Improving how we understand and manage cardiomyopathies is key to better patient care. New research and advancements in testing and treatments are helping. These changes are making a big difference in how we handle different types of cardiomyopathy.
The main types of cardiomyopathy include dilated, hypertrophic, restrictive, arrhythmogenic right ventricular, and left ventricular non-compaction. Each type needs its own approach to diagnosis and treatment. As we learn more, we can offer better, more specific treatments.
Investing in research and new ideas is essential. It helps us understand and treat cardiomyopathy better. This progress is important for helping patients all over the world.
Getting cardiomyopathy right means accurate diagnosis and the right treatment. We must keep working to understand and manage all types of cardiomyopathy. This commitment is vital for improving patient care.
FAQ
What is cardiomyopathy?
Cardiomyopathy is a disease that affects the heart muscle. It makes it hard for the heart to pump blood. There are five main types, each with its own characteristics.
What are the five main types of cardiomyopathy?
The five main types are dilated cardiomyopathy, hypertrophic cardiomyopathy, restrictive cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, and left ventricular non-compaction cardiomyopathy.
What is the difference between dilated and hypertrophic cardiomyopathy?
Dilated cardiomyopathy makes the heart big. Hypertrophic cardiomyopathy makes the heart muscle thick. Both affect the heart’s function but in different ways.
How does restrictive cardiomyopathy differ from hypertrophic cardiomyopathy?
Restrictive cardiomyopathy makes the heart stiff. This makes it hard for the heart to fill with blood. Hypertrophic cardiomyopathy makes the heart muscle thick, blocking blood flow.
What are the causes and risk factors for dilated cardiomyopathy?
Dilated cardiomyopathy can be caused by genetic mutations, infections, and toxins. Risk factors include family history and certain medical conditions.
How is hypertrophic cardiomyopathy diagnosed and treated?
Hypertrophic cardiomyopathy is diagnosed with imaging tests and genetic testing. Treatment aims to manage symptoms and prevent complications.
What are the unique characteristics of arrhythmogenic right ventricular cardiomyopathy?
Arrhythmogenic right ventricular cardiomyopathy is caused by fatty infiltration in the right ventricle. It can lead to dangerous arrhythmias. It’s often genetic and requires careful management.
How is left ventricular non-compaction cardiomyopathy diagnosed?
Left ventricular non-compaction cardiomyopathy is diagnosed with imaging tests. These tests show the non-compacted myocardium. Identifying this condition can be challenging.
What are the treatment options for cardiomyopathy?
Treatment for cardiomyopathy varies based on the type and severity. It may include medications, lifestyle changes, devices, or surgery.
How do genetic factors contribute to cardiomyopathy?
Genetic mutations can cause cardiomyopathy, including hypertrophic and arrhythmogenic right ventricular cardiomyopathy. Genetic testing helps identify at-risk individuals.
What is the role of imaging techniques in diagnosing cardiomyopathy?
Imaging techniques like echocardiography and MRI are key in diagnosing cardiomyopathy. They provide detailed images of the heart.
References
- Mwalimu, J., & Cooper, A. (2024). Multiple variations in abdominal aorta branching with special reference to the presence of accessory renal arteries from an East African female cadaver. Surgical and Radiologic Anatomy, 46(8), 929-934. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11441833/