Can a Full Blood Count Detect Ovarian Cancer? Ovarian cancer is a big health worry, with nearly 20,000 new cases in the United States each year. Finding it early is key to treating it well. But, it’s often found too late. A full blood count (FBC) is a test that checks different parts of the blood.
So, can an FBC spot ovarian cancer? It’s not a direct test for this disease. Yet, some blood markers might show it’s there. Knowing how FBC helps find ovarian cancer can lead to better treatment.

Key Takeaways
- Ovarian cancer is a significant health concern in the United States.
- Early detection is key for effective treatment.
- A full blood count is a common test.
- Certain blood markers might show ovarian cancer.
- Understanding FBC’s role in finding ovarian cancer can improve diagnosis.
Understanding Ovarian Cancer
Ovarian cancer is a serious health issue for women. It starts quietly but grows quickly. Knowing about it helps find it early and treat it better.
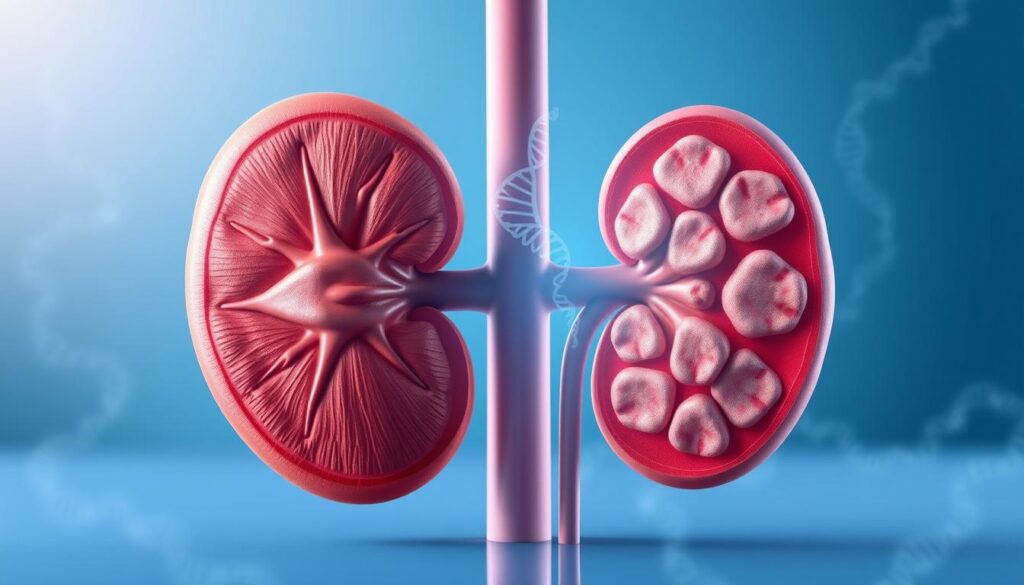
What is Ovarian Cancer?
Ovarian cancer starts in the ovaries, where eggs are made. It’s a complex disease with different types. The most common type is epithelial ovarian cancer, which starts in the outer layer of the ovaries.
Early ovarian cancer detection is hard because symptoms are not clear. There’s no good ovarian cancer screening tests yet. Scientists are working to find better ways to spot it in blood work.
Prevalence and Risk Factors
Ovarian cancer is the fifth leading cause of death in women in the U.S. Risk factors include genetic mutations, family history, age, and reproductive history. Women with BRCA1 or BRCA2 gene mutations are at higher risk.
Knowing these risks helps find women who need extra checks and prevention.
Common Symptoms and Warning Signs
Ovarian cancer symptoms are often vague and similar to other conditions. Symptoms include bloating, pelvic pain, trouble eating, and urgent need to urinate. Spotting these early ovarian cancer detection signs is key for timely checks.
If symptoms last or get worse, see a doctor. They can talk about ovarian cancer and how to diagnose it.
The Challenge of Early Ovarian Cancer Detection
Finding ovarian cancer early is hard because its symptoms are not clear. This cancer often grows quietly, making it hard to spot in the beginning.
Why Ovarian Cancer is Often Diagnosed Late
Ovarian cancer is often found late because its early signs are like other common issues. Symptoms like bloating, pain, and trouble eating are vague. They can be mistaken for other health problems.
Late diagnosis is a big worry because it changes treatment chances. Early detection means better treatment success. But, if it’s found late, treatment options are less effective.
The Importance of Early Detection
Finding ovarian cancer early is key to better survival rates. Early treatment can lead to better results. Studies show early-stage patients have a much higher five-year survival rate.
“Early detection is key to improving ovarian cancer survival rates. Advances in diagnostic techniques and increased awareness are critical in achieving this goal.”
Current Diagnostic Challenges
Even with new tech, finding ovarian cancer is tough. Current tests, like imaging and blood work, have their limits. For example, a full blood count (CBC) helps but isn’t a sure sign of ovarian cancer.
- Current screening methods lack specificity and sensitivity for early ovarian cancer detection.
- There is a need for more accurate and reliable diagnostic tests.
- Research is ongoing to develop better screening tools and methods.
To improve early detection, we need a few things. We must raise awareness about symptoms, create better screening tools, and improve how we diagnose.
What is a Full Blood Count (CBC)?
Understanding a full blood count (CBC) is key for patients and doctors. A CBC is a blood test that checks different parts of the blood. It gives important health information.
Components of a Full Blood Count
A CBC looks at several important parts:
- Red Blood Cell Count (RBC)
- White Blood Cell Count (WBC)
- Hemoglobin (Hb)
- Hematocrit (Hct)
- Platelet Count
Each part tells us about different health aspects. They help diagnose many conditions.
Normal Ranges and Values
Each CBC part has a normal range. These ranges can vary slightly between labs. Here are the general ranges:
| Component | Normal Range |
| RBC Count | 4.32-5.72 million cells/ µL (male) |
| WBC Count | 3.5-12.5 billion cells/L |
| Hemoglobin | 13.5-17.5 g/dL (male) |
| Hematocrit | 38.8-50.0% (male) |
| Platelet Count | 150,000-450,000/ µL |
Talking to a doctor is important to understand any results outside these ranges.
When Doctors Order a CBC
Doctors order a CBC for many reasons:
- To diagnose or monitor health issues like anemia, infection, or leukemia.
- As part of a routine check-up or physical exam.
- To check how the body reacts to certain medicines or treatments.
A CBC is a useful test. It gives important information for diagnosis and monitoring.
Full Blood Count Ovarian Cancer Detection Capabilities
A full blood count is a common test that might help find ovarian cancer. It looks at blood components for changes. This test is used to check health and find many conditions, like anemia or infections. Studies are looking into its use for ovarian cancer.
How Cancer Affects Blood Parameters
Cancer, like ovarian cancer, changes blood in many ways. It can cause inflammation, change blood cell production, and affect the immune system. These changes can show up in a full blood count, which checks different blood parts.
Inflammation is a big factor in how cancer changes blood. It can make some white blood cells go up and others go down. A CBC can spot this imbalance.
Specific Blood Count Changes in Ovarian Cancer
Research has found certain blood count changes linked to ovarian cancer. These include:
- Changes in white blood cell count, like more neutrophils.
- A higher neutrophil-to-lymphocyte ratio (NLR), which might mean cancer.
- Changes in red blood cells, like hemoglobin levels and RDW.
For example, a study found ovarian cancer patients often have a high NLR. This could be a sign of the disease.
| Blood Parameter | Change in Ovarian Cancer | Potential Significance |
| Neutrophil Count | Increase | Shows inflammation and might mean cancer |
| NLR | Increase | Could be a marker for ovarian cancer |
| RDW | Variation | May show nutritional issues or inflammation |
Sensitivity and Specificity of CBC for Cancer Detection
A full blood count can show changes linked to ovarian cancer. But, how well it works to find the disease is not clear. Sensitivity is about finding those with the disease, and specificity is about finding those without it.
“The role of CBC in ovarian cancer diagnosis is promising but requires further investigation to determine its true diagnostic tool.” – An Oncologist
Research says CBC can give useful info but isn’t enough on its own for diagnosis. It might be used with other tests, like imaging and biopsy, for a full check.
Red Blood Cell Parameters in Ovarian Cancer
Red blood cell parameters, like hemoglobin levels and red cell distribution width (RDW), change in ovarian cancer. These changes help us understand the disease’s progress and the patient’s health.
Hemoglobin Levels and Anemia
Anemia is common in cancer patients, including those with ovarian cancer. It causes fatigue, weakness, and shortness of breath. Studies show that anemia affects up to 40% of ovarian cancer patients, mostly in advanced stages.
Anemia in ovarian cancer comes from chronic disease, poor nutrition, and treatment side effects. Checking hemoglobin levels is key to managing anemia and improving patients’ lives.
Red Cell Distribution Width (RDW)
RDW shows how different red blood cells are in size. A high RDW means bigger differences in size, linked to cancer. Research finds that high RDW is tied to a worse prognosis in ovarian cancer.
The link between RDW and ovarian cancer prognosis is not clear. But it’s thought to be due to inflammation and oxidative stress, which harm red blood cell production and survival.
Hematocrit Changes
Hematocrit is the red blood cell part of blood. Changes in hematocrit levels happen in ovarian cancer patients. Watching hematocrit levels helps see how severe anemia is and if treatments work.
A study found that “Changes in hematocrit levels show underlying health issues, like cancer.” So, hematocrit is key in managing ovarian cancer.
“Understanding the changes in red blood cell parameters in ovarian cancer can lead to better diagnosis and management strategies.”
In summary, red blood cell parameters like hemoglobin levels, RDW, and hematocrit are important for ovarian cancer patients. Monitoring these can help catch complications early and tailor treatments.
White Blood Cell Parameters in Ovarian Cancer
Changes in white blood cell counts often show up in ovarian cancer patients. These changes can tell us a lot about how the disease is progressing and what the future might hold.
Neutrophil Count and Cancer
The neutrophil count is a key part of a patient’s white blood cell count. Studies have found that a high neutrophil count, or neutrophilia, is linked to many cancers, including ovarian cancer. Neutrophilia can show that the body is fighting the tumor with inflammation. In ovarian cancer, it might mean the disease is more aggressive and could have a worse outcome.
Lymphocyte Count in Ovarian Cancer
Lymphocytes are important white blood cells that help fight off infections. A higher lymphocyte count means the body is fighting cancer cells harder. Research shows that lymphocyte count can be a key factor in how well a patient will do with ovarian cancer. Higher counts are often linked to better results.
Neutrophil-to-Lymphocyte Ratio (NLR)
The neutrophil-to-lymphocyte ratio (NLR) combines neutrophil and lymphocyte counts into one number. A high NLR has been tied to lower survival rates and more advanced disease in cancers like ovarian cancer. The NLR is seen as a good tool for predicting how well a patient will do because it shows the balance between inflammation and the immune response.
In summary, white blood cell counts, including neutrophil, lymphocyte, and NLR, give us important clues about ovarian cancer’s outlook and how it’s progressing. Knowing these details can help doctors find better ways to treat the disease.
Inflammation Markers in Blood Tests
Inflammation is key in cancer growth, including ovarian cancer. It can cause genetic changes and help tumors grow. Blood tests for inflammation markers can show if cancer is present or getting worse.
C-Reactive Protein (CRP)
C-reactive protein (CRP) is made by the liver when there’s inflammation. High CRP levels are seen in infections, autoimmune diseases, and cancer. In ovarian cancer, high CRP levels mean the disease is more advanced and has a worse outlook.
CRP Levels and Cancer Prognosis
| CRP Level | Association with Ovarian Cancer |
| Normal (<1 mg/dL) | Less likely to be associated with advanced cancer |
| Elevated (1-3 mg/dL) | May indicate presence of cancer or other inflammatory conditions |
| Highly Elevated (>3 mg/dL) | Often associated with advanced disease or poor prognosis |
Erythrocyte Sedimentation Rate (ESR)
Erythrocyte sedimentation rate (ESR) shows how fast red blood cells settle. It’s not specific to cancer but high levels can mean there’s inflammation. This could be linked to cancer.
Relationship Between Inflammation and Cancer
The link between inflammation and cancer is complex. Chronic inflammation can help cancer grow and spread. CRP and ESR can help doctors understand cancer risk and treatment success.
Knowing how inflammation affects ovarian cancer is vital. Blood tests for inflammation markers help doctors see if cancer is present or getting worse.
Limitations of Blood Tests in Ovarian Cancer Detection
Testing for ovarian cancer in the blood is tricky. Blood tests can give clues, but they’re not enough to say for sure if you have cancer.
Sensitivity and Specificity Issues
Blood tests for ovarian cancer, like the CA-125 test, have big challenges. Sensitivity is about catching the disease correctly. Specificity is about not catching a disease when it’s not there. Both issues can cause wrong diagnoses.
The CA-125 test is often used but has its flaws. It can show high levels in conditions other than cancer, like endometriosis or pregnancy.
False Positives and False Negatives
False positives mean a test says you have cancer when you don’t. This can cause a lot of worry and extra tests. False negatives mean a test misses cancer when it’s there. This can delay getting the right treatment.
These problems show why blood tests alone aren’t enough for diagnosing ovarian cancer. We need a more complete way to check for cancer.
Why Blood Tests Alone Are Not Sufficient
Blood tests are just part of finding ovarian cancer. Other tools like ultrasound and MRI, and checking your body and medical history, are also key. Sometimes, surgery and a biopsy are needed to be sure.
| Diagnostic Method | Role in Ovarian Cancer Detection | Limitations |
| Blood Tests (CA-125) | Initial screening, monitoring recurrence | Limited sensitivity and specificity, false positives/negatives |
| Imaging Techniques (Ultrasound, MRI) | Visualizing tumors, assessing spread | May not detect early-stage cancer, requires expertise |
| Surgical Diagnosis and Biopsy | Definitive diagnosis, staging | Invasive, requires surgical expertise |
In short, blood tests help but have their limits. We need a mix of tests to find ovarian cancer accurately. Knowing these limits helps doctors and patients alike.
Comprehensive Approach to Ovarian Cancer Diagnosis
Diagnosing ovarian cancer is not just one test. It needs a mix of methods. This way, doctors can give the right treatment to patients.
Combining Blood Tests with Other Diagnostic Methods
Blood tests, like a full blood count (CBC), are key. But they work best with other tools. Using blood tests with imaging and clinical checks makes diagnosis better.
These tests help doctors spot signs of ovarian cancer. For example, blood changes can match what imaging shows. This helps confirm a diagnosis.
Imaging Techniques
Imaging is key in finding ovarian cancer. Ultrasound and CT scans help see the ovaries and find problems. They show how big, shaped, and what the masses are like.
| Imaging Technique | Description | Use in Ovarian Cancer Diagnosis |
| Ultrasound | Uses high-frequency sound waves to create images of the ovaries | Initial assessment of ovarian masses |
| CT Scan | Uses X-rays to create detailed cross-sectional images | Staging ovarian cancer and assessing spread |
| MRI | Uses magnetic fields and radio waves to create detailed images | Further evaluation of complex ovarian masses |
Surgical Diagnosis and Biopsy
Often, surgery and biopsy are needed for a clear diagnosis. Surgery lets doctors look at the ovaries and check for cancer spread.
During surgery, a piece of the mass is taken for lab tests. This biopsy is key to confirm cancer and its type and grade.
When to Consult a Doctor About Ovarian Cancer Concerns
Knowing when to see a doctor about ovarian cancer is key. Ovarian cancer is hard to find early. But knowing the signs can lead to quick medical checks.
Recognizing Warning Signs
Ovarian cancer symptoms can be tricky to spot. They might seem like other, less serious issues. Look out for:
- Persistent bloating or swelling in the belly
- Pelvic pain or discomfort that lasts
- Feeling full quickly or having trouble eating
- Needing to pee a lot or feeling urgent
- Changes in bowel habits, like constipation
If you notice these signs often, see a doctor right away.
What to Expect During Evaluation
When you talk to your doctor about ovarian cancer, expect a detailed check-up. This might include:
- Talking about your medical history to find risk factors
- A physical exam, including a pelvic check
- Imaging tests like ultrasound or CT scans
- Blood tests, including CA-125 levels
Your doctor might also talk about genetic tests if there’s a family history of ovarian or breast cancer.
Questions to Ask Your Healthcare Provider
Having questions ready can help you understand your situation. Ask:
| Question | Purpose |
| What are the possible causes of my symptoms? | Understand possible diagnoses |
| What tests do I need, and what do they involve? | Get ready for diagnostic tests |
| What are my treatment options if I have ovarian cancer? | Learn about treatment choices |
| Are there any clinical trials or new treatments available? | Find out about new treatment options |
Early detection and understanding your condition are key. They can greatly affect your treatment and outcomes. Don’t delay if you’re worried about ovarian cancer symptoms.
Living with Ovarian Cancer: Monitoring Through Blood Tests
Blood tests are key in managing ovarian cancer. They help doctors see if treatment is working and if the cancer might come back. These tests are important for tracking the disease and changing treatment plans as needed.
Treatment Response Monitoring
Blood tests are used to check how well treatment is working. CA-125 levels are a key marker for ovarian cancer. If CA-125 levels go down, it means treatment is working. But if they stay the same or go up, it might mean treatment isn’t working.
Checking blood counts, like complete blood counts (CBC), is also important. It helps doctors see how the patient is doing and if treatment is causing side effects. For example, chemotherapy can affect blood cell counts, which need to be watched closely.
| Blood Parameter | Normal Range | Significance in Ovarian Cancer |
| CA-125 | <35 U/mL | Tumor marker; elevated levels may indicate ovarian cancer or recurrence |
| Hemoglobin (Hb) | 12-16 g/dL (female) | Low levels may indicate anemia, a common side effect of treatment |
| White Blood Cell Count (WBC) | 4,500-11,000 cells/μL | Changes can indicate infection, inflammation, or bone marrow suppression due to treatment |
Recurrence Detection
Blood tests are also key in finding ovarian cancer again. Watching CA-125 levels can spot recurrence early, even before symptoms show. If CA-125 levels go up after treatment, it might mean the cancer has come back.
Long-term Surveillance Protocols
After treatment, it’s important to keep an eye on things. This means regular check-ups, imaging tests, and blood tests to watch for recurrence. How often these tests are done depends on the patient’s risk and cancer stage.
Surveillance plans are made just for each patient. They consider the cancer type, stage, treatment, and overall health.
Conclusion
Ovarian cancer is hard to diagnose because its symptoms are not clear and current tests have limits. A full blood count (CBC) is often used to check for health issues, including ovarian cancer. Even though a CBC can’t confirm ovarian cancer, it might show signs that suggest it.
The CBC’s role in finding ovarian cancer is to spot blood changes that could mean the disease is present. These changes might include different white blood cell counts or red blood cell distribution width. But, blood tests alone can’t be sure because they’re not very sensitive or specific.
To really diagnose ovarian cancer, doctors use a mix of blood tests, imaging, and other tests. This way, they can be more accurate and catch the disease early. This is key for good treatment. As science moves forward, new tests and biomarkers might help make diagnosing ovarian cancer even better.
FAQ
What is a full blood count (CBC) and how is it related to ovarian cancer detection?
A CBC is a blood test that checks different parts of your blood. It looks at red and white blood cells and platelets. It’s not a direct test for ovarian cancer. But, it can show signs of cancer, including ovarian cancer.
Can a CBC detect ovarian cancer?
A CBC alone can’t find ovarian cancer. But, it can give clues that help with diagnosis and tracking when used with other tests.
What changes in CBC parameters are associated with ovarian cancer?
Ovarian cancer can change your CBC results. This includes changes in hemoglobin, red cell distribution width (RDW), hematocrit, and more. It also affects neutrophil and lymphocyte counts and the neutrophil-to-lymphocyte ratio (NLR).
How does ovarian cancer affect hemoglobin levels?
Ovarian cancer can cause anemia, which means low hemoglobin. Anemia is common in cancer patients. It’s due to chronic disease, poor nutrition, and inflammation from cancer.
What is the significance of the neutrophil-to-lymphocyte ratio (NLR) in ovarian cancer?
The NLR shows inflammation levels in your body. High NLR values are linked to worse cancer outcomes, including ovarian cancer. They suggest more aggressive disease.
Are blood tests alone sufficient for ovarian cancer diagnosis?
No, blood tests alone can’t diagnose ovarian cancer. You need imaging like ultrasound and CT scans, and a biopsy for accurate diagnosis.
How are blood tests used in monitoring ovarian cancer?
Blood tests, like CBC and CA-125, help track treatment and watch for cancer return. They help doctors adjust treatment and catch problems early.
What are the limitations of blood tests in ovarian cancer detection?
Blood tests have limits in finding ovarian cancer. They can be not very sensitive or specific. This means they might miss some cancers or give false results.
When should I consult a doctor about ovarian cancer concerns?
If you have symptoms like bloating, pelvic pain, or abnormal bleeding, see a doctor. They can check your symptoms, do tests, and guide you on what to do next.
What questions should I ask my healthcare provider about ovarian cancer?
Ask your doctor about your risk for ovarian cancer, symptoms to watch for, tests they might do, and treatment options if you’re diagnosed.