Fundoscopic examination is key in modern ophthalmology. It lets doctors see the retina and spot important signs of diseases. This is true for both eye and body health issues. Learn fundoscopy papilloedema. This essential guide explains how to identify key findings in diabetic and glaucoma patients.
Fundoscopic examination is like a window into our health. It shows us things we can’t see with our eyes. This includes problems with blood vessels and nerves.
At Liv Hospital, we use fundoscopy in a big way. It helps us catch problems early, like papilloedema, diabetic retinopathy, and glaucoma. We follow the best practices and new methods to make sure we’re doing it right.
Key Takeaways
- Fundoscopic examination is key for spotting diseases in the eyes and body.
- Papilloedema is linked to high pressure in the brain.
- Diabetic retinopathy is a big problem for people with diabetes.
- Glaucoma can be seen through the shape of the optic cup in the eye.
- Finding these issues early is important for good treatment.
The Importance of Fundoscopic Examination
The fundoscopic examination is key in spotting and treating eye and body diseases. It lets doctors see the retina up close. This gives them important clues about eye health and helps find key problems.
Basic Principles of Fundoscopy
Fundoscopy looks inside the eye, at the retina and its parts. It’s about knowing what’s normal and spotting what’s not. Special tools help doctors see these important areas for a correct diagnosis.
Understanding fundoscopy basics is key to reading eye exams. It covers the science behind seeing inside the eye and how to do it right.
Normal Fundoscopic Anatomy
Healthy eyes show a clear optic disc, macula, and blood vessels. The optic disc should have clear edges and a normal size ratio. Knowing what’s normal helps doctors spot when something’s off.
- The optic disc is usually round or slightly oval.
- The macula is found next to the optic disc.
- Retinal vessels should not be twisted or too narrow.
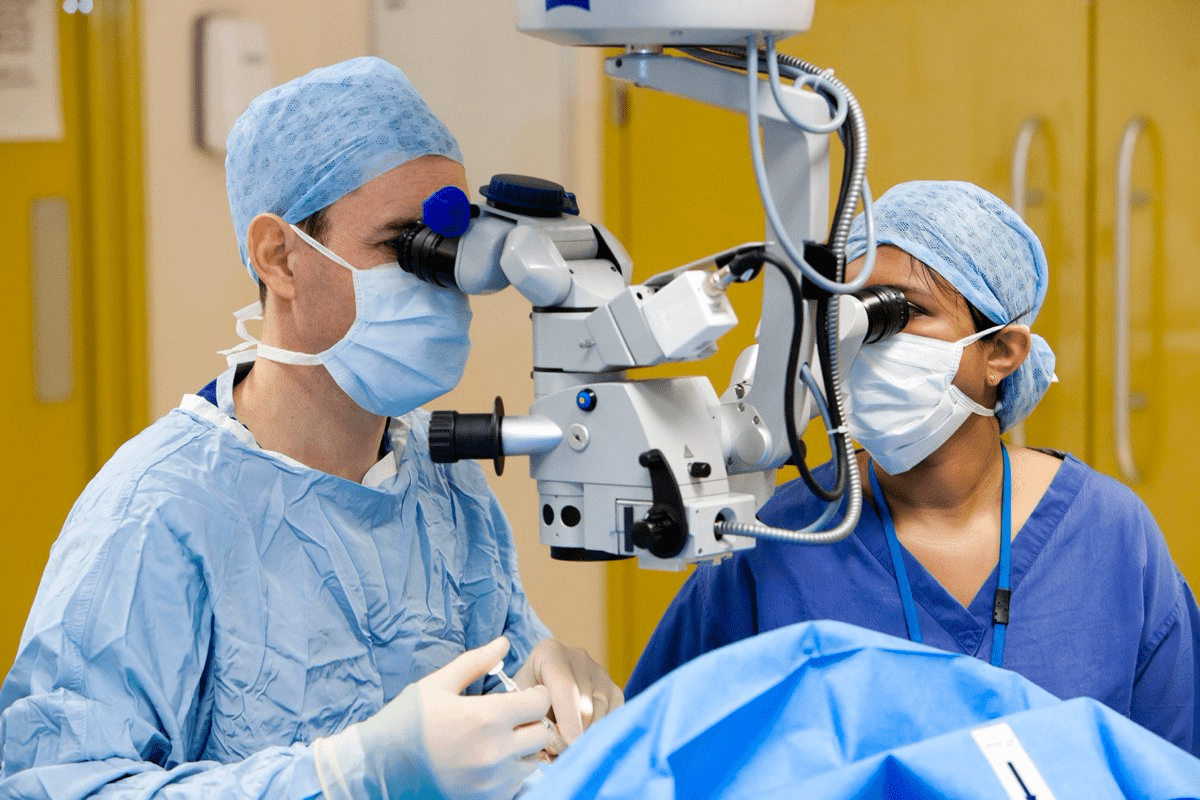
Equipment and Techniques
Fundoscopy can be done in two ways: direct or indirect ophthalmoscopy. Direct ophthalmoscopy gives a close-up view, while indirect ophthalmoscopy shows more. The choice depends on the situation and the doctor’s style.
Using the right tool and adjusting it to the patient’s eyes is important. This ensures a clear view of the retina.
Fundoscopy Papilloedema: Critical Diagnostic Features
Papilloedema is a serious condition where the optic disc swells due to high pressure inside the skull. It can be spotted through a fundoscopic exam. Knowing how it looks and why it happens is key to treating it right.
Pathophysiology of Increased Intracranial Pressure
High pressure inside the skull causes papilloedema. This pressure stops the flow of axoplasm at the optic nerve head. As a result, the optic disc swells, even if the vision seems normal at first.
Characteristic Appearances: Blurred Disc Margins and Venous Engorgement
Papilloedema shows up as blurred disc edges and veins that are too full. The disc might look red, and the normal cup in the center might be hidden. Venous engorgement is a big clue, showing the optic nerve sheath is under pressure.
Cotton Wool Spots and Hemorrhages
Papilloedema also brings cotton wool spots and bleeding around the optic disc. These signs mean the nerve fibers are under stress. Cotton wool spots show where the retina is not getting enough blood, and bleeding happens when tiny vessels burst.
Grading Systems and Management Approach
The Frisén scale helps doctors figure out how bad papilloedema is. This helps decide if urgent action is needed. Treatment aims to lower the pressure inside the skull, either with medicine or surgery.
“The Frisén scale provides a systematic approach to grading papilloedema, aiding in clinical decision-making.”
Frisén Scale Grade | Characteristics |
0 | Normal optic disc |
1 | Minimal blurring of the disc margin |
2 | Moderate blurring with elevation |
3 | Severe blurring with significant elevation |
In conclusion, papilloedema is a serious issue that needs quick action. A fundoscopy is key to spotting the signs of papilloedema. It helps doctors treat the high pressure and avoid worse problems.
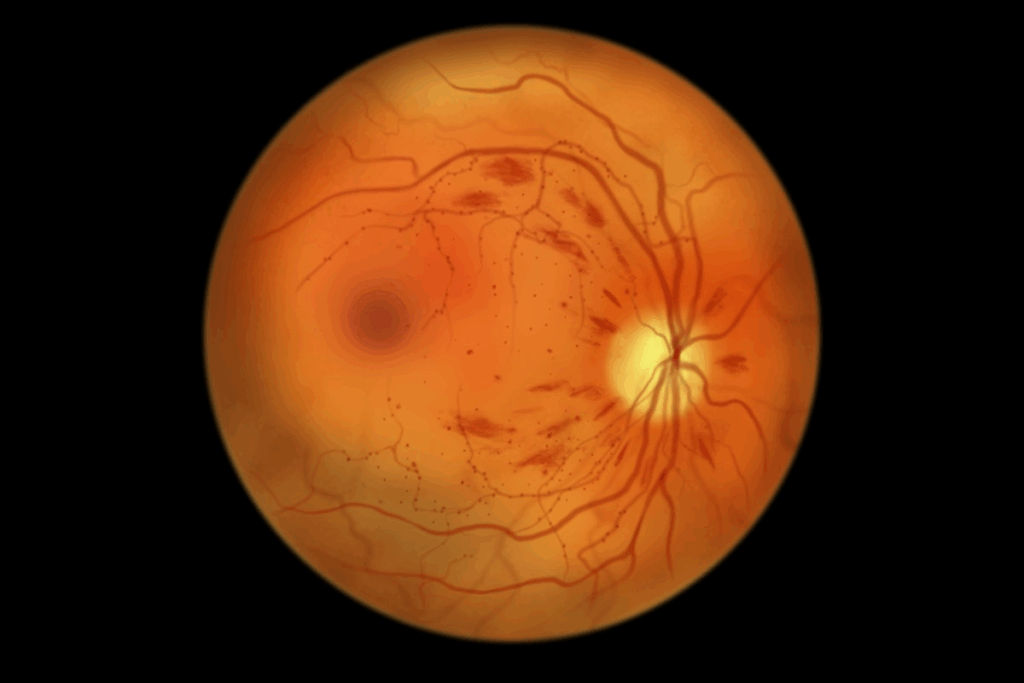
Diabetic Retinopathy: Spectrum of Vascular Changes
Diabetic retinopathy causes changes in blood vessels that can harm your vision if not treated. Looking at the eyes of people with diabetes, we see different signs of how bad the disease is.
Non-Proliferative Findings
At first, diabetic retinopathy shows signs like microaneurysms and dot-blot hemorrhages. Microaneurysms are small bulges in blood vessels. Dot-blot hemorrhages are tiny spots of blood in the retina. These are early signs seen during eye exams.
Progression to Cotton Wool Spots and Hard Exudates
As the disease gets worse, we see cotton wool spots and hard exudates. Cotton wool spots are white, fluffy spots from lack of blood flow. Hard exudates are fatty deposits that form around leaks in blood vessels.
Cotton wool spots mean there’s not enough blood flow. Hard exudates show long-term leaks. These signs mean the disease is getting more serious.
Proliferative Changes
When it gets even worse, we see proliferative diabetic retinopathy with neovascularization. This means new, weak blood vessels grow on the retina or optic disc. These can easily bleed, causing serious problems like vitreous hemorrhage or retinal detachment.
Proliferative diabetic retinopathy is a serious problem that needs quick treatment to save your sight.
Risk Factors
The chance of getting diabetic retinopathy depends on how long you’ve had diabetes and how well you control your blood sugar. People with diabetes for a long time or who don’t control their blood sugar well are at higher risk.
Knowing these risks helps catch diabetic retinopathy early. Regular eye exams are key to tracking the disease and deciding on treatment.
Glaucomatous Optic Neuropathy on Fundoscopy
Fundoscopic examination is key in spotting glaucomatous optic neuropathy. It shows changes in the optic nerve head. These include higher cup-to-disc ratios, cupping of the optic disc, and defects in the retinal nerve fiber layer. These signs are important for early detection and treatment.
Increased Cup-to-Disc Ratio Assessment
The cup-to-disc ratio is a key measure for glaucoma damage. A normal ratio is less than 0.5. In glaucoma, the cup grows, making the ratio higher. Getting this ratio right is critical for diagnosing and tracking glaucoma.
Optic Disc Cupping and Rim Thinning
Optic disc cupping is a key sign of glaucoma. As it gets worse, the rim of the optic disc thins, mainly in the bottom and top parts. This thinning often goes with visual field problems. It’s important to check the optic disc rim for early signs.
Retinal Nerve Fiber Layer Defects
Retinal nerve fiber layer (RNFL) defects are also a sign of glaucoma. These show up as thinning in the RNFL. New imaging methods help spot these defects early.
Correlation with Visual Field Loss
The changes seen in fundoscopy, like cupping and RNFL defects, match up with visual field losses. Knowing this link is key for doctors to diagnose and manage glaucoma well. Watching both structural and functional changes helps track the disease and see if treatments work.
Hypertensive Retinopathy: Vascular Manifestations
Hypertensive retinopathy shows clear signs of vascular changes. These signs are key to understanding how high blood pressure affects the retina.
Keith-Wagener-Barker Classification System
The Keith-Wagener-Barker system helps grade hypertensive retinopathy. It ranges from mild to severe, helping doctors assess the damage.
- Grade 1: Minimal narrowing or sclerosis of the retinal arterioles.
- Grade 2: Moderate to marked narrowing or sclerosis, with or without focal constriction.
- Grade 3: Severe changes including retinal hemorrhages, exudates, or cotton wool spots.
- Grade 4: Papilledema, in addition to the changes seen in Grade 3.
Arteriolar Narrowing and AV Nicking
Arteriolar narrowing and AV nicking are key signs of hypertensive retinopathy. Narrowing happens due to high blood pressure. AV nicking is when veins get compressed by thick arterioles.
Key Features:
- Arteriolar narrowing: A response to increased blood pressure.
- AV nicking: Indicates more severe vascular changes.
Distinguishing Features from Diabetic Retinopathy
Hypertensive and diabetic retinopathy both affect blood vessels in the retina. But they show different signs. Hypertensive retinopathy is marked by arteriolar narrowing and AV nicking. Diabetic retinopathy, on the other hand, shows microaneurysms, hemorrhages, and exudates.
“The differentiation between hypertensive and diabetic retinopathy is critical for proper treatment.” –
Retinal Specialist
Prognostic Implications for Systemic Hypertension
The severity of hypertensive retinopathy is important for patients with high blood pressure. Severe retinopathy signals a higher risk of heart problems and death.
Knowing this helps doctors manage high blood pressure better.
Age-Related Macular Degeneration Findings
Age-related macular degeneration (AMD) is a big cause of vision loss in older adults. It shows clear signs when we look into the eye. As we get older, the chance of getting AMD goes up, worrying both patients and doctors.
Dry AMD Characteristics
Dry AMD is the most common type, making up 85-90% of cases. When we look into the eye, we see drusen, yellow spots under the retina. These spots can vary in size and look.
Type of Drusen | Description |
Hard Drusen | Small, discrete, and yellowish deposits |
Soft Drusen | Larger, more confluent deposits that may be associated with a higher risk of progression |
As dry AMD gets worse, geographic atrophy can happen. This is when parts of the retina start to lose their color, causing vision problems.
Wet AMD Features
Wet AMD is less common but causes most severe vision loss. We see subretinal hemorrhage and fluid buildup because of new blood vessels. These changes can quickly make vision worse if not treated.
Progression Markers and Risk Assessment
Knowing how AMD progresses is key for early treatment. Risk factors include age, smoking, and family history. Regular eye checks can spot those at risk and track how the disease is moving.
By spotting AMD’s signs, doctors can start treatment early. This helps patients keep their vision better.
Retinal Vascular Occlusions
Retinal vascular occlusions are a major cause of sudden vision loss. They need quick diagnosis and treatment. These can be divided into arterial and venous occlusions, each showing different signs.
Arterial Occlusions: Pale Retina and Cherry-Red Spot
Arterial occlusions happen when the retinal arteries get blocked. This causes the retina to not get enough blood. When you look at the eye, you see a pale retina and a cherry-red spot in the fovea.
The cherry-red spot is because the choroidal circulation keeps the foveola supplied with oxygen and nutrients. The pale retina is due to swelling from lack of blood.
The severity of the blockage affects how pale the retina looks and the chances of getting your vision back. It’s very important to get the blood flowing again quickly to avoid lasting damage.
Venous Occlusions: Extensive Hemorrhages and Tortuosity
Venous occlusions happen when the retinal veins get blocked. When you look at the eye, you see extensive retinal hemorrhages and tortuosity of the retinal veins. The hemorrhages can be all over the retina and might have cotton wool spots, showing the retina isn’t getting enough blood.
Big retinal edema and hemorrhages can cause problems like macular edema and new blood vessels. Treating venous occlusions focuses on fixing these issues and improving blood flow to the retina.
Acute vs. Chronic Findings
Telling acute from chronic retinal vascular occlusions is key to choosing the right treatment. Acute occlusions happen suddenly and show signs of recent ischemia or bleeding. Chronic occlusions show signs of long-term damage, like thinning of the retina and a pale optic disc.
Knowing how long the occlusion has been there helps doctors decide how to treat it. They might need to act fast for acute cases or manage it over time for chronic ones.
Optic Neuritis and Neuroretinitis
It’s important to understand optic neuritis and neuroretinitis to diagnose and treat patients with possible multiple sclerosis. These conditions cause inflammation in the optic nerve. This leads to symptoms and changes seen in the eyes.
Distinguishing from Papilloedema
Optic neuritis and neuroretinitis can look like papilloedema because they both cause swelling in the optic disc. But, there are big differences. Papilloedema is linked to high pressure in the brain and affects both eyes. Optic neuritis usually affects one eye and has a different cause.
It’s vital to examine the patient carefully and ask about their medical history to tell these conditions apart.
Associated Systemic Conditions
Optic neuritis is often linked to multiple sclerosis, a disease that damages the protective covering of nerve fibers. Seeing optic neuritis might mean a patient has multiple sclerosis early on. Doctors should look for other diseases that could be causing the symptoms too.
Temporal Evolution of Findings
The signs of optic neuritis and neuroretinitis change over time. At first, you might see swelling in the optic disc. Then, a macular star might appear in neuroretinitis. Knowing how these signs change helps doctors make the right diagnosis and track the patient’s progress.
It’s important to see the patient regularly to check how they’re doing and if treatment is working.
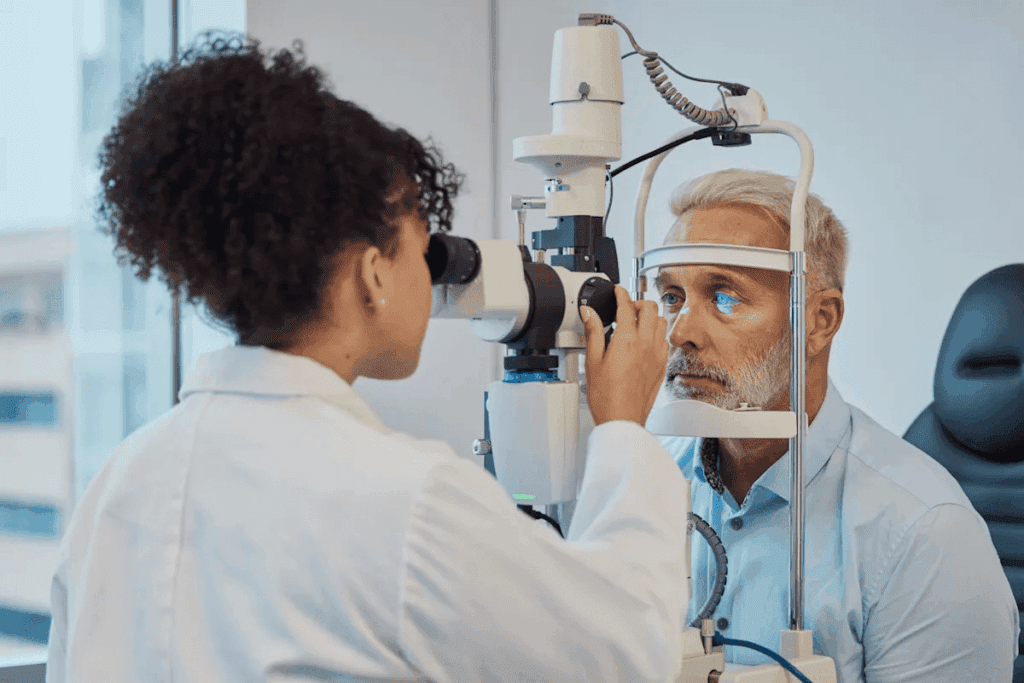
Techniques for Optimal Fundoscopic Examination
To get accurate diagnoses, healthcare pros need to use the best fundoscopic exam methods. This exam is key in eye care, helping to see the retina and other eye parts well.
Direct vs. Indirect Ophthalmoscopy
There are two main ways to do fundoscopic exams: direct and indirect ophthalmoscopy. Direct ophthalmoscopy gives a close-up look of the retina but only shows a small area. It’s great for checking the optic disc and macula.
Indirect ophthalmoscopy shows more of the retina but not as clearly. It’s best for seeing the outer parts of the retina. It’s often used with scleral depression to see even more.
Characteristics | Direct Ophthalmoscopy | Indirect Ophthalmoscopy |
Magnification | High | Low |
Field of View | Limited | Wide |
Usefulness | Optic disc, macula | Peripheral retina |
Pupillary Dilation Considerations
Pupillary dilation is key for a good fundoscopic exam. It lets you see more of the retina. Tropicamide and phenylephrine are common agents used. The right one depends on the patient and how long you need dilation.
Documentation and Photography
It’s important to document fundoscopic findings for patient care. Fundus photography is great for tracking changes in the retina. It gives a permanent record for future exams.
Learning these techniques helps healthcare pros do better fundoscopic exams. This makes diagnoses more accurate and effective.
Clinical Significance and Differential Diagnosis
Understanding fundoscopic findings is key to spotting serious eye problems. These exams help doctors make accurate diagnoses and plan treatments. We’ll look at how to tell serious eye issues from minor ones, and when to send patients to eye specialists.
Emergent vs. Non-Emergent Findings
Some eye problems need quick action to avoid serious damage. Issues like papilloedema, retinal detachment, and central retinal artery occlusion are urgent. It’s important to know which problems are serious and need fast treatment.
For example, sudden vision loss with a cherry-red spot means a patient needs to see an eye doctor right away. This could be a sign of a serious problem. But, age-related eye changes are not as urgent.
Systemic Disease Correlations
Fundoscopic exams can show signs of diseases like diabetes, high blood pressure, and multiple sclerosis. For instance, diabetic retinopathy shows up in people with diabetes who don’t control their blood sugar well. High blood pressure can also be seen in the eyes, helping doctors understand heart health.
Systemic Disease | Fundoscopic Findings |
Diabetes | Microaneurysms, dot-blot hemorrhages, cotton wool spots |
Hypertension | Arteriolar narrowing, AV nicking, retinal hemorrhages |
Multiple Sclerosis | Optic neuritis, retinal nerve fiber layer thinning |
When to Refer to Ophthalmology
Deciding when to send a patient to an eye doctor is very important. Patients with serious eye problems need to see a specialist right away. Also, those with complex or unclear cases should be referred for better care.
“The ophthalmologist plays a critical role in the diagnosis and management of ocular and systemic diseases, and timely referral is essential for optimal patient outcomes.”
— Expert Opinion
In summary, knowing how to interpret eye exams is vital for good patient care. By spotting serious problems, understanding related diseases, and knowing when to refer, we can help our patients get the best care.
Conclusion
Fundoscopic examination is key in eye care. It lets doctors see the retina up close. This helps them spot problems linked to eye and body diseases.
Knowing how to do a fundoscopic exam is critical. It helps doctors find and treat issues like swelling in the optic nerve and eye damage from diabetes. This leads to better care for patients.
We stress the value of fundoscopic exams in eye care today. They help doctors give better care to patients with eye problems. This way, patients get the help they need sooner.
FAQ
What is fundoscopic examination, and why is it important?
Fundoscopic examination is a tool used in eye care. It lets doctors see the retina and spot problems. This is key for diagnosing and treating diseases like papilloedema, diabetic retinopathy, and glaucoma.
What are the characteristic features of papilloedema on fundoscopic examination?
Papilloedema shows as swelling of the optic disc. It’s caused by high pressure in the brain. Look for blurred disc edges, veins that are too full, cotton wool spots, and blood spots.
How does diabetic retinopathy progress, and what are its characteristic features on fundoscopy?
Diabetic retinopathy starts with small blood vessel problems. It then gets worse, showing signs like tiny blood spots, more blood spots, cotton wool spots, and new blood vessels.
What are the fundoscopic features of glaucomatous optic neuropathy?
Glaucoma makes the optic disc look different. You’ll see a bigger cup in the center and damage to the nerve layer. These changes can lead to vision loss.
How does hypertensive retinopathy manifest on fundoscopy, and how is it distinguished from diabetic retinopathy?
Hypertensive retinopathy shows as narrow blood vessels and a specific sign called AV nicking. It’s different from diabetic retinopathy because it doesn’t have tiny blood spots or hard exudates.
What are the characteristic features of age-related macular degeneration on fundoscopic examination?
Age-related macular degeneration shows as drusen, which are yellow spots, and areas where the retina is missing. It also has blood spots under the retina. These signs help doctors diagnose and manage the condition.
What are the fundoscopic features of retinal vascular occlusions?
Arterial occlusions show a pale retina and a cherry-red spot. Venous occlusions have lots of blood and twisted blood vessels. These signs help doctors figure out what’s happening and how to treat it.
How is optic neuritis distinguished from papilloedema on fundoscopic examination?
Optic neuritis has swelling of the optic disc and a star shape in the macula. It’s different from papilloedema because of these signs. Knowing the difference helps doctors treat it right.
What are the advantages and disadvantages of direct and indirect ophthalmoscopy?
Direct ophthalmoscopy gives a close-up view. Indirect ophthalmoscopy shows more of the retina. Each has its own benefits and drawbacks, depending on what the doctor needs to see.
When should a patient be referred to ophthalmology based on fundoscopic findings?
If a patient has serious eye problems like retinal detachment, they need to see an eye doctor right away. For less urgent issues, like age-related macular degeneration, they can wait a bit.
What is the significance of cotton wool spots on fundoscopy?
Cotton wool spots mean the retina isn’t getting enough blood. They can be seen in diseases like diabetic retinopathy, high blood pressure, and blood vessel problems in the eye.
How does fundoscopic examination aid in the diagnosis of systemic diseases?
Fundoscopy can show signs of diseases like high blood pressure and diabetes. This helps doctors catch these conditions early and treat them.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10332214/