At Liv Hospital, we know that Gastroesophageal Reflux Disease (GERD) is a common problem. It happens when stomach acid flows back up into the esophagus. This can cause pain and may lead to more serious issues.
The NCBI Bookshelf says GERD is when stomach acid goes back up into the esophagus. It can even go further, into the mouth, throat, or lungs. This backflow can make people feel uncomfortable, from mild to severe, and can really affect their daily life.
We believe it’s key to know what GERD is and its medical definition. Knowing about GERD helps patients understand their condition better. This way, they can make informed choices about their treatment.
This is your ultimate GERD pain location guide. Learn 5 common areas for pain, from the chest and throat to the back, and why it happens.
Key Takeaways
- GERD is a chronic gastrointestinal disorder.
- It occurs when stomach contents flow back into the esophagus.
- GERD can cause a range of symptoms and potentially lead to complications.
- Understanding GERD is key for effective diagnosis and treatment.
- Liv Hospital offers complete care for GERD patients.
Understanding GERD: Definition and Overview
To understand GERD, we need to know its medical terms and how it differs from other reflux conditions. Gastroesophageal reflux disease, or GERD, is a long-term condition. It happens when stomach contents flow back into the esophagus, causing symptoms and possible complications.
What GERD Stands for in Medical Terms
GERD means Gastroesophageal Reflux Disease. In simple terms, Gastroesophageal refers to the stomach and esophagus. Reflux means stomach contents flowing back up. And Disease shows it’s a serious condition, not just a temporary issue.
The American College of Gastroenterology says GERD is when symptoms or damage in the esophagus happen because of stomach acid flowing back up.
The Difference Between GERD and Occasional Acid Reflux
Occasional acid reflux is common and usually not serious. But GERD is more severe and long-lasting. The main difference is in how often and how badly symptoms happen, and the risk of damage to the esophagus.
Occasional acid reflux might happen after eating a lot or when lying down. But it doesn’t cause the ongoing problems or damage that GERD does. Knowing the difference is key for getting the right treatment.
GERD as a Chronic Gastrointestinal Disorder
GERD is seen as a chronic gastrointestinal disorder because it causes ongoing symptoms in the digestive system. Because it’s chronic, it needs ongoing care and treatment to avoid serious problems like esophagitis or Barrett’s esophagus.
Seeing GERD as a long-term issue, not just a short-term problem, is important. It helps patients get the right medical help and make lifestyle changes to manage their symptoms better.
The Global Impact of GERD: Prevalence and Statistics
GERD is a big worry worldwide, with different rates in different places. It’s a long-term problem that affects the stomach and intestines. It impacts people in many ways, across different groups and areas.
GERD Prevalence Across Different Regions
In 2019, there were about 783.95 million GERD cases worldwide. The rates vary a lot, from 10 percent to 27.8 percent. This difference comes from many things, like what people eat, how they live, and their genes.
Regional variations in GERD rates are clear. For example, Western countries have more cases than some Eastern ones. This is because of diet, obesity, and lifestyle differences.
Age and Gender Distribution
GERD can happen to anyone, but it’s more common with age. Older people are more likely to get it. This might be because their stomach moves less and they face more risks over time.
Research shows GERD affects both men and women, but men might get it a bit more. The exact reason is not known. It could be because of hormones or body differences.
Economic Impact of GERD
The cost of GERD is huge, with both direct and indirect expenses. Direct costs include medical bills like drugs, hospital stays, and tests. Indirect costs are lost work time and lower quality of life.
GERD costs a lot, with billions spent on healthcare each year. It also affects daily life and sleep, making it hard to do everyday things.
The Pathophysiology of GERD
Understanding GERD’s pathophysiology is key to knowing how it develops and worsens. It involves several mechanisms that cause its symptoms.
Lower Esophageal Sphincter Dysfunction
The lower esophageal sphincter (LES) plays a big role in GERD. It’s a muscle ring that separates the esophagus and stomach. In GERD, the LES might be weak or relax too much, letting stomach acid flow back up.
This can happen for many reasons, like transient LES relaxations. These aren’t linked to swallowing. They can cause reflux, often after eating or when lying down.
Esophageal Dysmotility
Esophageal dysmotility means food moves abnormally through the esophagus. In GERD, this can mean the muscles don’t push food down well. This weakens peristalsis, the movement that moves food towards the stomach.
When peristalsis is weak, food stays in the esophagus longer. This means the esophagus is exposed to stomach acid for longer. This can make GERD symptoms worse.
Increased Intra-abdominal Pressure
Higher intra-abdominal pressure also plays a part in GERD. This can be due to things like being overweight, being pregnant, or wearing tight clothes.
Higher pressure in the belly can push stomach acid up towards the esophagus. This is more likely if the LES is weak or not working right.
| Pathophysiological Mechanism | Description | Impact on GERD |
|---|---|---|
| Lower Esophageal Sphincter Dysfunction | Weakness or inappropriate relaxation of the LES | Increased reflux of stomach contents into the esophagus |
| Esophageal Dysmotility | Abnormal movement of food through the esophagus | Delayed clearance of refluxed material, prolonging esophageal exposure to acid |
| Increased Intra-abdominal Pressure | Elevated pressure within the abdominal cavity | Increased likelihood of reflux, specially with a weak LES |
Knowing these mechanisms is key to treating GERD. Healthcare providers can then use targeted treatments to manage symptoms and prevent complications.
Common GERD Symptoms and Warning Signs
Knowing the symptoms of GERD is key to managing it well. We’ll look at the different signs of GERD, from common to rare. We’ll also talk about when you should see a doctor.
Classic Symptoms: Heartburn and Regurgitation
The most common signs of GERD are heartburn and regurgitation. Heartburn feels like a burning in your chest, often after eating. It can get worse at night. Regurgitation makes stomach acid come back up into your mouth, leaving a sour taste.
These symptoms are not just uncomfortable. They can also mess up your daily life and sleep.
Atypical Symptoms of GERD
GERD can also show up in different ways. Some people might feel chest pain that feels like a heart problem. Others might have a chronic cough or asthma-like symptoms because of stomach acid going into their lungs.
It’s important to know these signs to get the right treatment.
When Symptoms Require Immediate Medical Attention
Some symptoms need you to see a doctor right away. If you have difficulty swallowing, severe chest pain, or vomiting blood, get help fast. These could mean serious problems like esophageal stricture or bleeding.
If your symptoms don’t get better or get worse, talk to your doctor. They can change your treatment plan.
GERD Pain Location: Where and Why It Hurts
Knowing where GERD pain is located is key to treating it right. GERD happens when stomach acid flows back up into the esophagus. This can cause pain among other symptoms.
Chest Pain Behind the Breastbone
GERD pain often hits right behind the breastbone, or sternum. This can be scary because it might feel like heart pain. The pain comes from the acid irritating the esophagus lining.
Key characteristics of chest pain in GERD:
- Typically felt behind the breastbone
- Can be triggered or worsened by eating
- May be accompanied by a sour taste in the mouth
Throat and Upper Abdominal Pain
GERD pain can also show up in the throat or upper belly. Throat pain might make swallowing hard or feel like there’s a lump. Belly pain can be mistaken for other stomach problems.
Understanding these variations is key for the right diagnosis.
Radiation Patterns of GERD Pain
GERD pain can spread to the back, arms, or jaw, but this is rare. This spread can make it hard to tell if it’s GERD or heart pain.
Differentiating GERD Pain from Cardiac Issues
Telling GERD pain from heart pain is important because heart problems are serious. Both can cause chest pain, but they act differently and have different causes.
| Characteristics | GERD Pain | Cardiac Pain |
|---|---|---|
| Trigger | Eating, lying down | Exertion, stress |
| Nature of Pain | Burning, squeezing | Pressure, heaviness |
| Relief | Antacids, sitting up | Nitroglycerin, rest |
Seeing a doctor is vital for a correct diagnosis. Telling GERD from heart pain can be tricky and needs a pro’s eye.
Risk Factors and Causes of GERD
Understanding GERD’s risk factors and causes is key to managing and preventing it. GERD, or gastroesophageal reflux disease, affects millions globally. We’ll look at the factors that lead to and worsen GERD.
Lifestyle and Dietary Factors
Lifestyle and diet greatly impact GERD. Obesity puts extra pressure on the stomach, causing acid to flow up. Smoking weakens the LES and lowers saliva, which helps neutralize acid.
Diet also plays a part. Eating large or fatty meals can relax the LES. Foods like citrus fruits, tomatoes, chocolate, and spicy foods can also trigger symptoms. Keeping a food diary helps identify and avoid personal triggers.
| Lifestyle Factor | Impact on GERD |
|---|---|
| Obesity | Increases abdominal pressure, causing acid reflux |
| Smoking | Weakens LES and reduces saliva production |
| Large or fatty meals | Relaxes LES, allowing acid to flow back into the esophagus |
Medical Conditions Associated with GERD
Some medical conditions raise the risk of GERD. A hiatus hernia weakens the LES, leading to acid reflux. Conditions like diabetes, scleroderma, and gastroparesis can also cause GERD symptoms.
“The presence of a hiatus hernia can significantly compromise the function of the lower esophageal sphincter, leading to increased risk of GERD.”
— Medical Expert
Medications That Can Trigger or Worsen GERD
Some medications can make GERD worse. Calcium channel blockers, benzodiazepines, and certain antidepressants relax the LES. NSAIDs and bisphosphonates can also irritate the esophagus, making symptoms worse.
- Calcium channel blockers
- Benzodiazepines
- Certain antidepressants
- NSAIDs
- Bisphosphonates
Diagnosing GERD: Tests and Procedures
To diagnose GERD, doctors use several steps. They start with initial checks, look at the patient’s medical history, and do special tests. This helps figure out how bad the condition is and if other things could be causing symptoms.
Initial Evaluation and Medical History
The first step in diagnosing GERD is a detailed check and a look at the patient’s medical history. Doctors examine symptoms like heartburn and how often they happen. They also ask about diet and any medicines that might make symptoms worse.
Doctors also think about the patient’s overall health and past treatments. This info helps decide the best tests and treatments.
Diagnostic Tests for GERD
There are several tests to confirm GERD and see how severe it is. These include:
- Endoscopy: This lets doctors see the esophagus, stomach, and duodenum. It helps find any damage or problems from GERD.
- Ambulatory pH Monitoring: This test checks acid levels in the esophagus for 24 hours. It shows how often and long acid reflux happens.
- Esophageal Manometry: This test checks how well the esophagus and lower esophageal sphincter work. It helps find any problems with how they move.
Ruling Out Other Conditions
It’s important to tell GERD apart from other conditions that might have similar symptoms. These include eosinophilic esophagitis and peptic ulcer disease. Doctors use tests and checks to make sure they get the right diagnosis.
By accurately diagnosing GERD, doctors can create a treatment plan that really works. This helps improve the patient’s life a lot.
Treatment Options for GERD
Managing GERD needs a mix of lifestyle changes, medication, and sometimes surgery. We’ll look at the different ways to treat it, so you can find the best way to manage your condition.
Lifestyle Modifications
Making big lifestyle changes is often the first step against GERD. These changes can help lessen symptoms and improve digestion.
- Dietary Changes: Stay away from foods like citrus fruits, tomatoes, chocolate, and fatty or fried foods to cut down on symptoms.
- Weight Management: Keeping a healthy weight can ease pressure on your stomach, which helps reduce GERD symptoms.
- Elevating the Head of the Bed: Raising your bed’s head by 6-8 inches can stop stomach acid from flowing into your esophagus while you sleep.
- Avoiding Late-Night Eating: Don’t eat at least 2-3 hours before bedtime to lessen nighttime symptoms.
A gastroenterology expert says, “Lifestyle changes are key in managing GERD symptoms and can greatly improve life quality for patients.”
“The key to managing GERD is making sustainable lifestyle changes that reduce symptoms and improve overall health.”
Medication Therapies
For many, lifestyle changes aren’t enough, and medication is needed. There are many medications, each with its own benefits.
- Antacids: Give quick relief by neutralizing stomach acid.
- H-2-Receptor Blockers: Cut down acid production in the stomach.
- Proton Pump Inhibitors (PPIs): More effective than H-2-receptor blockers, PPIs block acid production and help the esophagus heal.
Talking to a healthcare provider is key to finding the right medication and dosage. A medical expert notes, “The right medication can make a big difference in managing GERD symptoms.”
Surgical and Endoscopic Interventions
For severe GERD that doesn’t get better with lifestyle changes and medication, surgery or endoscopy might be needed. These methods aim to strengthen the lower esophageal sphincter and stop acid reflux.
- Fundoplication: A surgery that wraps the top of the stomach around the lower esophagus to strengthen the sphincter.
- LINX Device: A ring of magnetic beads placed around the stomach and esophagus junction to prevent reflux.
- Endoscopic Procedures: Techniques like Stretta and TIF (Transoral Incisionless Fundoplication) are less invasive than traditional surgery.
These advanced treatments can help those with severe GERD. It’s important to talk to a healthcare professional to find the best treatment.
Complications of Untreated GERD
If GERD is not treated, it can cause many problems. These issues can harm a person’s health in many ways. They can also make life much harder and, in some cases, very dangerous.
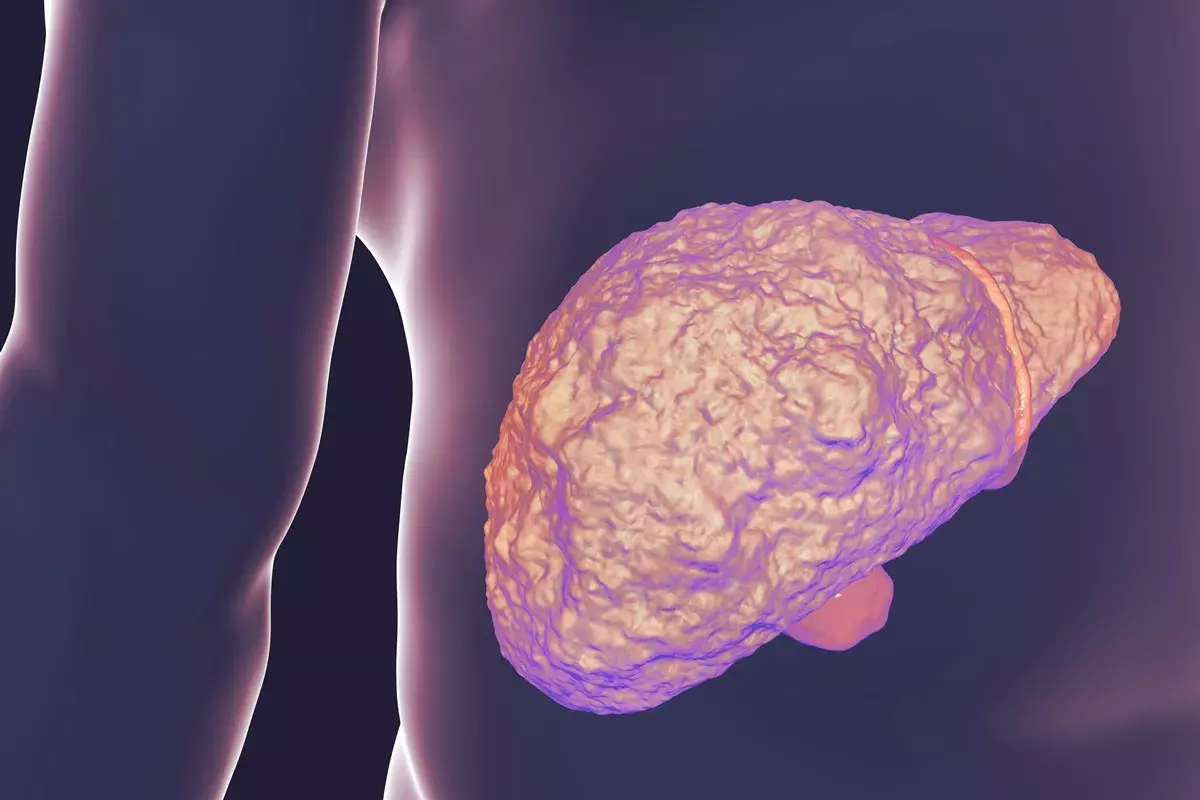
Esophageal Damage and Barrett’s Esophagus
Stomach acid can damage the esophagus over time. This can lead to esophagitis, strictures, and ulcers. A big worry is Barrett’s esophagus, where the esophagus lining changes to abnormal cells. This can lead to esophageal cancer.
The American Gastroenterological Association says, “Barrett’s esophagus is a complication of chronic GERD and is associated with an increased risk of esophageal adenocarcinoma.”
“The presence of Barrett’s esophagus is a significant risk factor for the development of esophageal adenocarcinoma, highlighting the importance of surveillance and management of GERD.”
Respiratory Complications
GERD can also harm the lungs. When stomach contents go into the lungs, it can cause chronic cough, asthma, and pneumonitis. In bad cases, it can lead to pulmonary fibrosis.
| Respiratory Complication | Description |
|---|---|
| Chronic Cough | A persistent cough often associated with GERD due to acid reflux irritating the throat. |
| Asthma | GERD can make asthma symptoms worse by causing acid reflux, which irritates the airways. |
| Pneumonitis | Inflammation of the lung tissue due to aspiration of stomach contents. |
Impact on Quality of Life
Untreated GERD can really hurt a person’s life. It can cause pain, discomfort, and trouble swallowing. This can make someone feel anxious, depressed, and want to stay away from people.
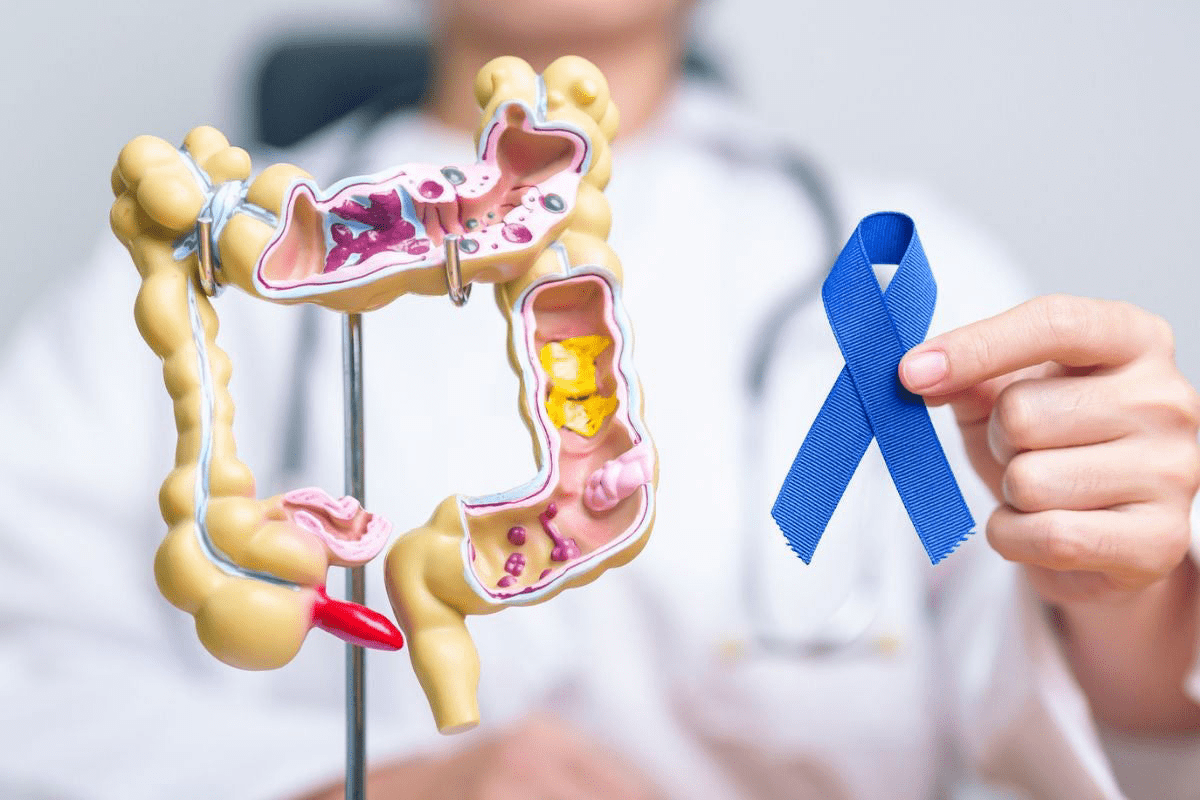
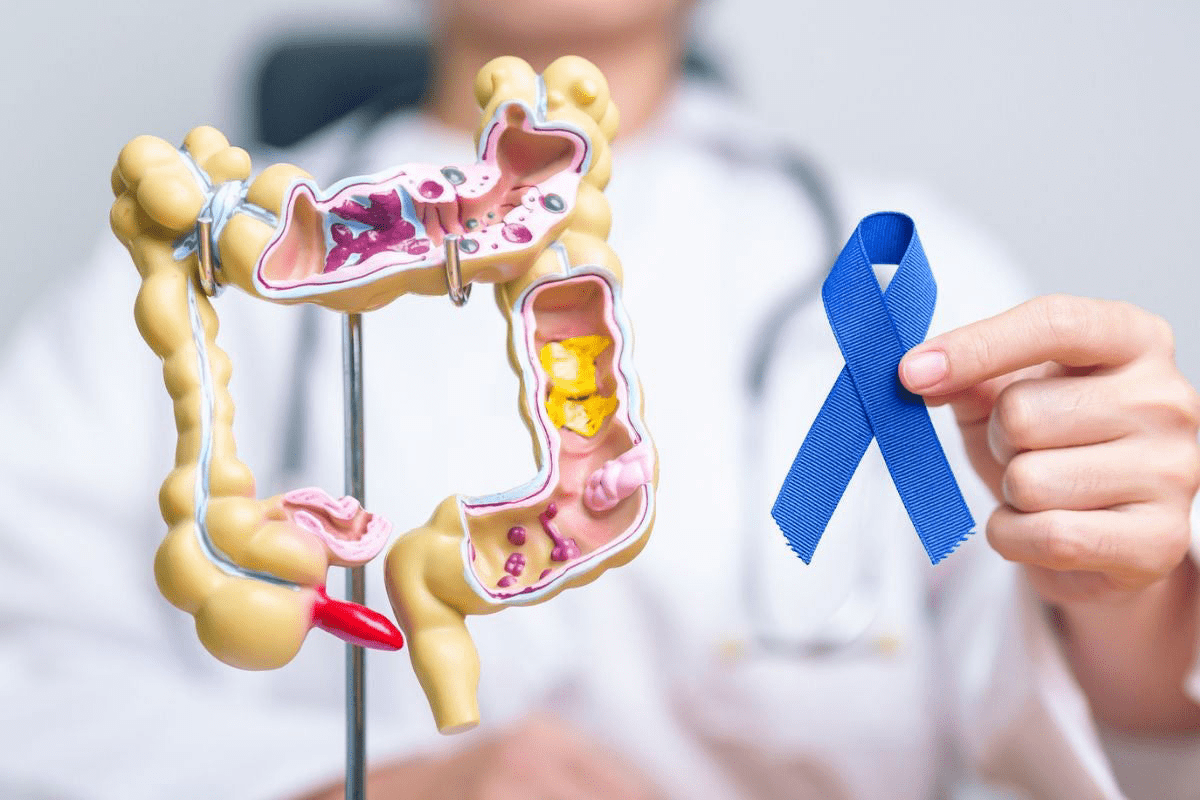
Risk of Esophageal Cancer
One of the worst things about untreated GERD is the risk of esophageal cancer. The long-term damage and inflammation can lead to adenocarcinoma, a serious type of esophageal cancer.
It’s very important to manage GERD symptoms to avoid these problems. Early treatment can greatly lower the chance of serious conditions.
Living with GERD: Management Strategies
Managing GERD well needs a mix of diet changes, lifestyle tweaks, and stress control. These steps can lessen symptoms and boost life quality.
Dietary Adjustments for GERD Relief
Diet is key in managing GERD. Some foods can make symptoms worse, while others help. Avoiding trigger foods like citrus fruits, tomatoes, chocolate, and spicy or fatty foods is a good start.
Adding GERD-friendly foods to your diet can also help. These include:
- Lean proteins like chicken and fish
- Low-fat dairy products
- Non-citrus fruits like bananas and melons
- Vegetables like green beans and broccoli
- Whole grains like brown rice and oatmeal
| Food Category | Recommended Foods | Foods to Avoid |
|---|---|---|
| Fruits | Bananas, Melons | Citrus Fruits, Tomatoes |
| Proteins | Lean Chicken, Fish | Fatty Meats, Fried Foods |
| Dairy | Low-fat Yogurt, Milk | High-fat Cheese, Cream |
Sleep Positioning and Lifestyle Changes
Sleep position affects GERD symptoms. Elevating the head of the bed by 6-8 inches helps prevent acid reflux during sleep.
Other lifestyle changes are also important. Keeping a healthy weight, wearing loose clothes, and not lying down after eating can help manage symptoms.
Stress Management Techniques
Stress can make GERD symptoms worse. Stress-reducing activities like meditation, deep breathing, or yoga can help lessen symptoms.
When to Consider Alternative Therapies
Some people find relief in alternative treatments like acupuncture or herbal supplements. But, always talk to a healthcare provider before trying these to make sure they’re safe and work well.
Conclusion: Taking Control of Your GERD
Understanding GERD, or Gastroesophageal Reflux Disease, is key to managing it well. Knowing what it is, its symptoms, how it’s diagnosed, and treatment options helps patients take charge. This way, they can improve their life quality.
To manage GERD, making smart lifestyle changes is important. Following medication advice and considering surgery or endoscopy when needed is also vital. GERD affects millions, causing discomfort and serious problems if not treated.
By managing GERD, people can reduce symptoms, avoid long-term damage, and feel better overall. We urge patients to team up with healthcare experts. Together, they can create a plan to manage GERD. This way, patients can control their condition and get better health results.
FAQ
What does GERD stand for in medical terms?
GERD stands for Gastroesophageal Reflux Disease. It’s a chronic condition where stomach acid flows back into the esophagus.
What is the difference between GERD and occasional acid reflux?
Occasional acid reflux is common. But GERD is a chronic issue that can cause a lot of discomfort. It can also lead to serious problems if not treated.
Is GERD a gastrointestinal disorder?
Yes, GERD is a chronic disorder of the digestive system. It affects the esophagus and can cause symptoms like heartburn and regurgitation.
What are the classic symptoms of GERD?
Classic GERD symptoms include heartburn and regurgitation. Other symptoms can be chest pain and trouble swallowing.
What are the risk factors for developing GERD?
Risk factors for GERD include obesity and eating certain foods. Medical conditions and some medications also play a role.
How is GERD diagnosed?
Doctors diagnose GERD by looking at your medical history and doing a physical exam. They might also use tests like endoscopy and pH monitoring.
What are the treatment options for GERD?
Treatments for GERD include changing your diet and lifestyle. Medications and sometimes surgery or endoscopy are also options. They aim to reduce symptoms and prevent complications.
Can GERD lead to complications if left untreated?
Yes, untreated GERD can cause serious problems. These include damage to the esophagus, Barrett’s esophagus, breathing issues, and an increased risk of esophageal cancer.
How can I manage GERD symptoms?
To manage GERD symptoms, make dietary changes and adopt a healthy lifestyle. Stress management and alternative therapies can also help.
What is the global impact of GERD?
GERD affects millions worldwide, causing a big economic burden on healthcare systems. It has a significant global impact.
Can GERD be differentiated from cardiac issues?
Yes, it’s important to tell GERD pain from heart problems. The symptoms can be similar. Getting the right diagnosis is key for effective treatment.
What is the pathophysiology of GERD?
GERD happens because of problems with the lower esophageal sphincter and esophageal motility. Increased pressure in the abdomen also plays a role, causing stomach acid to flow back into the esophagus.
References
https://my.clevelandclinic.org/health/diseases/17019-gastroesophageal-reflux-disease-gerd