Patients who get allogeneic hematopoietic stem cell transplantation face a big risk. They might get graft vs host disease in their lungs.
Up to 9% of those who get transplanted will see their lungs affected. This can be very dangerous and affect their life quality a lot.
At Liv Hospital, we use the newest ways to fight this serious problem. Our team focuses on each patient, giving them the best care for lung issues after stem cell transplants.
It’s key to grasp how GVHD affects the lungs to better care for transplant patients. GVHD in the lungs is a serious and potentially deadly issue that can happen after a transplant.
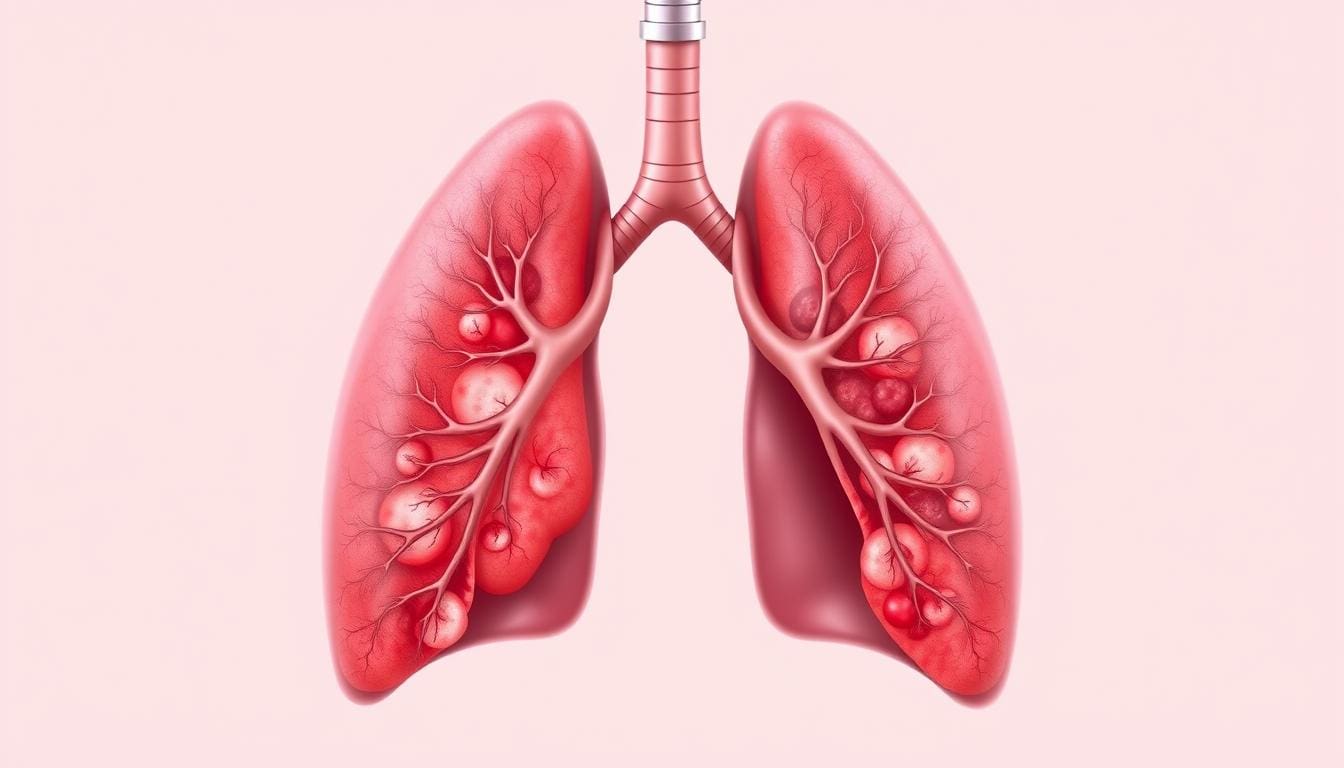
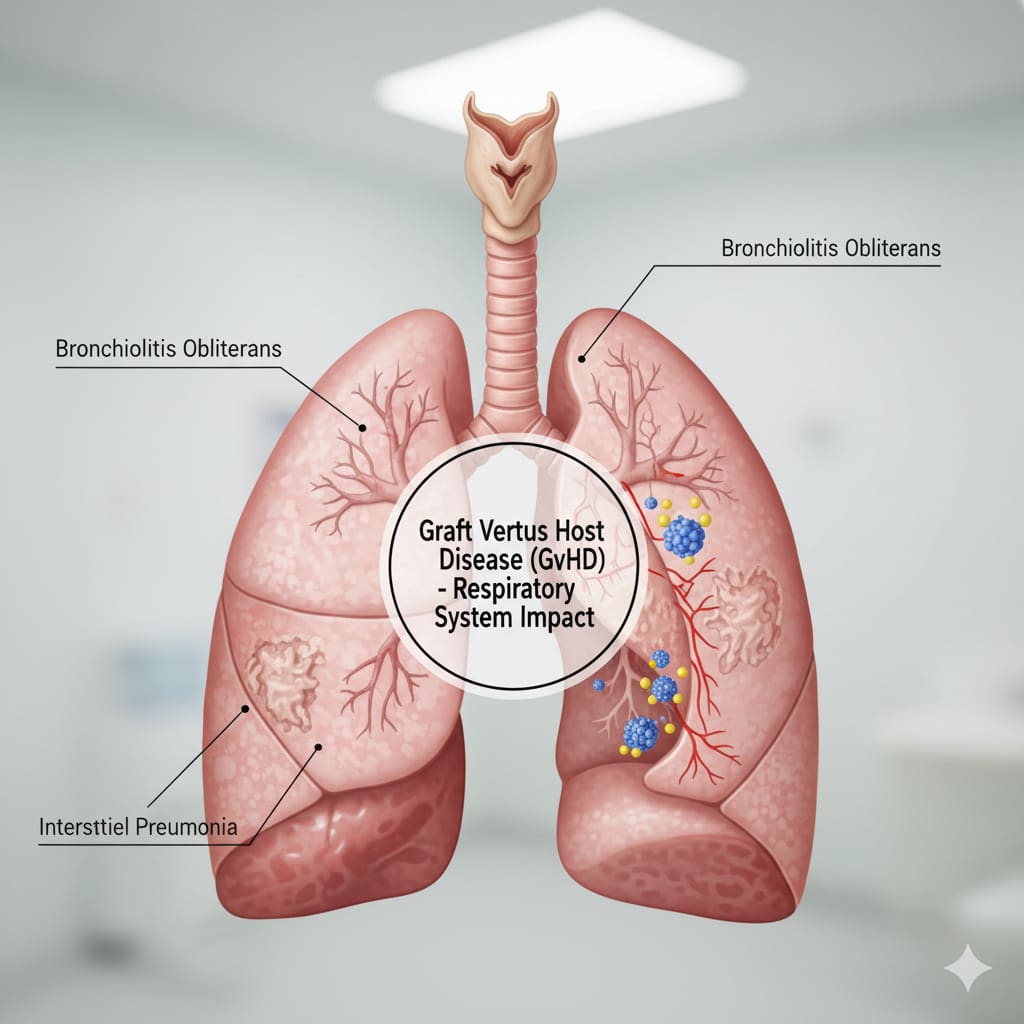
Lung GVHD is when the immune system attacks the lung tissue, causing inflammation and damage. This often shows up as bronchiolitis obliterans syndrome. This is when the small airways in the lungs get scarred and blocked, making it hard to breathe.
The way lung GVHD works is complex. It involves donor immune cells reacting with the recipient’s lung tissue. This can lead to more inflammation and damage in the lungs.
Lung GVHD is a big problem after allogeneic stem cell transplantation. Research shows that up to 9% of transplant patients might get lung GVHD.
There are several things that can increase the risk of lung GVHD. These include:
Knowing these risk factors helps doctors spot and treat lung GVHD early. By understanding GVHD in the lungs, doctors can find better ways to help transplant patients.
Pulmonary GVHD is a big worry after stem cell transplants, hitting up to 9% of patients. It can really change how well a patient does, so knowing the risks is key.
Research shows pulmonary GVHD can hit up to 9% of those getting stem cell transplants. This serious issue can lead to a lot of sickness and even death. So, finding it early and treating it well is very important.
“Pulmonary GVHD is a big problem after stem cell transplants,” say experts. “It can be very dangerous and even life-threatening.”
Some patients are more likely to get pulmonary GVHD. These include those who’ve had GVHD before, got transplants from mismatched donors, or have certain genes that make them more likely to get GVHD.
Spotting these high-risk patients early is vital. It helps in taking steps to prevent GVHD and closely watching them for any signs.
The main sign of lung trouble in graft vs host disease is bronchiolitis obliterans syndrome. This condition causes inflammation and scarring in the small airways. It makes breathing very hard.
We will look at how lung tissue changes and how it affects patients. Bronchiolitis obliterans syndrome is a serious issue. It can really hurt the quality of life for those with graft vs host disease lungs.
Bronchiolitis obliterans syndrome causes the small airways to close off. This happens because of inflammation and scarring. It damages the airway structure, causing breathing problems and symptoms.
The changes include:
These changes can be seen through tests and scans. These are key for diagnosing gvhd lung.
| Pathological Feature | Description | Impact on Lung Function |
|---|---|---|
| Inflammation | Inflammation of the bronchioles | Leads to airway obstruction |
| Fibrosis | Fibrosis and scarring within the airways | Causes irreversible damage |
| Obliteration | Obliteration of the bronchiolar lumen | Results in severe airflow limitation |
Bronchiolitis obliterans syndrome greatly affects breathing in patients with graft vs host disease lungs. They may have trouble breathing, cough, and wheeze. These symptoms can make it hard to move around and enjoy life.
We need to focus on diagnosing and treating lung injury in gvhd. Early action and the right treatment for bronchiolitis obliterans syndrome are key. They help improve outcomes for these patients.
Treatment for gvhd lung often includes medicines to reduce the immune system and care to manage symptoms. This helps slow down the disease.
GVHD in the lungs often goes unnoticed, making it hard to catch early. This is a big worry for those who have had a stem cell transplant. It can cause serious lung problems.
The first signs of lung GVHD can be vague or missing. This makes it tough for doctors to spot it early. Patients might not show typical lung symptoms like coughing or breathing trouble until it’s too late. This makes it hard to catch and treat GVHD lung disease early.
A top expert in hematology says, “Because early lung GVHD doesn’t have clear symptoms, doctors must watch patients closely and act fast.”
It’s hard to diagnose GVHD lung disease when it’s most treatable. The disease often progresses quietly before symptoms show up. By then, it might be too late.
Doctors use regular checks and tests to catch GVHD early. They do lung function tests and imaging to spot any lung changes. Finding GVHD lung disease early is key to better patient care.
“The best way to handle GVHD lung disease is to catch it early and act fast,” says a pulmonary medicine expert. “Finding it before it gets worse can greatly help patients.”
It’s important to know the difference between chronic and acute pulmonary GVHD. Each form needs a different treatment plan. This is key for managing the condition effectively.
Acute pulmonary GVHD usually starts within the first 100 days after a transplant. It comes on fast and can be very severe. Chronic GVHD, on the other hand, starts later, sometimes months or years after the transplant. It grows slower over time.
Timing of GVHD Forms
| GVHD Form | Typical Onset Time | Progression Rate |
|---|---|---|
| Acute GVHD | Within 100 days post-transplant | Rapid |
| Chronic GVHD | Months or years post-transplant | Slow |
Acute and chronic pulmonary GVHD show different symptoms. Acute GVHD has symptoms like fever and rash, along with breathing problems. Chronic GVHD mainly affects the lungs but can also affect other organs like the liver and skin.
Knowing the difference helps us treat lung problems in GVHD better. We need to understand how GVHD affects the lungs and how it changes over time. This way, we can give the right treatment to each patient.
Diagnosing lung GVHD needs a mix of tools. We’ve seen how lung GVHD can show up differently. So, getting it right is key to treating it well.
We’ll look at how to diagnose lung GVHD. This includes pulmonary function tests, imaging studies, and the importance of biopsy.
Pulmonary function tests (PFTs) are important for lung GVHD diagnosis. They check lung function like how much air you can breathe out and how well oxygen moves into your blood.
These tests help spot lung GVHD early. But, understanding the results needs to consider the patient’s history and other tests too.
| Pulmonary Function Test | Typical Findings in Lung GVHD |
|---|---|
| FEV1/FVC Ratio | Reduced, indicating obstructive lung disease |
| DLCO | Decreased, suggesting impaired gas exchange |
| FVC | Reduced, indicating restrictive lung disease |
Imaging like chest X-rays and HRCT scans help see lung damage. They look for signs that match GVHD.
HRCT scans can show signs like bronchiectasis and air trapping. But, biopsy is the best way to confirm lung GVHD. It shows the disease’s signs under a microscope.
But, biopsies carry risks. So, deciding to do one must balance its benefits and dangers for each patient.
The outlook for patients with lung GVHD is very important. It affects how doctors treat them and their overall well-being. Chronic GVHD is very serious, and lung problems make it even harder to manage.
How long patients with GVHD lung problems live varies a lot. This depends on how bad the lung problems are, if other parts of the body are affected, and how well they respond to treatment. Prognostic indicators like how well lungs work are key in predicting long-term results.
Patients with very bad lung function at the start usually do worse. Other health issues and overall health also play big roles in survival chances.
Lung GVHD greatly affects daily life and breathing. Symptoms like shortness of breath, cough, and tiredness make it hard to do everyday tasks. Respiratory capacity often drops, making it hard to do physical activities without getting tired.
It’s very important to manage these symptoms to improve life quality for those with GVHD lung problems. A good treatment plan includes exercises, managing symptoms, and medicines to help control the disease.
Knowing the prognosis and long-term effects helps doctors tailor treatments better. This can improve survival rates and quality of life for patients with GVHD lung disease.
In severe cases of GVHD, lung transplantation is considered a lifesaving option. This complex surgery is for those who have tried all other treatments and are facing serious lung problems.
Choosing the right patients for lung transplantation is a detailed process. It looks at their health, GVHD severity, and recovery chances. Key criteria include no active cancer, good heart function, and no major organ problems.
A leading transplant specialist notes,
“The decision to proceed with lung transplantation in GVHD patients requires a multidisciplinary approach, involving pulmonologists, transplant surgeons, and other specialists to ensure the best possible outcomes.”
Lung transplantation outcomes for GVHD patients vary. Some see big improvements in lung function and life quality. Others face issues like chronic rejection or GVHD in the new lung.
Careful patient selection and post-transplant management are key for success. As we learn more about GVHD, lung transplantation’s role will grow, giving hope to those with severe disease.
Lung transplantation is a major step for those with severe GVHD. As medical science improves, we’ll see better selection and outcomes for this complex surgery.
Managing pulmonary graft-versus-host disease (GVHD) needs a mix of treatments. We see that combining old and new treatments is key to better patient care.
Immunosuppressive treatments are the base for treating pulmonary GVHD. Corticosteroids are often the first choice to fight inflammation and calm the immune system. A study in the Journal of Clinical Oncology shows that corticosteroids are the first go-to for GVHD treatment.
Other treatments like calcineurin inhibitors and mTOR inhibitors can also help. The right treatment depends on how severe the GVHD is and the patient’s overall health.
New treatments for GVHD are being developed as we learn more about it. Biological agents that target GVHD’s causes are being tested in trials. These agents aim to lessen GVHD’s impact without harming the body’s ability to fight cancer.
“The emergence of new therapeutic strategies offers hope for improving outcomes in patients with pulmonary GVHD.” –
GVHD Researcher
Joining clinical trials is important for finding better treatments for pulmonary GVHD. These trials help find safer and more effective ways to treat this condition.
Treating pulmonary GVHD needs a team effort. Doctors from different fields work together to care for patients. This team approach makes sure all parts of the patient’s health are looked after.
By using a team approach to treat pulmonary GVHD, we can make patients’ lives better. This way, we can improve their quality of life and outcomes.
Understanding graft vs host disease lungs is complex. To improve care, we need a detailed approach. The outcome for patients depends on how severe the lung disease is and how well treatments work.
Spotting GVHD lung disease early and treating it with a team effort is key. We must focus on treatments like immunosuppressive drugs and new biological agents. These help meet the unique needs of these patients.
Healthcare providers must grasp the details of GVHD lung disease and its effects on patients. Keeping up with the latest research and treatments is vital. This way, we can improve care for those with this tough condition.
Looking ahead, we must explore new treatments and deepen our knowledge of GVHD lungs. This will help us give patients the best care possible.
Graft vs host disease (GVHD) lungs is a complication after stem cell transplant. The transplanted cells attack the lung tissue of the recipient. This leads to inflammation and damage.
Symptoms of GVHD lungs can be hard to spot early. They might include shortness of breath, cough, and wheezing.
Doctors use tests like pulmonary function tests and imaging studies to diagnose GVHD lungs. A biopsy is also used to check the lung damage and rule out other conditions.
Bronchiolitis obliterans syndrome is a condition that causes inflammation and scarring in the small airways. It can lead to breathing problems. It’s a common part of GVHD lungs.
Treatment for GVHD lungs includes immunosuppressive therapies and new biological agents. A team of doctors works together to manage the condition. In severe cases, lung transplantation might be considered.
The outlook for patients with GVHD lungs depends on the lung damage, how well they respond to treatment, and their overall health. Survival rates and quality of life can be greatly affected.
Preventing GVHD lungs is not guaranteed. But, careful patient selection and managing GVHD risk factors can lower the chance of getting this complication.
Risk factors for GVHD lungs include the type of stem cell transplant and how well the donor and recipient match. The presence of other GVHD symptoms also increases the risk. Some patients are at higher risk than others.
GVHD lungs can make everyday activities harder and reduce breathing capacity. This can lead to less exercise tolerance, fatigue, and a lower quality of life.
Lung transplantation is a last resort for severe GVHD lungs that haven’t responded to other treatments. Choosing the right patient is key for a successful transplant.
ASH Publications (Blood): Real-World Outcomes of Pulmonary Function Tests (PFTs) in Screening for Lung Complications
PubMed (NCBI): Bone Marrow Transplantation
NCBI Bookshelf (National Library of Medicine): Graft-Versus-Host Disease (StatPearls)
Radiopaedia: Graft-Versus-Host Disease: Pulmonary Manifestations
ASCO Publications (Journal of Clinical Oncology): Abstract on Post-Transplant Outcomes
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us