Last Updated on October 31, 2025 by
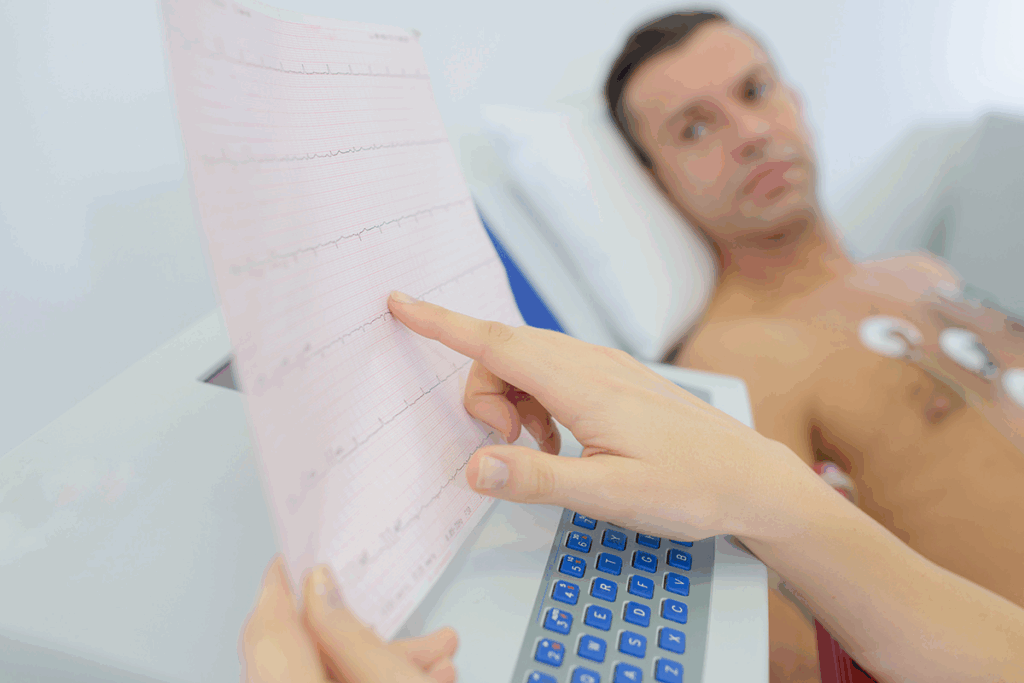
Diagnosing congestive heart failure needs a detailed physical assessment. At Liv Hospital, we stress the value of a complete physical exam. It helps spot patients with this complex condition.
A heart failure physical exam is key to finding the problems that mark this condition. We use the latest guidelines and top clinical skills. This makes sure every check-up is precise and focused on the patient.
Key Takeaways
- A thorough physical exam is essential for diagnosing congestive heart failure.
- Key physical findings play a critical role in identifying patients with heart failure.
- A complete physical assessment uses the latest guidelines and clinical excellence.
- Liv Hospital’s patient-centered approach ensures accurate and personalized care.
- Early diagnosis is critical in managing heart failure effectively.
The Fundamentals of Heart Failure Physical Examination

Understanding heart failure physical examination is key for correct diagnosis and care. We will look at the reasons behind physical signs and how to assess them. These are vital for checking patients with heart failure.
Pathophysiological Basis of Physical Findings
Heart failure (HF) has many causes, with heart disease being the main one. The exam checks fluid levels, blood pressure, and weight. Knowing why these signs happen helps doctors diagnose heart failure correctly.
Fluid overload causes signs like swollen neck veins, lung sounds, and leg swelling. These signs show how bad heart failure is and help doctors understand the patient’s condition.
Systematic Approach to Assessment
Doing a thorough physical exam is important. It starts with looking at the patient’s overall look for signs of trouble. Then, we focus on the heart, checking it in different ways.
Inspection looks for signs like neck vein swelling, leg swelling, and blue skin. Palpation checks the heart’s beat and feels for problems. Auscultation listens for heart sounds, like an extra sound in heart failure, and murmurs from valve problems.
By following a systematic exam, we get a full picture of the patient’s health. This helps doctors make the right diagnosis and treatment plan.
Jugular Venous Distention: Cardinal Sign of Volume Overload

Checking jugular venous distention is key to spotting volume overload in heart failure patients. Jugular venous distention (JVD) shows high pressure in the right atrium. It’s a big sign of heart failure.
Proper Technique for JVD Assessment
To get a good JVD check, the right method is important. The patient should sit at a 45-degree angle, with their head up a bit. We look at the jugular venous pulse and compare it to the sternal angle.
The space between the sternal angle and the jugular venous pulse is measured. If it’s over 3 cm, it’s too high.
Interpretation and Clinical Significance
JVD showing up means volume overload, a big sign of heart failure. It often goes with other signs like lung sounds and swelling in the legs. The more JVD, the worse the heart failure.
| JVD Measurement | Interpretation | Clinical Significance |
| < 3 cm | Normal | No sign of volume overload |
| 3-5 cm | Mild elevation | Mild volume overload, keep an eye on the patient |
| > 5 cm | Significant elevation | Big volume overload, shows heart failure |
Knowing what JVD means is key for diagnosing and treating heart failure. It helps doctors see how bad the volume overload is and if treatment is working.
Pulmonary Crackles (Rales): Detecting Pulmonary Edema
In heart failure patients, pulmonary crackles are a key sign. Clinicians must recognize and understand these sounds. They are a sign of possible pulmonary edema.
Distribution and Characteristics of Crackles
Pulmonary crackles are heard when listening to the lungs. They vary in timing, pitch, and location. Fine crackles are high-pitched and heard in late inspiration, often showing pulmonary fibrosis or edema. On the other hand, coarse crackles are louder and lower in pitch, heard throughout breathing, often linked to chronic bronchitis or pneumonia.
The location of crackles can hint at the underlying issue. For example, crackles at the lung bases, heard on both sides, might point to pulmonary edema. This is a common problem in heart failure.
Differentiation from Other Respiratory Findings
It’s important to tell pulmonary crackles from other lung sounds. Wheezes, for instance, are high-pitched and heard when exhaling. They are linked to airway blockage. Unlike crackles, wheezes sound musical and may go away with a cough.
- Pulmonary crackles are often more noticeable when the patient is lying down.
- Crackles linked to heart failure might get better or go away with heart treatment.
- Other symptoms, like trouble breathing when lying down or sudden shortness of breath at night, can help confirm heart failure.
By looking closely at the type and where crackles are heard, doctors can learn a lot. They can understand how severe pulmonary edema is in heart failure patients.
The Third Heart Sound (S3): Hallmark of Heart Failure Physical Exam
When we hear an S3 heart sound, it’s a big clue about heart problems. This sound is a low-frequency noise that happens early in the heartbeat. It’s a key sign we look for when checking for heart failure.
Auscultation Technique for S3 Detection
To find the S3 sound, we use a special listening method. We use the bell of the stethoscope, which catches low sounds better. The patient lies on their side to get the heart closer to the chest. We listen at the apex beat, making sure it’s quiet around us.
Key steps for S3 auscultation:
- Use the bell of the stethoscope.
- Position the patient in left lateral decubitus.
- Listen at the apex beat.
- Ensure a quiet environment.
Pathophysiological Significance
An S3 sound means the ventricle is full and under pressure during diastole. It’s often seen in heart failure, where the ventricle is too full. This sound happens when the ventricle fills up fast, making vibrations we can hear.
Understanding S3 is key for diagnosing and treating heart failure. It helps us see how bad the heart problem is and if treatments are working. The S3 sound is a big help in checking how well the heart is doing.
Displaced Apex Beat: Assessing Ventricular Enlargement
When checking a patient’s heart, finding a displaced apex beat is key. It shows if the left ventricle is too big or thick. This is common in heart failure.
Proper Palpation Technique
To check the apex beat right, you need the right touch. Here’s how to do it:
- Make sure the patient is comfy lying down or on their side.
- Feel the apex beat with the palm of your fingers. It’s at the fifth space, mid-clavicular line.
- Pay attention to where, how strong, and how long the beat is.
A displaced apex beat means the ventricle is too big. Getting it right means touching gently but firmly.
Correlation with Cardiac Remodeling
Heart failure makes the heart change shape and function. A displaced apex beat shows this change.
| Characteristic | Normal | Displaced Apex Beat |
| Location | Fifth intercostal space, mid-clavicular line | Lateral and/or inferior to usual location |
| Amplitude | Brisk, tapping | Forceful, sustained |
| Clinical Implication | Normal cardiac anatomy | Ventricular enlargement, cardiac remodeling |
A cardiology expert says, “Finding a displaced apex beat is a big deal. It means we need to check the heart’s function and if there’s heart failure.”
“The apex beat is a valuable indicator of cardiac health, and its displacement can signal significant pathology.”
Cardiology Expert
Knowing about displaced apex beats and how to feel them helps doctors. It helps them find and treat heart failure better.
Lower Extremity Edema: Quantification and Distribution
Checking for lower extremity edema is key in heart failure exams. It’s common in heart failure patients. A grading system helps measure its severity.
Grading System for Pitting Edema
Pitting edema is a sign of heart failure. Its severity can be graded. Here’s how:
| Grade | Description | Indentation Depth | Recovery Time |
| 1+ | Mild pitting edema | 2 mm | <10 seconds |
| 2+ | Moderate pitting edema | 4 mm | 10-15 seconds |
| 3+ | Severe pitting edema | 6 mm | >15 seconds |
| 4+ | Very severe pitting edema | 8 mm | >30 seconds |
This grading helps measure fluid overload in heart failure patients.
Bilateral vs. Unilateral Presentation
Edema can be on both legs or just one. Bilateral edema often means heart failure. Unilateral edema might point to a problem like a blood clot.
Bilateral Edema: Seen in heart failure, it shows fluid buildup all over.
Unilateral Edema: Could mean a problem like a blood clot or blocked lymphatic system.
Knowing how and how much edema is present is key to diagnosing and treating heart failure.
Vital Signs Abnormalities in Congestive Heart Failure
Vital sign changes are key in diagnosing congestive heart failure. These signs help us understand how severe the condition is. They also guide us in making treatment plans.
Tachycardia and Blood Pressure Changes
Tachycardia, or a fast heart rate, is common in heart failure patients. It helps the heart work harder when it’s not working well. Tachycardia can show that heart failure is getting worse or treatment isn’t working, so we need to change the treatment.
Blood pressure changes are also seen in heart failure. Hypotension happens when the heart can’t pump enough blood. Hypertension can make heart failure worse. It’s important to watch blood pressure closely to manage heart failure well.
Narrow Pulse Pressure Significance
Narrow pulse pressure is when the difference between the highest and lowest blood pressure is small. A narrow pulse pressure means the heart isn’t pumping enough blood, which is a sign of heart failure.
The importance of narrow pulse pressure is in its ability to predict outcomes. Research shows that a narrow pulse pressure is linked to bad outcomes in heart failure patients, including higher death rates. So, it’s vital to address narrow pulse pressure in managing heart failure.
In summary, vital sign changes like tachycardia, blood pressure issues, and narrow pulse pressure are important in diagnosing and treating congestive heart failure. By carefully looking at and understanding these signs, we can better treat patients and improve their health.
Hepatomegaly and Ascites: Abdominal Manifestations
In advanced heart failure, signs like hepatomegaly and ascites are key. They show right-sided heart failure. Doctors must spot these signs to help patients and predict their future.
Hepatojugular Reflux Assessment
Hepatojugular reflux is a sign linked to hepatomegaly and right ventricular issues. To check for it, press on the liver while the patient breathes normally. If the jugular veins get bigger, it’s a positive sign.
“The hepatojugular reflux test is a simple yet effective method for assessing right ventricular function and identifying heart failure,” say doctors.
Techniques for Detecting Ascites
Finding ascites needs a mix of physical checks and doctor’s judgment. The shifting dullness test is common. It involves checking for dullness changes when the patient moves.
- Perform the shifting dullness test to detect fluid.
- Use ultrasound if the diagnosis is uncertain.
- Assess for other signs of fluid overload.
Seeing ascites in heart failure patients means a worse outlook. So, finding and treating it early is vital.
Skin Changes and Peripheral Hypoperfusion
Skin changes are a key sign of heart failure, showing peripheral hypoperfusion. These signs help us understand how severe heart failure is and how well the body’s blood flow is working.
Cool, Clammy Extremities Assessment
One major sign of heart failure is cool, clammy hands and feet. This happens because less blood reaches the outer parts of the body. The skin feels cool and looks clammy because of more sweat.
To check for cool, clammy extremities, we should:
- Palpate the patient’s hands and feet to assess temperature
- Observe for visible signs of sweating
- Compare the temperature of the extremities to the core body temperature
Cyanosis and Delayed Capillary Refill
Cyanosis, or bluish skin, and slow capillary refill are also signs of poor blood flow. Cyanosis is most visible in lips, fingers, and toes.
| Sign | Description | Clinical Significance |
| Cyanosis | Bluish discoloration of skin and mucous membranes | Indicates poor oxygenation and perfusion |
| Delayed Capillary Refill | Prolonged time for capillaries to refill with blood after compression | Suggests decreased peripheral circulation |
To check for cyanosis and slow capillary refill, we look at the skin, mainly in the extremities. We also do a capillary refill test. These tests tell us a lot about the patient’s blood flow.
Diagnostic Criteria and Integration of Physical Findings
Diagnosing heart failure needs a detailed approach. We use guidelines to make sure we’re accurate.
Framingham Criteria for Heart Failure
The Framingham Heart Study criteria are key for diagnosing heart failure. They include both clinical and historical parts.
- Major criteria:
- Paroxysmal nocturnal dyspnea
- Neck vein distension
- Rales
- Cardiomegaly
- Acute pulmonary edema
- S3 gallop
- Increased venous pressure >16 cm H2O
- Circulation time ≥25 seconds
- Hepatojugular reflux
- Minor criteria:
- Ankle edema
- Night cough
- Dyspnea on exertion
- Hepatomegaly
- Pleural effusion
- Tachycardia (≥120 bpm)
- Weight loss ≥4.5 kg in 5 days
Diagnosis is confirmed with two major or one major and two minor criteria.
Boston Criteria for Heart Failure
The Boston criteria offer another way to diagnose heart failure. They focus on symptoms and clinical findings.
| Category | Points |
| Rest dyspnea | 4 |
| Orthopnea | 4 |
| Paroxysmal nocturnal dyspnea | 3 |
| Rales | 1-2 |
| Wheezing | 1 |
| Tachycardia ≥120 bpm | 1 |
| Edema | 1 |
A score of 8 or more means definite heart failure.
AAFP Guidelines for Heart Failure Diagnosis
The American Academy of Family Physicians (AAFP) suggests a detailed assessment. This includes history, physical exam, and tests.
Key components:
- Detailed medical history
- Physical examination findings
- Laboratory tests (e.g., BNP)
- Imaging studies (e.g., echocardiogram)
By following these guidelines and using physical findings, we can accurately diagnose and manage heart failure.
Conclusion: Optimizing Heart Failure Diagnosis Through Physical Examination
A detailed heart failure physical exam is key for accurate diagnosis and effective treatment. By combining physical findings with diagnostic criteria, we can make precise diagnoses. This leads to effective treatment plans.
Various physical signs are important in diagnosing heart failure. These include jugular venous distention, pulmonary crackles, and the third heart sound. Together, they give a full picture of the patient’s health. This helps doctors identify who needs more evaluation and treatment.
Highlighting the role of physical examination in diagnosing heart failure can improve patient care. A thorough physical exam allows doctors to create specific treatment plans. This results in better heart failure management. We must keep stressing the importance of physical exams in diagnosing and treating heart failure.
FAQ
What is the importance of a thorough heart failure physical exam in diagnosing congestive heart failure?
A detailed physical exam is key in spotting heart failure. It helps doctors find important signs and make a correct diagnosis.
What are the essential components of a heart failure physical examination?
The main parts include checking for jugular venous distention and pulmonary crackles. Also, looking for the third heart sound (S3), a displaced apex beat, and lower extremity edema. Doctors also check vital signs, abdominal signs, and skin changes.
How is jugular venous distention assessed, and what is its clinical significance?
Jugular venous distention is checked by looking at the jugular venous pressure. It’s a key sign of volume overload in heart failure, showing high right-sided pressures.
What is the significance of pulmonary crackles in detecting pulmonary edema?
Pulmonary crackles are important for spotting pulmonary edema in heart failure patients. Their pattern and sound help tell it apart from other lung issues.
How is the third heart sound (S3) detected, and what is its pathophysiological significance?
The third heart sound (S3) is found through proper listening. Its presence is a clear sign of heart failure, showing increased ventricular volume and pressure.
What is the significance of a displaced apex beat in heart failure patients?
A displaced apex beat means the ventricle is enlarged. It shows the heart has changed shape, which can mean severe heart failure.
How is lower extremity edema assessed, and what is its significance?
Lower extremity edema is graded for pitting. Its presence, more so if both legs are affected, suggests fluid overload and heart failure.
What vital sign abnormalities can occur in congestive heart failure?
In congestive heart failure, vital signs can change. This includes fast heart rate, blood pressure shifts, and narrow pulse pressure. These signs show how severe the heart failure is.
What are the diagnostic criteria for heart failure, and how are physical findings integrated into the diagnostic process?
Heart failure diagnosis uses the Framingham, Boston, and AAFP guidelines. These criteria look at physical signs to make a correct diagnosis and plan treatment.
What is the role of physical examination in optimizing heart failure diagnosis and management?
A detailed physical exam is vital for diagnosing and managing heart failure. It helps find key signs, guides tests, and shapes treatment plans.
How do the Framingham criteria, Boston criteria, and AAFP guidelines differ in diagnosing heart failure?
The Framingham, Boston, and AAFP guidelines have different criteria for diagnosing heart failure. Yet, they all stress the need for a full assessment to make an accurate diagnosis.
What is the significance of hepatomegaly and ascites in heart failure patients?
Hepatomegaly and ascites are signs of right-sided heart failure. They show fluid buildup and possible heart problems, guiding further care.
How are skin changes and peripheral hypoperfusion assessed in heart failure patients?
Skin changes and peripheral hypoperfusion are checked by looking at cool, clammy limbs, cyanosis, and slow capillary refill. These signs indicate heart issues and need further evaluation.
References
National Center for Biotechnology Information. (2025). Heart Failure Physical Exam 10 Key Physical Findings. Retrieved from