Last Updated on November 25, 2025 by Ugurkan Demir

Cardiomyopathy is a disease that weakens the heart muscle. It makes it harder for the heart to pump blood. This condition affects millions worldwide. The term “cardiomyopathy” literally means “disease of the heart muscle.” We will explore the essential facts about this condition and its diagnosis.
At Liv Hospital, we know how important it is to spot cardiomyopathy early. We use the latest diagnostic tools and focus on our patients. This helps them understand their condition and protect their heart health.
Key Takeaways
- Cardiomyopathy is a disease that affects the heart’s ability to pump blood.
- Understanding cardiomyopathy is key for early detection and treatment.
- Liv Hospital offers advanced diagnostic approaches for cardiomyopathy.
- Patient-centered care is our top priority in treating heart muscle conditions.
- Spotting the signs of cardiomyopathy can prevent serious complications.
What Is Cardiomyopathy? An Overview of Heart Muscle Disease
The term cardiomyopathy refers to a group of diseases that harm the heart muscle. This makes it hard for the heart to pump blood well. It’s a condition where the heart muscle doesn’t work right.
Medical Definition and Terminology
Medically, cardiomyopathy means diseases that hurt the heart muscle. This makes it hard for the heart to pump blood well. It can happen for many reasons, like genes, infections, or other health issues.
Doctors use special words to talk about different types of cardiomyopathy. These include dilated, hypertrophic, and restrictive cardiomyopathy. Each type has its own way of affecting the heart.
How Cardiomyopathy Affects Heart Function
Cardiomyopathy makes it hard for the heart to pump blood by changing the heart muscle. This can cause symptoms like shortness of breath, tiredness, and swelling in the legs.
The heart muscle can get thick, stretchy, or stiff in cardiomyopathy. This makes it hard for the heart to contract and pump blood. Sometimes, the heart wall can even get thinner, making it harder to pump blood.
It’s important to understand how cardiomyopathy affects the heart. This helps doctors find the best ways to treat and manage it.
Types of Heart Muscle Conditions and Their Characteristics

Heart muscle conditions, known as cardiomyopathy, come in different forms. Each has its own set of characteristics. Knowing these differences is key for the right diagnosis and treatment.
There are several types of cardiomyopathy, each affecting the heart in unique ways. The main types include dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy.
Dilated Cardiomyopathy
Dilated cardiomyopathy makes the left ventricle bigger and weaker. This reduces the heart’s ability to pump blood well. If not managed, it can lead to heart failure.
Some common features of dilated cardiomyopathy include:
- Enlargement of the heart chambers
- Reduced pumping efficiency
- Potential for arrhythmias
Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy makes the heart walls thicker, mainly the septum. This thickening can block blood flow and raise the risk of sudden cardiac death.
Key characteristics of hypertrophic cardiomyopathy include:
- Thickening of the heart muscle
- Potential obstruction of blood flow
- Increased risk of arrhythmias
Restrictive Cardiomyopathy
Restrictive cardiomyopathy stiffens the heart muscle. This makes it hard for the ventricles to fill with blood. It can lead to heart failure because the heart can’t relax and fill properly.
Some key features of restrictive cardiomyopathy include:
- Stiffening of the heart muscle
- Impaired filling of the ventricles
- Potential for heart failure
Essential Fact #1: The Spectrum of Heart Muscle Conditions
Cardiomyopathy is not just one condition. It’s a spectrum of heart muscle disorders that can vary a lot. These disorders affect how well the heart works. Knowing about this spectrum is key for diagnosing and treating it.
The severity of cardiomyopathy can differ a lot between people. Some might have mild symptoms that don’t affect their daily life much. Others might face severe problems that could be life-threatening.
Varying Degrees of Severity
The spectrum of heart muscle conditions includes many types of cardiomyopathy. Each type has its own level of severity. At one end, mild cardiomyopathy might not really affect heart function, and symptoms might not be obvious. At the other end, acute cardiomyopathy can be very serious and even fatal if not treated quickly.
It’s important to remember that cardiomyopathy can get worse over time. Regular check-ups are needed to manage it well. Catching it early and treating it right can really help people with cardiomyopathy.
Different Manifestations Across Age Groups
Cardiomyopathy can happen to people of all ages, from young kids to older adults. The way it shows up can change with age. For example, hypertrophic cardiomyopathy often causes sudden death in young athletes. Dilated cardiomyopathy is more common in older people.
It’s vital for doctors to understand these age-related differences. This helps them diagnose and treat cardiomyopathy better for people of all ages. We stress the need for care plans that fit each patient’s unique situation.
Essential Fact #2: Symptoms May Be Silent Until Advanced Stages
Cardiomyopathy often starts quietly, making it key to know its early signs. It affects the heart muscle, making it hard for the heart to pump blood. Many people with cardiomyopathy don’t notice symptoms until it’s too late.
Recognizing Subtle Warning Signs
In the early stages, cardiomyopathy might not show symptoms or they might be mild. But as it gets worse, signs become clearer. These can include:
- Shortness of breath during routine activities
- Fatigue or feeling weak
- Swelling in the legs, ankles, and feet
- Irregular heartbeats or palpitations
- Dizziness or lightheadedness
Knowing these symptoms and watching for changes in your health is important. Early detection can greatly help in managing and treating cardiomyopathy.
When to Seek Medical Attention
If you notice any of these symptoms, see a doctor right away. They can run tests to find out what’s wrong and create a treatment plan. Don’t delay in getting medical help if you notice unusual health changes.
| Symptom | Description | Action |
| Shortness of breath | Difficulty breathing during normal activities | Consult a doctor |
| Fatigue | Feeling weak or tired without reason | Discuss with a healthcare provider |
| Swelling | Swollen legs, ankles, or feet | Seek medical evaluation |
The American Heart Association says, “Cardiomyopathy can be silent until it’s advanced.” Taking care of your heart is important. If you’re worried about cardiomyopathy or have symptoms, don’t wait to see a doctor.
“The key to managing cardiomyopathy is early detection and appropriate treatment. Being aware of the subtle warning signs can make a significant difference in patient outcomes.”
Dr. John Smith, Cardiologist
Essential Fact #3: Genetic Factors Are Major Contributors
We now understand that genetic mutations play a big role in cardiomyopathy risk. This knowledge has greatly helped us diagnose and manage the condition.
Hereditary Forms of Cardiomyopathy
Cardiomyopathy can be passed down in families. It follows an autosomal dominant pattern, meaning just one mutated gene is needed. Genetic factors cause different types, like hypertrophic cardiomyopathy (HCM) and dilated cardiomyopathy (DCM).
In some families, cardiomyopathy shows up in many generations. This shows how important family history is in figuring out risk.
Genetic Testing and Family Screening
Genetic testing can spot specific mutations linked to cardiomyopathy. This lets us start early interventions and take preventive steps. Family screening is suggested when a genetic mutation is found in a family member.
Knowing the genetic roots of cardiomyopathy helps us give more precise diagnoses and treatment plans. It also helps us talk to families about their risks and the risks to their kids.
With better genetic testing, we can handle cardiomyopathy better. This leads to better results for those dealing with this condition.
Essential Fact #4: Diagnosing Cardiomyopathy Requires Multiple Approaches
To accurately diagnose cardiomyopathy, healthcare professionals use many tools. They combine imaging, blood tests, and other procedures. This helps them fully understand the heart’s structure and function.
Imaging Techniques for Heart Assessment
Imaging is key in diagnosing cardiomyopathy. Echocardiography is a common test. It checks the heart’s chambers, valves, and walls for any issues.
Cardiac MRI and CT scans are also used. They give more detailed views of the heart. These tests can spot scarring or other changes in the heart muscle.
Blood Tests and Biomarkers
Blood tests are vital in diagnosing cardiomyopathy. They look for biomarkers that show heart damage. For example, high levels of troponin or brain natriuretic peptide (BNP) can indicate heart injury.
Genetic testing is also recommended if there’s a family history. It can find specific mutations linked to cardiomyopathy. This helps assess the risk in family members.
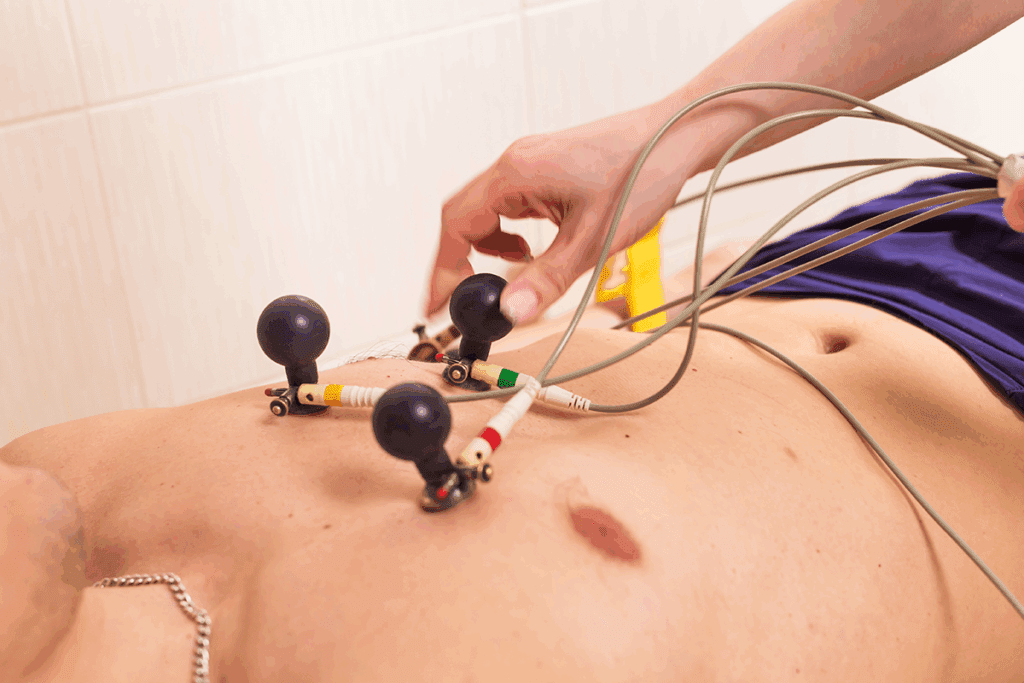
Other Diagnostic Procedures
Other tests are needed to diagnose and manage cardiomyopathy. Electrocardiography (ECG) checks for abnormal heart rhythms. It looks for any electrical issues.
A stress test is used to see how the heart works under stress. It can reveal problems that aren’t seen at rest.
In some cases, a heart biopsy is needed. It involves taking a small sample of heart tissue for examination. This helps doctors understand the heart muscle better.
Essential Fact #5: Blood Pressure Abnormalities Signal Complications
It’s key to understand how cardiomyopathy affects blood pressure. Cardiomyopathy makes the heart muscle sick. This can change blood pressure, showing signs of bigger problems.
“Managing blood pressure is vital for patients with cardiomyopathy,” says recent guidelines. Both high and low blood pressure can mean there’s something wrong that needs quick doctor’s care.
Cardiomyopathy Blood Pressure: High Readings
High blood pressure, or hypertension, often goes with cardiomyopathy. It makes the heart work harder, making the condition worse. We need to watch blood pressure closely. Unchecked high blood pressure can cause heart failure, arrhythmias, and other heart problems.
High blood pressure in cardiomyopathy comes from many things. These include vascular resistance, fluid buildup, and too much of certain hormones. To manage it, we use lifestyle changes and medicines.
Low Blood Pressure as a Warning Sign
Low blood pressure (hypotension) is also a worry in cardiomyopathy patients. It might mean the heart isn’t pumping well, dehydration, or other serious issues that need quick doctor’s help.
Low blood pressure can cause problems like dizziness, fainting, or tiredness. We must watch blood pressure closely and act fast if it changes a lot.
A recent study found, “Blood pressure changes are a big deal for heart failure and cardiomyopathy patients.” So, keeping blood pressure just right is key to better health.
Essential Fact #6: Acute Cardiomyopathy Can Develop Rapidly
We are learning more about how acute cardiomyopathy can strike suddenly. It impacts heart function dramatically. This condition requires immediate medical attention to prevent severe complications or even death.
Causes of Sudden Heart Muscle Deterioration
Several factors can contribute to the sudden deterioration of the heart muscle in acute cardiomyopathy. These include:
- Viral infections that directly affect the heart muscle
- Toxic reactions to certain medications or substances
- Autoimmune diseases where the body’s immune system attacks the heart
Understanding these causes is key for early diagnosis and treatment.
Emergency Signs and Interventions
Recognizing the emergency signs of acute cardiomyopathy is vital for timely intervention. Symptoms may include:
- Severe chest pain or discomfort
- Shortness of breath or difficulty breathing
- Rapid or irregular heartbeat
- Fainting or severe weakness
If you or someone else is experiencing these symptoms, it’s essential to seek immediate medical help.
In the emergency setting, healthcare providers may use various interventions to stabilize the patient. These can include:
- Administering medications to support heart function or control arrhythmias
- Using mechanical support devices like intra-aortic balloon pumps
- In some cases, heart transplantation may be considered for severe cases
| Emergency Signs | Potential Interventions |
| Severe chest pain | Medications for pain and to support heart function |
| Shortness of breath | Oxygen therapy, mechanical ventilation |
| Rapid or irregular heartbeat | Anti-arrhythmic medications, cardioversion |
| Fainting or severe weakness | Cardiac pacing, mechanical support devices |
By understanding the causes, recognizing emergency signs, and knowing the interventions, we can better manage acute cardiomyopathy. This improves patient outcomes.
Essential Fact #7: Treatment Options Continue to Evolve
Research keeps moving forward, and so do treatments for cardiomyopathy. Now, we have many ways to manage this condition. These include medicines and surgeries.
Medication Approaches
Medicines are key in treating cardiomyopathy. They help ease symptoms, slow the disease, and make life better. Some common medicines are:
- Beta-blockers to slow heart rate and boost heart function
- ACE inhibitors to lower blood pressure and ease heart strain
- Diuretics to get rid of extra body fluid
- Anti-arrhythmic drugs to control irregular heartbeats
Doctors might use these medicines alone or together, based on what each patient needs.
Surgical and Device-Based Interventions
There are also surgeries and devices to help with cardiomyopathy. Some options are:
| Procedure | Description | Benefits |
| Septal Myectomy | Surgical removal of extra heart muscle | Boosts heart function, lessens symptoms |
| Implantable Cardioverter-Defibrillator (ICD) | Device that watches and fixes irregular heartbeats | Prevents sudden cardiac death |
| Cardiac Resynchronization Therapy (CRT) | Device that syncs heart contractions | Improves heart function, reduces symptoms |
These treatments can greatly help patients with cardiomyopathy. By using medicines, lifestyle changes, and devices, we can offer full care for those with this condition.
Living with Heart Muscle Conditions: Management Strategies
Managing cardiomyopathy well needs a mix of lifestyle changes and regular doctor visits. It’s key to know the different ways to better your life and health when you have heart muscle issues.
Lifestyle Modifications
Making lifestyle changes is very important for managing cardiomyopathy. A balanced diet that’s low in salt and full of nutrients can help. It’s best to talk to a doctor or a nutritionist to make a meal plan that’s right for you.
Doing some exercise is good, but don’t overdo it. Regular, gentle exercises like walking or yoga can help your heart without harming it too much.
“Adopting a healthy lifestyle is not just about managing cardiomyopathy; it’s about improving your overall health.”
— Cardiomyopathy Association
Monitoring and Follow-up Care
It’s very important to keep an eye on your heart health. This means regular check-ups with your doctor to check how your heart is doing and change your treatment if needed.
Also, know the signs of serious problems, like trouble breathing or chest pain. If you notice these, get help right away.
Quality of Life Considerations
Keeping your quality of life good is a big part of managing cardiomyopathy. This means not just medical care, but also emotional support and making lifestyle changes that help you feel better overall.
- Stay close to family and friends
- Do things that make you happy and fulfilled
- Find ways to handle stress
By using these strategies, people with cardiomyopathy can live full and happy lives. We suggest working with your healthcare team to make a plan that’s just right for you.
Recent Advances in Cardiomyopathy Research and Treatment
The study of cardiomyopathy is moving fast, with new treatments coming up. We’re getting better at understanding and treating this heart condition. This means we can help people more effectively.
Emerging Therapies
New treatments are being developed for cardiomyopathy. These include:
- Gene Therapy: Scientists are looking into gene therapy to fix the genetic problems that cause cardiomyopathy.
- Stem Cell Therapy: They’re also studying stem cell therapy to fix damaged heart tissue.
- Targeted Pharmacological Treatments: New medicines are being made to target specific problems in cardiomyopathy. This means treatments can be more personalized.
These new treatments could greatly help people with cardiomyopathy. As research goes on, we’ll see even better treatments.
Promising Research Directions
There are also many promising areas of research in cardiomyopathy. These include:
- Advanced Imaging Techniques: New imaging tech is helping us diagnose and keep an eye on cardiomyopathy better.
- Genetic Research: Genetic studies are helping us understand the hereditary parts of cardiomyopathy. This helps us find people at risk.
- Personalized Medicine: Personalized medicine is leading to treatments that fit each patient’s needs better.
By exploring these areas, we’ll learn more about cardiomyopathy. This will lead to better care and outcomes for patients.
Conclusion: Taking Control of Your Heart Health
Understanding cardiomyopathy is key to managing heart health. Knowing about heart muscle conditions helps people take action. They can keep their heart healthy and deal with issues like cardiomy and thickening around the heart.
We’ve looked at the different types of cardiomyopathy and why early detection is vital. Spotting symptoms and knowing about genetic factors helps people get medical help when needed.
Managing cardiomyopathy well means making lifestyle changes and following up with doctors. Working with healthcare experts helps create a plan for heart health. This plan can handle any heart problems that come up.
Heart health control needs a full approach, and knowing about cardiomyopathy is a big part of it. By staying informed and active, people can lower heart risks. This keeps them healthy overall.
FAQ
What is cardiomyopathy?
Cardiomyopathy is a disease that affects the heart muscle. It makes the heart less able to pump blood. This includes different conditions that harm the heart’s function.
What are the different types of cardiomyopathy?
There are three main types: dilated, hypertrophic, and restrictive cardiomyopathy. Each has its own symptoms and characteristics.
What is the medical term for hardening of the heart muscle?
Hardening of the heart muscle is linked to conditions like myocardial fibrosis or cardiac sclerosis. These are part of cardiomyopathy.
Can cardiomyopathy be genetic?
Yes, some cardiomyopathy types are inherited. Genetic tests and family screenings help find those at risk.
How is cardiomyopathy diagnosed?
Doctors use many methods to diagnose cardiomyopathy. These include echocardiography, blood tests, and other tests.
What are the symptoms of cardiomyopathy?
Early symptoms of cardiomyopathy can be mild. Look out for signs like shortness of breath, fatigue, or swelling. Seeing a doctor early is key.
How does cardiomyopathy affect blood pressure?
Cardiomyopathy can cause high or low blood pressure. These changes can signal serious issues.
What is acute cardiomyopathy?
Acute cardiomyopathy is a sudden and severe heart muscle problem. It needs quick medical help.
How is cardiomyopathy treated?
Treatment for cardiomyopathy includes medicines, surgery, and devices. Medical research keeps improving these options.
Can lifestyle modifications help manage cardiomyopathy?
Yes, making lifestyle changes is important. They help manage the condition and improve quality of life.
What is thinning of the heart wall?
Thinning of the heart wall makes the heart muscle weaker. It can lead to poor heart function and is linked to some cardiomyopathy types.
What is the impact of cardiomyopathy on heart function?
Cardiomyopathy weakens the heart’s pumping ability. This can cause heart failure and other serious problems.
References
- Mwalimu, J., & Cooper, A. (2024). Multiple variations in abdominal aorta branching with special reference to the presence of accessory renal arteries from an East African female cadaver. Surgical and Radiologic Anatomy, 46(8), 929-934. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11441833/