The liver and bile ducts play a key role in digestion and health. Yet, hepatobiliary diseases are on the rise worldwide.
Metabolic Associated Steatotic Liver Disease (MASLD) is now a major global health issue. It affects about 38% of adults globally. This rise is linked to more obesity and diabetes.
MASLD is changing how we view liver health and care today. It’s important to understand MASLD to tackle its global health effects.
Key Takeaways
- MASLD is the most common hepatobiliary disease globally.
- Approximately 38% of adults worldwide are affected by MASLD.
- Rising obesity and diabetes rates are driving the prevalence of MASLD.
- MASLD significantly impacts liver health and patient care.
- Understanding MASLD is key to addressing its global health implications.
Understanding the Hepatobiliary System
The hepatobiliary system is a network of organs and ducts that keeps us healthy. It’s key for digestion, metabolism, and getting rid of toxins.
Anatomy of the Liver, Gallbladder, and Bile Ducts
The system includes the liver, gallbladder, and bile ducts. The liver, our biggest organ, cleans toxins and makes proteins. It also helps with digestion.
The gallbladder holds bile, which helps break down fats. The bile ducts carry bile from the liver to the gallbladder and then to the small intestine.
Physiological Functions of the Hepatobiliary System
The system does many important jobs. The liver breaks down nutrients and detoxifies harmful stuff. It also makes bile.
The gallbladder makes bile more concentrated. Then, the bile ducts send it to the small intestine. There, it helps digest fats and absorb vitamins.
|
Organ |
Primary Functions |
|---|---|
|
Liver |
Detoxification, metabolism, production of bile and proteins |
|
Gallbladder |
Storage and concentration of bile |
|
Bile Ducts |
Transportation of bile to the small intestine |
Importance in Overall Health
The hepatobiliary system is essential for our health. Problems here can cause jaundice, cirrhosis, and gallstones. Keeping it healthy is key to avoiding diseases.
By eating right, not drinking too much alcohol, and managing health issues, we can keep our system working well. This is vital for our health and happiness.
Overview of Hepatobiliary Diseases

Hepatobiliary diseases affect the liver, gallbladder, and bile ducts. They can greatly reduce a person’s quality of life. These diseases also put a big strain on healthcare systems around the world.
Classification of Hepatobiliary Disorders
Hepatobiliary disorders fall into several categories. They are based on their cause and the part of the system they impact. The main categories include:
- Metabolic Disorders: Like Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), linked to metabolic syndrome.
- Infectious Diseases: Viral hepatitis (B and C) that harm the liver.
- Autoimmune Diseases: When the body’s immune system attacks the liver or bile ducts.
- Cancer: Types like hepatocellular carcinoma and cholangiocarcinoma affect the system.
Knowing these categories is key for diagnosing and treating these diseases.
Common Symptoms of Hepatobiliary Dysfunction
The symptoms of hepatobiliary diseases vary by condition. Common signs include:
- Jaundice, which makes the skin and eyes turn yellow.
- Abdominal pain, often in the right upper area.
- Fatigue and feeling generally unwell.
- Changes in urine and stool color.
Spotting these symptoms early is critical for quick action.
Global Impact on Healthcare Systems
Hepatobiliary diseases significantly affect healthcare systems worldwide. The rise in conditions like MASLD is linked to obesity and metabolic syndrome. This affects how healthcare resources are used and the need for better prevention and treatment.
As the global burden of these diseases grows, it’s vital to raise awareness. We must also improve diagnosis and develop effective treatments.
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): The Most Common Hepatobiliary Disease
It’s important to know about MASLD. It’s a type of liver disease linked to metabolic problems. This condition is getting more common and can lead to serious liver damage.
From NAFLD to MASLD: Understanding the Terminology Change
The term NAFLD (Non-Alcoholic Fatty Liver Disease) has changed to MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease). This change shows a deeper understanding of the disease. It highlights how metabolic issues and liver problems are connected, beyond just not drinking alcohol.
The new name focuses on metabolic problems in causing the disease. It gives a clearer picture of the condition. It looks at the metabolic issues, not just the lack of alcohol.
Definition and Characteristics
MASLD is marked by too much fat in liver cells, often tied to metabolic syndrome. It includes different levels of liver damage, from simple fat buildup to non-alcoholic steatohepatitis (NASH), which adds inflammation and scarring.
The main traits of MASLD are:
- Too much fat in liver cells
- Linked to metabolic syndrome, like obesity and insulin resistance
- Can cause various liver problems, from simple fat buildup to NASH and cirrhosis
Spectrum of Disease: From Simple Steatosis to NASH
MASLD’s range goes from simple steatosis, where there’s fat buildup without inflammation, to NASH. NASH has fat buildup, inflammation, and damage to liver cells. It can lead to scarring, cirrhosis, and even liver cancer in severe cases.
It’s key for doctors to understand this range to treat MASLD well. Catching it early and treating it can stop it from getting worse. This shows why it’s vital to screen and treat those at risk.
Epidemiology of MASLD
Understanding MASLD’s spread is key to seeing its global health impact. Metabolic Dysfunction-Associated Steatotic Liver Disease, or MASLD, is a growing worry worldwide.
Global Prevalence Statistics
MASLD hits a big chunk of the world’s adults. Studies show it affects about 38% of adults globally. This makes it a top liver disease globally. The numbers vary by region and population, based on diet, lifestyle, and genes.
United States Prevalence and Projections
In the US, MASLD is a big deal, affecting over 14.9 million people. Experts think this number will jump to 23.2 million by 2050. This growth is due to more obesity, diabetes, and metabolic issues, which raise MASLD risk.
|
Year |
Prevalence of MASLD in the US (in millions) |
|---|---|
|
Current |
14.9 |
|
2050 (Projected) |
23.2 |
Demographic Patterns and High-Risk Populations
Some groups face a higher risk of MASLD. These include people with obesity, type 2 diabetes, and those who don’t move much. Genes also play a part, with some ethnic groups more likely to get MASLD.
Knowing who’s at risk helps us aim our prevention and treatment better. By focusing on lifestyle changes and early action, we can fight MASLD’s rise.
Risk Factors Contributing to MASLD Development
MASLD develops from many factors, including metabolic, genetic, and environmental ones. Knowing these risk factors helps us spot who’s at high risk. It also guides us in taking steps to prevent it.
Obesity and Metabolic Syndrome
Being obese, mainly around the middle, is a big risk for MASLD. Obesity links to MASLD through insulin resistance and more. It also leads to inflammation in fat tissue.
Metabolic syndrome adds to this risk. It includes high blood pressure, high blood sugar, and too much belly fat. It also affects cholesterol and triglyceride levels.
Key components of metabolic syndrome that contribute to MASLD include:
- Insulin resistance
- Dyslipidemia
- Hypertension
- Pro-inflammatory state
Type 2 Diabetes and Insulin Resistance
Type 2 diabetes is a big risk for MASLD, with insulin resistance at the heart of it. Insulin resistance makes the liver store more fat. It does this by letting more fatty acids into the liver and making more fat from scratch.
Insulin resistance means the body can’t take up glucose well. This leads to high blood sugar and insulin levels. This mess ups the liver, making it fatter, more inflamed, and scarred.
Genetic Predisposition and Environmental Factors
Genetics also play a big part in MASLD. Certain genes linked to fat, insulin, and inflammation increase the risk. Environmental factors like diet, exercise, and toxins can change this risk too.
A mix of genetic and environmental factors can cause MASLD. For example, eating too much saturated fat and simple carbs worsens insulin resistance. It also makes the liver fatter.
Pathophysiology of MASLD
Understanding MASLD means looking into its complex processes. It involves many metabolic and cellular steps. The disease’s development is a mix of several factors that harm the liver.
The “Multiple Hit” Hypothesis
The “multiple hit” hypothesis is key to understanding MASLD. It says the disease comes from many insults. These include insulin resistance and oxidative stress, which together damage the liver.
These “hits” are like a series of events that make the liver more prone to damage. For example, insulin resistance helps fat build up in the liver, a key sign of MASLD.
Cellular Mechanisms of Liver Fat Accumulation
Liver fat buildup in MASLD happens because of an imbalance. This imbalance is caused by more fatty acids coming in, more fat being made, and less fat being burned.
The cells in the liver, like hepatocytes and Kupffer cells, play a big role. They interact in ways that release harmful substances and start fibrosis.
Progression from Steatosis to Fibrosis
The move from simple fat buildup to NASH and then to fibrosis is a big part of MASLD. This move is caused by ongoing damage and inflammation. It leads to scarring and the buildup of matrix proteins in the liver.
Knowing how this move happens is key to finding ways to stop or reverse MASLD’s progress.
Clinical Presentation and Symptoms of MASLD
MASLD can be hard to spot early on. Many people don’t show symptoms until it’s too late. This makes it tough to catch MASLD before it causes serious liver damage.
Asymptomatic Presentation in Early Stages
In the beginning, MASLD doesn’t show up much. People might not feel any pain or discomfort. Getting regular health checks and screenings is key to finding MASLD early.
Signs and Symptoms as Disease Progresses
As MASLD gets worse, symptoms start to show up. These can include:
- Fatigue
- Abdominal discomfort or pain, mainly in the right upper quadrant
- General malaise
When MASLD gets really bad, symptoms get worse. You might see jaundice, itching, and swelling in your legs and belly.
Quality of Life Impact
MASLD can really hurt your quality of life. Chronic fatigue and discomfort can mess up your daily life and mood. Also, dealing with a chronic liver disease can lead to anxiety and depression.
It’s important for doctors to know about MASLD’s symptoms. Catching it early can make a big difference in how well a patient lives with the disease.
Diagnostic Approaches for Hepatobiliary Diseases
Diagnosing hepatobiliary diseases, like Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), requires several steps. These include lab tests, imaging studies, and sometimes a liver biopsy. Getting the diagnosis right is key to managing these conditions well.
Laboratory Tests and Biomarkers
Laboratory tests are essential in diagnosing these diseases. Tests like liver function tests (LFTs) show if the liver is damaged. Other tests, like gamma-glutamyl transferase (GGT) and alkaline phosphatase (ALP), help spot cholestatic disorders.
Biomarkers like the Fibrosis-4 (FIB-4) index and the NAFLD Fibrosis Score (NFS) check fibrosis levels in MASLD patients. These tests are non-invasive and help decide if further evaluation or treatment is needed.
|
Laboratory Test |
Significance |
|---|---|
|
ALT, AST |
Indicate liver damage |
|
GGT, ALP |
Elevated in cholestatic disorders |
|
FIB-4, NFS |
Assess degree of fibrosis |
Imaging Techniques
Imaging is vital for diagnosing these diseases. Ultrasound is often the first choice because it’s non-invasive and can spot steatosis and gallstones. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) offer more detailed views of the liver. They help identify issues like cirrhosis or liver masses.
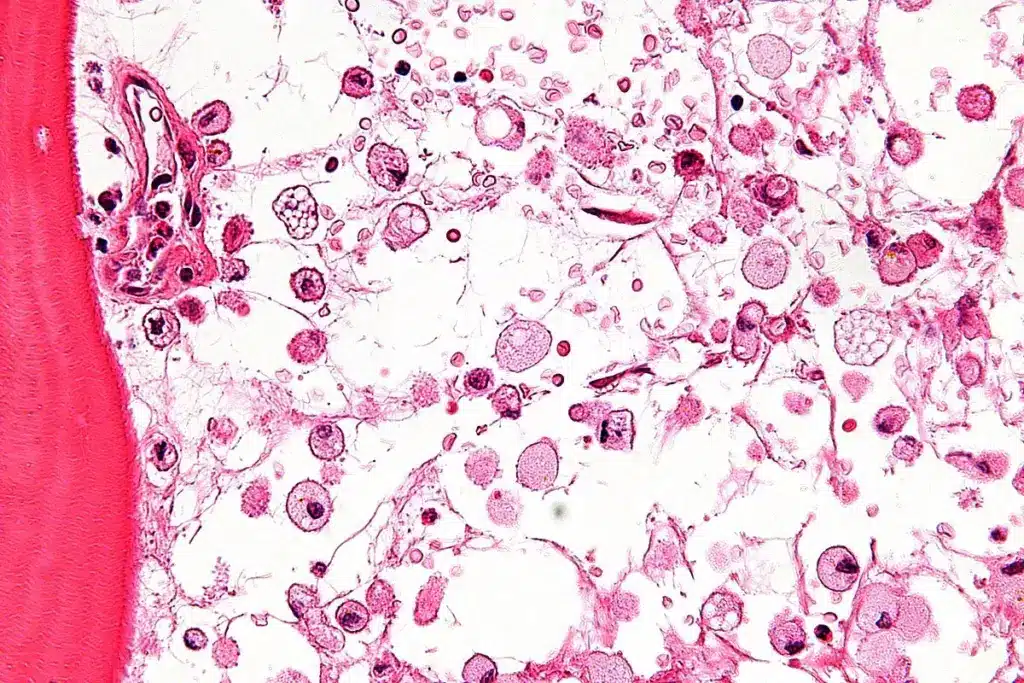
Liver Biopsy and Histological Assessment
Liver biopsy is the most accurate way to diagnose MASLD and assess inflammation and fibrosis levels. It can tell the difference between simple steatosis and steatohepatitis (NASH). This information is vital for planning treatment and predicting outcomes.
Non-invasive Fibrosis Assessment Tools
Tools like transient elastography (FibroScan) are becoming popular alternatives to liver biopsy. They measure liver stiffness, which shows the level of fibrosis. These tools are useful for tracking disease progression and treatment success.
Treatment Strategies for MASLD
Managing Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) mainly involves lifestyle changes and, if needed, medicines. Treatment plans are made to fit each person’s disease stage and health.
Lifestyle Modifications as First-Line Treatment
Lifestyle changes are key in treating MASLD. These include:
- Weight Loss: Losing 5-10% of body weight can greatly reduce liver fat and inflammation.
- Dietary Changes: Eating a healthy diet low in fats, sugars, and refined carbs is important.
- Increased Physical Activity: Regular exercise boosts insulin sensitivity and lowers liver fat.
These lifestyle changes not only help the liver but also improve overall health.
Pharmacological Interventions
For those who don’t respond to lifestyle changes or have severe disease, medicines might be used. Current options include:
- Insulin Sensitizers: Medications like metformin help improve insulin resistance.
- Lipid-Lowering Drugs: Statins and fibrates manage dyslipidemia.
- Antioxidants: Vitamin E can improve liver health in some patients.
These medicines are chosen carefully based on the patient’s condition and other health issues.
Emerging Therapies in Clinical Trials
New treatments for MASLD are being researched. Emerging options include:
- FXR Agonists: These drugs improve bile acid metabolism and show promise in reducing liver fat.
- Anti-Fibrotic Agents: Therapies aimed at preventing or reversing fibrosis are being studied.
Patients with advanced MASLD might consider joining clinical trials.
Management of Advanced Disease and Complications
When MASLD has progressed to cirrhosis or complications, management focuses on:
- Surveillance for Hepatocellular Carcinoma: Regular monitoring is key for early detection.
- Management of Portal Hypertension: Medications or procedures may be used to reduce pressure.
- Liver Transplantation: In severe liver disease, liver transplant may be an option.
Complications and Long-term Outcomes of Untreated MASLD
MASLD, if not treated, can harm the liver a lot. It can lead to serious problems and affect a person’s life quality a lot.
Progression to Cirrhosis
Untreated MASLD can turn into cirrhosis. Cirrhosis means the liver gets scarred and works poorly. This damage can take years to happen.
Things like inflammation, oxidative stress, and insulin resistance can make MASLD worse. Knowing these can help find who’s at risk and how to help them.
Hepatocellular Carcinoma Risk
People with untreated MASLD are more likely to get hepatocellular carcinoma (HCC), a liver cancer. The constant inflammation and damage to liver cells help cancer grow.
It’s important to watch closely for HCC in those at high risk, like those with advanced fibrosis or cirrhosis.
Liver Transplantation Considerations
In severe cases of MASLD, like when cirrhosis or HCC happens, liver transplantation might be needed. This big surgery replaces the sick liver with a healthy one from a donor.
Extrahepatic Manifestations and Comorbidities
MASLD also causes problems outside the liver. These include heart disease, type 2 diabetes, and metabolic syndrome. These add to the sickness and death risk from MASLD.
It’s key to manage these other health issues to improve life for those with MASLD.
Other Common Hepatobiliary Diseases in Comparison
Hepatobiliary diseases include many conditions that affect the liver and biliary system. It’s important to know about these diseases for accurate diagnosis and treatment.
Viral Hepatitis (B and C)
Viral hepatitis is a big health problem worldwide. It’s caused by hepatitis B and C viruses. These viruses can cause liver infections that may lead to cirrhosis and cancer.
Key differences between MASLD and viral hepatitis:
- Cause: MASLD is linked to metabolic issues, while viral hepatitis comes from viruses.
- Transmission: Viral hepatitis spreads through bodily fluids and blood. MASLD is related to lifestyle and metabolic factors.
- Treatment: For viral hepatitis, antiviral drugs are used. For MASLD, lifestyle changes and new treatments are considered.
Alcoholic Liver Disease
Alcoholic liver disease (ALD) is liver damage from too much alcohol. It can range from simple liver fat buildup to severe liver damage.
Similarities and differences between MASLD and ALD:
|
Disease Characteristics |
MASLD |
ALD |
|---|---|---|
|
Cause |
Metabolic dysfunction |
Excessive alcohol consumption |
|
Liver Damage |
Steatosis, inflammation, fibrosis |
Steatosis, inflammation, fibrosis, cirrhosis |
|
Treatment Approach |
Lifestyle modifications, emerging therapies |
Alcohol cessation, supportive care |
Gallstone Disease and Cholecystitis
Gallstone disease is when stones form in the gallbladder. It can cause cholecystitis, an inflammation of the gallbladder. It’s not a liver disease but affects the biliary system.
“Gallstones are a common condition, and their prevalence is increasing in parallel with the rising incidence of metabolic syndrome and obesity.”
Primary Biliary Cholangitis and Primary Sclerosing Cholangitis
Primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) are autoimmune diseases of the bile ducts. PBC destroys the bile ducts inside the liver. PSC affects both inside and outside bile ducts, causing scarring and narrowing.
Key features of PBC and PSC:
- PBC: It’s more common in women and is linked to antimitochondrial antibodies.
- PSC: It’s more common in men and often linked to inflammatory bowel disease.
In conclusion, while MASLD is a common disease, it’s important to understand other conditions like viral hepatitis, alcoholic liver disease, gallstone disease, and autoimmune cholangitis. This knowledge is key for effective patient care.
Prevention Strategies and Public Health Approaches
MASLD prevention needs a wide approach. It includes lifestyle changes, early detection, and community programs. These steps help lower MASLD cases and their effects.
Lifestyle Interventions for High-Risk Populations
Lifestyle changes are key for stopping MASLD, mainly in those at high risk. Weight management is a big part of it. Eating less fat, sugar, and carbs helps. Exercise also helps manage weight and improves insulin use, lowering MASLD risk.
Targeted interventions are vital for groups at high risk, like the obese or those with diabetes. These might include diet advice, exercise tips, and lifestyle counseling.
Screening Recommendations
Finding MASLD early is key to stopping it from getting worse. Screening recommendations focus on those at risk, like the obese or those with diabetes. Doctors use tests like liver enzyme checks and ultrasound to spot liver fat and fibrosis risk.
Guidelines say people at risk should get screened for liver disease often. How often depends on their risk and the doctor’s advice.
Public Health Campaigns and Education
Public health campaigns are important for spreading the word about MASLD. Educational initiatives teach about the need for a healthy weight, exercise, and balanced diet.
Community programs that push for healthy living are also key. They can be in schools, workplaces, or community centers. This way, many people can learn about health and wellness.
Conclusion: The Growing Challenge of MASLD in Modern Healthcare
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) is a big problem in today’s healthcare. It’s linked to obesity, metabolic syndrome, and insulin resistance. This makes it a major public health issue.
The number of people with MASLD is growing fast. This will put a lot of pressure on healthcare systems. We need good ways to manage it, like changing our lifestyle and new treatments.
Knowing the risks, like genetics and environment, helps us find better ways to fight MASLD. For example, liver and bile duct cancer can happen because of MASLD. You can learn more about this on theSEER website.
To tackle the MASLD challenge, we must raise awareness, prevent it, and catch it early. This will help lessen its impact on healthcare today.
FAQ
What is MASLD, and how does it differ from NAFLD?
MASLD, or Metabolic Dysfunction-Associated Steatotic Liver Disease, is a condition where fat builds up in the liver. It used to be called NAFLD, or Non-Alcoholic Fatty Liver Disease. The name change to MASLD highlights its link to metabolic issues.
What are the risk factors for developing MASLD?
Risk factors for MASLD include obesity, metabolic syndrome, type 2 diabetes, and insulin resistance. Genetics and environment also play a part.
What are the symptoms of MASLD, and how does it progress?
Early MASLD often has no symptoms. Later, symptoms like fatigue, abdominal pain, and jaundice may appear. If not treated, it can lead to cirrhosis and liver cancer.
How is MASLD diagnosed?
Diagnosing MASLD involves tests and imaging. Tests check liver function and biomarkers. Imaging like ultrasound and MRI look at liver fat and fibrosis.
What are the treatment options for MASLD?
Treatment starts with lifestyle changes like losing weight and exercising. Medicines and new treatments are being researched. In severe cases, a liver transplant might be needed.
Can MASLD be prevented?
Yes, preventing MASLD is possible with healthy lifestyle choices. Eating well and exercising regularly can help. Early detection through screenings is also key.
How does MASLD compare to other hepatobiliary diseases?
MASLD is among several liver diseases, like viral hepatitis and alcoholic liver disease. Each has its own cause and symptoms.
What is the global impact of MASLD?
MASLD affects millions worldwide and is growing due to obesity and metabolic syndrome.
What are the possible complications of untreated MASLD?
Untreated MASLD can cause cirrhosis, liver cancer, and liver failure. It may need a liver transplant. It also increases the risk of heart disease.
How can healthcare systems address the growing challenge of MASLD?
Healthcare can fight MASLD by raising awareness and promoting prevention. This includes public health campaigns and effective treatments.
What is the role of the hepatobiliary system in overall health?
The liver, gallbladder, and bile ducts are vital for digestion, metabolism, and detox. Problems here can lead to diseases like MASLD.
What are the current research directions for MASLD?
Research focuses on new treatments, therapies, and understanding MASLD’s causes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11374351/[1





