Hepatobiliary surgery, including liver and biliary resections, comes with big risks. These complex surgeries can cause many problems after the operation.
Studies show that up to 28.4% of patients face complications. Serious issues happen in 18.6% of cases. Also, 2.7% of patients die during or right after surgery. It’s important for doctors and patients to know these risks to get the best results.
Key Takeaways
- Hepatobiliary surgery carries significant risks, including high morbidity rates.
- Serious complications can occur in a substantial percentage of cases.
- Peri-operative mortality is a notable concern.
- Understanding these risks is essential for improving patient outcomes.
- Continuous quality improvement is necessary to mitigate these risks.
Understanding Hepatobiliary Surgery

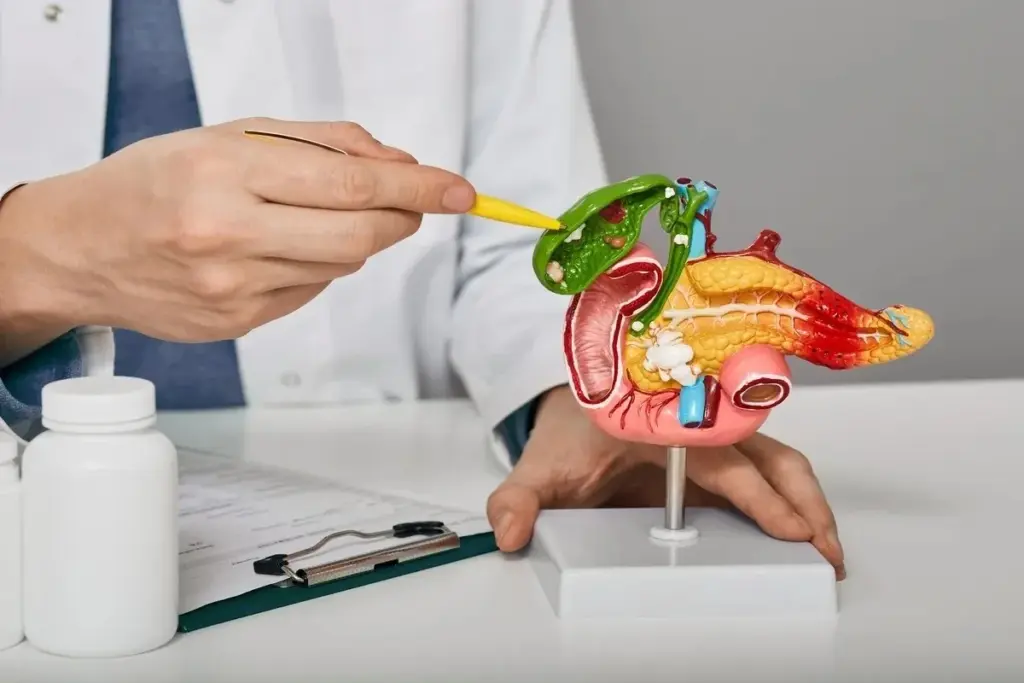
Hepatobiliary surgery deals with treating liver and bile duct problems. These surgeries are very complex and need a lot of skill.
Definition and Scope
Hepatobiliary surgery involves the liver, bile ducts, and gallbladder. It includes many procedures like liver removals and fixing bile ducts. It also covers removing the gallbladder.
At Liv Hospital, our mission is to compete internationally with excellent outcomes by following current academic protocols. This ensures patients get the best treatments.
Common Hepatobiliary Procedures
Some common surgeries include:
- Liver resections for cancer or damaged liver tissue
- Bile duct surgery for strictures, cancer, or other obstructions
- Gallbladder surgery, typically for gallstones or cancer
A renowned expert said,
“The complexity of hepatobiliary surgery necessitates a multidisciplinary approach to patient care, ensuring optimal outcomes.”
Knowing about these surgeries helps us understand the risks and the need for skilled doctors.
Epidemiology of Hepatobiliary Surgical Complications
It’s key to know about the risks of hepatobiliary surgery to better care for patients. These surgeries are lifesaving but come with big risks and complications.
Research shows that up to 28.4% of patients face complications after these surgeries. These issues can really affect a patient’s life and add to healthcare costs.
Overall Morbidity Rates
The 28.4% morbidity rate shows how complex and risky these surgeries are. This rate includes everything from minor problems to serious ones that need big interventions.
Serious Complications
About 18.6% of patients face serious complications that need treatment or cause big problems. These can be bile leaks, blood clots, or bleeding after surgery. Handling these issues often takes a team effort, including radiologists and surgeons.
Perioperative Mortality
Even though it’s rare, 2.7% of patients die soon after surgery. This low rate shows how important it is to pick the right patients, prepare them well, and give top-notch care during surgery.
Studying these complications helps us improve care and save lives. By understanding the risks, doctors and nurses can work to lower the number of problems and deaths.
Important facts about complications from hepatobiliary surgery include:
- Overall morbidity rate: 28.4%
- Serious complications: 18.6%
- Perioperative mortality: 2.7%
Complications of Hepatobiliary Surgery: An Overview
It’s important to know about the risks of hepatobiliary surgery. This surgery is complex and can be dangerous. It involves the liver and bile ducts.
Hepatobiliary surgery comes with big risks. One major issue is bile leaks. These can make recovery harder. Complications can be sorted by how serious they are, when they happen, and what they are.
Classification of Complications
There are many ways to group complications from hepatobiliary surgery. One way is by type, like biliary, vascular, or infectious issues. This helps doctors understand and treat each problem better.
The table below shows a simple way to group complications:
|
Type of Complication |
Description |
Examples |
|---|---|---|
|
Biliary Complications |
Problems with the bile ducts |
Bile leaks, biliary strictures |
|
Vascular Complications |
Issues with blood vessels |
Hepatic artery thrombosis, portal vein thrombosis |
|
Infectious Complications |
Problems caused by infection |
Surgical site infections, intra-abdominal abscesses |
Grading Severity of Complications
Doctors use systems like the Clavien-Dindo classification to rate complications. This system goes from I (minor) to V (death). Rating complications helps doctors understand their impact and how to manage them.
Timing of Complications
Complications can happen at any time, from during surgery to years later. Knowing when complications occur is key to preventing and treating them.
By understanding and grading complications, doctors can create better plans for prevention and treatment. This helps improve outcomes for patients having hepatobiliary surgery.
Biliary Complications
Biliary complications are a big worry after hepatobiliary surgery. They can affect how well a patient recovers. Bile leaks and biliary strictures are two major issues.
Bile Leaks
Bile leaks happen in 6.5% to 27.2% of patients after surgery. They can cause infections, longer stays in the hospital, and even death. The risk depends on the surgery type, liver health, and overall patient health.
Biliary Strictures
Biliary strictures can come from surgery or bile duct injury. They can block bile flow, leading to jaundice and infections. This might need more treatment.
Impact on Hospitalization and Mortality
Biliary problems can make recovery harder. They lead to longer hospital stays, higher costs, and a greater risk of death.
|
Type of Complication |
Incidence Rate |
Impact |
|---|---|---|
|
Bile Leaks |
6.5-27.2% |
Increased infection rates, prolonged hospitalization, higher mortality |
|
Biliary Strictures |
Variable |
Obstructive jaundice, cholangitis, need for further intervention |
Handling biliary issues needs a team effort. This includes conservative management, interventional radiology, and sometimes surgical reintervention. Knowing the risks and taking steps to prevent them is key.
Vascular Complications Following Hepatobiliary Surgery
Vascular problems after hepatobiliary surgery can be very serious. They can greatly affect patient outcomes. Managing these issues is complex.
Hepatic Artery Thrombosis
Hepatic artery thrombosis is a major concern after surgery. It happens when a blood clot forms in the hepatic artery. This can cause liver ischemia and failure.
Prompt diagnosis and treatment are key to avoid graft loss and severe outcomes.
Portal Vein Thrombosis
Portal vein thrombosis is another serious issue. It’s when a blood clot forms in the portal vein. This can lead to portal hypertension and variceal bleeding.
Early detection is critical to manage it well and prevent liver damage.
Hemorrhagic Complications
Bleeding is a risk after hepatobiliary surgery. It can come from the surgical site or vascular injuries. Effective hemostasis during surgery and careful postoperative monitoring are vital to reduce bleeding risks.
Managing vascular complications needs a team effort. Surgeons, radiologists, and other healthcare professionals must work together. Knowing the risks and taking preventive steps can help lower complication rates.
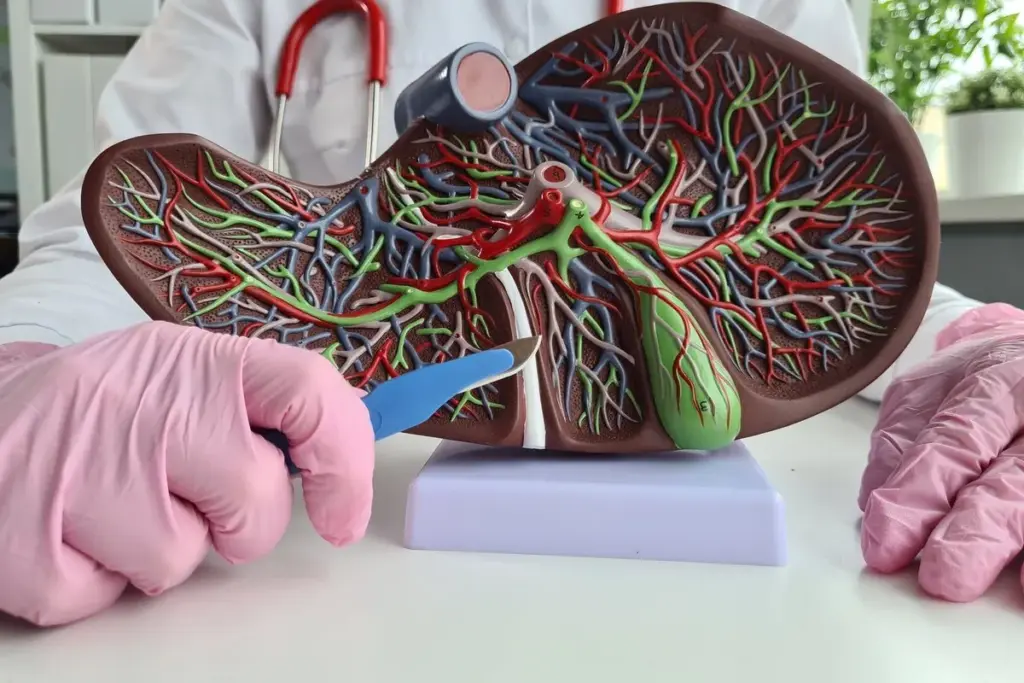
Liver-Specific Complications
After liver surgery, specific complications can arise. These can affect how well a patient does and their quality of life.
Post-Hepatectomy Liver Failure
Post-hepatectomy liver failure happens in about 35.7% of cases. It’s when the liver can’t recover or work right after surgery. Early detection and management are key to stop things from getting worse.
Factors that increase the risk include how much liver is removed, the liver’s condition before surgery, and the patient’s liver function beforehand. Knowing these can help doctors adjust care to lower the risk of this problem.
Small-for-Size Syndrome
Small-for-size syndrome happens when the liver left after surgery is too small. It leads to long-term cholestasis, ascites, and coagulopathy. It’s a serious issue that can come up after big liver surgeries.
To manage small-for-size syndrome, doctors try to make the liver left work better. They use strategies to boost liver regeneration and support care.
Hepatic Encephalopathy
Hepatic encephalopathy is a brain problem caused by liver issues. It can cause anything from mild confusion to coma. Quick action and treatment are vital to stop it from getting worse and to help the patient.
Managing hepatic encephalopathy means lowering ammonia levels, fixing electrolyte imbalances, and fixing things that make it worse. Doctors often use lactulose and rifaximin to treat it.
Liver-specific problems like post-hepatectomy liver failure, small-for-size syndrome, and hepatic encephalopathy are serious. They can greatly affect how well a patient does. It’s important to understand these issues to prevent and manage them.
Infectious Complications After Hepatobiliary Procedures
The risk of infections after liver and bile duct surgery is a big worry for doctors and healthcare teams. These infections can make patients sicker, keep them in the hospital longer, and cost more money.
These infections can show up in different ways, like infections at the surgery site, abscesses in the belly, and cholangitis. Knowing about these risks helps doctors prevent and treat them better.
Surgical Site Infections
Surgical site infections (SSIs) are a common problem after liver and bile duct surgery. These infections can be mild or serious, affecting the skin or deeper tissues.
Risk factors for SSIs include things like diabetes and being overweight. Also, longer surgeries and dirty surgical sites can increase the risk.
Intra-abdominal Abscesses
Intra-abdominal abscesses are serious infections that can happen after liver and bile duct surgery. These are pockets of pus in the belly that need to be drained.
To find these abscesses, doctors use CT scans. Then, they drain them to treat the infection.
Cholangitis
Cholangitis is inflammation of the bile ducts, often caused by infection. It can happen after surgery, if the bile ducts get blocked or stagnant.
Managing cholangitis means using antibiotics. Sometimes, doctors need to do an ERCP to clear the blockage in the bile ducts.
|
Type of Complication |
Description |
Management Strategies |
|---|---|---|
|
Surgical Site Infections |
Infections involving the skin or deep tissues at the surgical site |
Antibiotics, wound care, possible surgical debridement |
|
Intra Abdominal Abscesses |
Collections of pus in the abdominal cavity |
Imaging-guided drainage, antibiotics |
|
Cholangitis |
Inflammation of the bile ducts, often due to infection |
Antibiotics, ERCP for bile duct clearance |
In conclusion, infections after liver and bile duct surgery are a big worry. Knowing about these infections and how to treat them is key to helping patients get better.
Systemic Complications
After hepatobiliary surgery, patients might face systemic complications. These include pulmonary, renal, and cardiovascular issues. These problems can greatly affect how well a patient does and their quality of life.
Pulmonary Complications
Pulmonary issues are a big worry after these surgeries. They can be anything from mild atelectasis to severe ARDS.
- Pneumonia
- Atelectasis
- Acute Respiratory Distress Syndrome (ARDS)
Pulmonary complications can be minimized with the right care before and after surgery. This includes respiratory therapy and getting patients moving early.
Renal Dysfunction
Renal dysfunction is another serious issue that can happen after surgery. It can lead to more problems and even death.
Things that increase the risk of renal dysfunction include:
- Pre-existing kidney disease
- Hypovolemia
- Nephrotoxic medications
Cardiovascular Events
Cardiovascular events, like heart attacks and cardiac arrests, can also happen after surgery. These are often linked to heart disease.
|
Cardiovascular Risk Factors |
Description |
|---|---|
|
Hypertension |
High blood pressure |
|
Hyperlipidemia |
Elevated levels of lipids in the blood |
|
Diabetes Mellitus |
Chronic condition affecting blood sugar regulation |
In conclusion, systemic complications after hepatobiliary surgery are complex. They need a detailed plan for prevention and management.
Risk Factors for Developing Complications
It’s key to know the risks linked to hepatobiliary surgery to better patient care. Many factors can lead to complications. Knowing these can help lower risks.
Patient-Related Factors
Factors related to the patient greatly affect complication risks. Advanced age is a big risk, as older people often have more health issues. Other factors include pre-existing liver disease, diabetes, and obesity. These can make surgery and recovery harder.
- Advanced age
- Pre-existing liver disease
- Diabetes
- Obesity
Surgery-Related Factors
Factors related to the surgery itself also matter a lot. The duration of surgery and the extent of resection are key. Longer surgeries and more complex ones carry higher risks.
- Longer surgery times
- Complex resections
- Type of surgical approach (open vs. laparoscopic)
Disease-Related Factors
The type and stage of the disease also affect risks. Patients with advanced disease or certain tumors face higher risks.
- Type and stage of hepatobiliary disease
- Presence of cirrhosis or fibrosis
Understanding these risks helps doctors take steps to reduce complications. This improves outcomes for patients having hepatobiliary surgery.
Diagnostic Approaches to Postoperative Complications
Diagnosing postoperative complications after liver and bile duct surgery is a team effort. It combines clinical checks and advanced tests. Finding problems early is key to treating them well.
Clinical Assessment
First, doctors check the patient’s history and body. They look for signs and symptoms that might show a problem.
Key parts of this check include:
- Watching vital signs
- Checking pain levels
- Looking at the wound
- Listening to what the patient says
Laboratory Investigations
Lab tests are vital for spotting postoperative issues. They give doctors real data on how the patient is doing.
Some common tests are:
- Liver function tests
- Complete blood count
- Bilirubin levels
- Coagulation profiles
|
Laboratory Test |
Purpose |
|---|---|
|
Liver Function Tests |
Check for liver damage or problems |
|
Complete Blood Count |
Look for signs of infection or bleeding |
|
Bilirubin Levels |
Spot biliary blockages or issues |
Imaging Modalities
Imaging tools are key for seeing inside the liver and bile ducts. They help find any issues.
Some common imaging methods are:
- Ultrasound
- Computed Tomography (CT) scans
- Magnetic Resonance Cholangiopancreatography (MRCP)
By using clinical checks, lab tests, and imaging, doctors can find and treat postoperative problems after liver and bile duct surgery.
Management Strategies for Hepatobiliary Complications
Managing hepatobiliary complications needs a mix of strategies. Each complication is unique, so the approach must match it.
Conservative Management
For some issues, starting with conservative management is best. This might include antibiotic therapy, nutrition support, and watching the patient closely.
Interventional Radiology Approaches
Interventional radiology is key for problems like bile leaks or blood vessel issues. Methods like embolization or drainage can fix these without surgery.
|
Procedure |
Indications |
Benefits |
|---|---|---|
|
Embolization |
Bleeding, vascular malformations |
Minimally invasive, reduces risk of further surgery |
|
Drainage |
Bile leaks, abscesses |
Reduces infection risk, promotes healing |
Surgical Reintervention
Sometimes, surgery is needed to handle complications. This might mean going back to a previous surgery site or dealing with new problems.
Multidisciplinary Team Approach
Working together is key in managing hepatobiliary complications. Surgeons, radiologists, and others team up to give the best care.
Prevention of Complications in Hepatobiliary Surgery
The success of hepatobiliary surgery depends on avoiding complications. This is achieved through careful planning and execution. Several strategies are used to prevent complications.
Preoperative Optimization
Preoperative optimization is key to reducing complication risks. It involves a detailed check of the patient’s health. This includes looking at any existing health issues that might affect surgery outcomes.
Improving nutritional status and managing chronic conditions like diabetes are important. Ensuring the patient is in the best shape before surgery is critical.
Pre-surgery imaging and tests are also vital. They help plan the surgery, lowering the chance of unexpected problems during the operation.
Intraoperative Techniques
Intraoperative techniques are also vital in preventing complications. Surgeons must use precise techniques to avoid tissue damage. This reduces the risk of bleeding or other issues during surgery.
Using advanced technologies like electrosurgical units and surgical staplers can improve surgery precision. This reduces complication risks.
Enhanced Recovery After Surgery (ERAS) Protocols
ERAS protocols are a big step forward in surgical care. They focus on reducing surgical stress and keeping organs working well after surgery. This helps with faster recovery.
ERAS includes preoperative counseling, nutrition optimization, standard pain management, and early movement. These steps help lower complication risks and improve patient results.
In summary, preventing complications in hepatobiliary surgery needs a full approach. This includes preoperative preparation, careful surgery techniques, and ERAS protocols. By focusing on these, surgeons and healthcare teams can reduce risks and better patient outcomes.
Modern Advances in Reducing Surgical Complications
New surgical techniques and better care before and after surgery have changed hepatobiliary surgery. These changes have made surgeries safer and more precise. Now, surgeons can handle complex tasks with more skill and safety.
Minimally Invasive Approaches
Minimally invasive surgery is now common in hepatobiliary surgery. It helps reduce pain, shortens hospital stays, and leaves less scarring. Techniques like laparoscopic and robotic-assisted surgeries offer better views and control.
Benefits of Minimally Invasive Approaches:
- Reduced postoperative pain
- Shorter hospital stays
- Less visible scarring
- Quicker recovery times
Technological Innovations
New technologies have greatly improved hepatobiliary surgery outcomes. Tools like intraoperative ultrasound, fluorescence imaging, and 3D printing help plan and perform surgeries better.
|
Technological Innovation |
Description |
Benefit |
|---|---|---|
|
Intraoperative Ultrasound |
Real-time imaging during surgery |
Improved tumor localization |
|
Fluorescence Imaging |
Visualization of blood flow and bile ducts |
Reduced risk of bile duct injury |
|
3D Printing |
Creation of patient-specific anatomical models |
Enhanced surgical planning |
Perioperative Care Improvements
Improvements in care before and after surgery have also cut down on complications. Better recovery after surgery (ERAS) protocols, new anesthesia methods, and enhanced pain management have all helped. These changes have made patients’ outcomes better.
ERAS protocols have been very effective. They involve a team effort for care before, during, and after surgery. This approach aims to reduce stress, manage pain well, and speed up recovery.
Key Components of ERAS Protocols:
- Preoperative counseling and optimization
- Standardized analgesic and anesthetic regimens
- Minimally invasive surgical techniques
- Goal-directed fluid therapy
- Early mobilization and oral feeding
Quality Metrics and Outcomes in Hepatobiliary Surgery
Quality metrics are key in checking how well hepatobiliary surgeries work. They help see if patients get good care during complex surgeries.
Institutional Performance Measures
Institutional performance measures check how well healthcare places do. They look at morbidity rates, mortality rates, and readmission rates. These are important for seeing how well hepatobiliary surgery units do.
|
Performance Measure |
Description |
Benchmark |
|---|---|---|
|
Morbidity Rate |
Rate of complications after surgery |
< 20% |
|
Mortality Rate |
Rate of death after surgery |
< 5% |
|
Readmission Rate |
Rate of hospital readmission after discharge |
< 10% |
Long-term Survival Rates
Long-term survival rates are very important for patients having hepatobiliary surgery. These rates depend on many things. Like the disease stage, how well the surgery goes, and post-surgery care.
Survival analysis helps figure out survival chances over time. It gives insights into the long-term results of hepatobiliary surgery.
Quality of Life After Complications
Quality of life after surgery is a big part of patient care in hepatobiliary surgery. Surgery complications can really affect a patient’s health and mood. This can change their life quality a lot.
Checking quality of life means looking at physical function, emotional well-being, and social functioning. This info is key for making plans to better patient results and improve their life quality.
Conclusion
Hepatobiliary surgery comes with big risks, like many complications that can affect how well a patient does. It’s key for doctors to know about these risks to find ways to manage them better.
Doctors can spot and prevent problems like biliary, vascular, and liver issues. They can also catch infections and systemic problems early. This helps a lot in keeping patients safe.
At Liv Hospital, we’re all about giving top-notch care and cutting down on complications. We keep up with the latest in surgery, like new tech and less invasive methods. This helps patients live better and longer after surgery.
Handling complications in hepatobiliary surgery needs a team effort. This team uses different ways to help patients, like watching them closely, using special treatments, and sometimes doing surgery again. By focusing on preventing problems and improving care, doctors can make surgery safer and more successful for everyone.
FAQ
What are the most common complications of hepatobiliary surgery?
Common issues include bile leaks and strictures, and problems with blood vessels. Liver failure after surgery is also a concern.
How are complications of hepatobiliary surgery classified?
They’re sorted by how severe and when they happen. Knowing this helps in managing and preventing them.
What are the risk factors for developing complications after hepatobiliary surgery?
Factors include the patient’s health, the surgery itself, and the disease being treated. Understanding these helps prevent and manage issues.
How are postoperative complications diagnosed?
Doctors use clinical checks, lab tests, and imaging to find complications.
What are the management strategies for hepatobiliary complications?
Strategies include watching and waiting, using radiology, and sometimes surgery. A team approach is key to managing complications.
How can complications be prevented in hepatobiliary surgery?
Prevention involves getting the patient ready for surgery, using special techniques during surgery, and following ERAS protocols.
What are the modern advances in reducing surgical complications?
Advances include less invasive surgery, new technologies, and better care before and after surgery. These have helped lower complication rates.
What are the quality metrics used to evaluate outcomes in hepatobiliary surgery?
Metrics include how well a hospital does, survival rates, and quality of life after surgery.
What is the overall morbidity rate for hepatobiliary surgery?
The rate is about 28.4%, with serious issues in 18.6% of cases.
What is the perioperative mortality rate for hepatobiliary surgery?
The death rate is about 2.7% during and right after surgery.
How do biliary complications impact hospitalization and mortality?
Biliary issues, like bile leaks, can lead to longer hospital stays and higher death rates. They also increase the risk of infections and other serious problems.
What are the liver-specific complications after liver surgery?
Specific liver issues include liver failure after surgery, small liver syndrome, and brain problems due to liver issues.
What are the systemic complications that can occur after hepatobiliary surgery?
Systemic issues include lung problems, kidney issues, and heart problems.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11374351/[1





