Last Updated on December 3, 2025 by Bilal Hasdemir

Liver cancer in kids is rare but serious. Hepatoblastoma is the most common type. Knowing if it’s benign or malignant is key to treating it right. Is Hepatoblastoma malignant? Yes! Get the crucial facts on this scary type of childhood cancer and what it means.
Pediatric liver tumors need careful diagnosis and treatment. Whether hepatoblastoma is benign or malignant affects treatment and chances of recovery.
Exploring hepatoblastoma shows it’s vital to know if it’s malignant. This helps tackle liver cancer in kids more effectively.
Key Takeaways
- Hepatoblastoma is a rare liver cancer mainly in children.
- Figuring out if hepatoblastoma is benign or malignant is vital for treatment.
- Pediatric liver tumors need exact diagnosis and care.
- The type of hepatoblastoma greatly impacts treatment and outcome.
- Understanding hepatoblastoma’s traits is essential for effective treatment.
Understanding Hepatoblastoma: A Rare Liver Cancer
Hepatoblastoma is the most common liver cancer in kids. It’s a rare liver tumor that needs quick and effective treatment. Parents and doctors must know about it to help kids get better fast.
Definition and Occurrence Rates
Hepatoblastoma is a cancer that starts in the liver. It’s the top liver cancer in kids, making up about 1% of all childhood cancers. Even though it’s rare, it has a big impact on kids and their families.
This cancer usually hits kids under 3, mostly in the first 18 months. This early start makes it very important for parents and doctors to stay alert.
| Age Group | Incidence Rate |
| 0-1 year | High |
| 1-3 years | Moderate |
| 3+ years | Low |
Primary Affected Population
Young kids, mainly those under 3, are most at risk for hepatoblastoma. Their livers are more vulnerable because of genetics and the environment.
Some genetic conditions can raise the risk of getting this cancer. Knowing these risks helps catch it early and treat it better.
Knowing about hepatoblastoma helps us tackle this rare liver cancer in kids better. We can improve how we diagnose and treat it.
The Malignant Nature of Hepatoblastoma

It’s important to understand the bad side of hepatoblastoma to find good treatments. This rare and fast-growing liver cancer mainly hits kids.
Classification as a Malignant Tumor
Hepatoblastoma is seen as a bad tumor because it grows fast and can spread. Doctors say we need quick and full treatment for it.
Aggressive Growth Patterns
The tumor grows quickly, making the liver big and causing pain. Aggressive growth patterns mean we must act fast.
Metastatic Potential
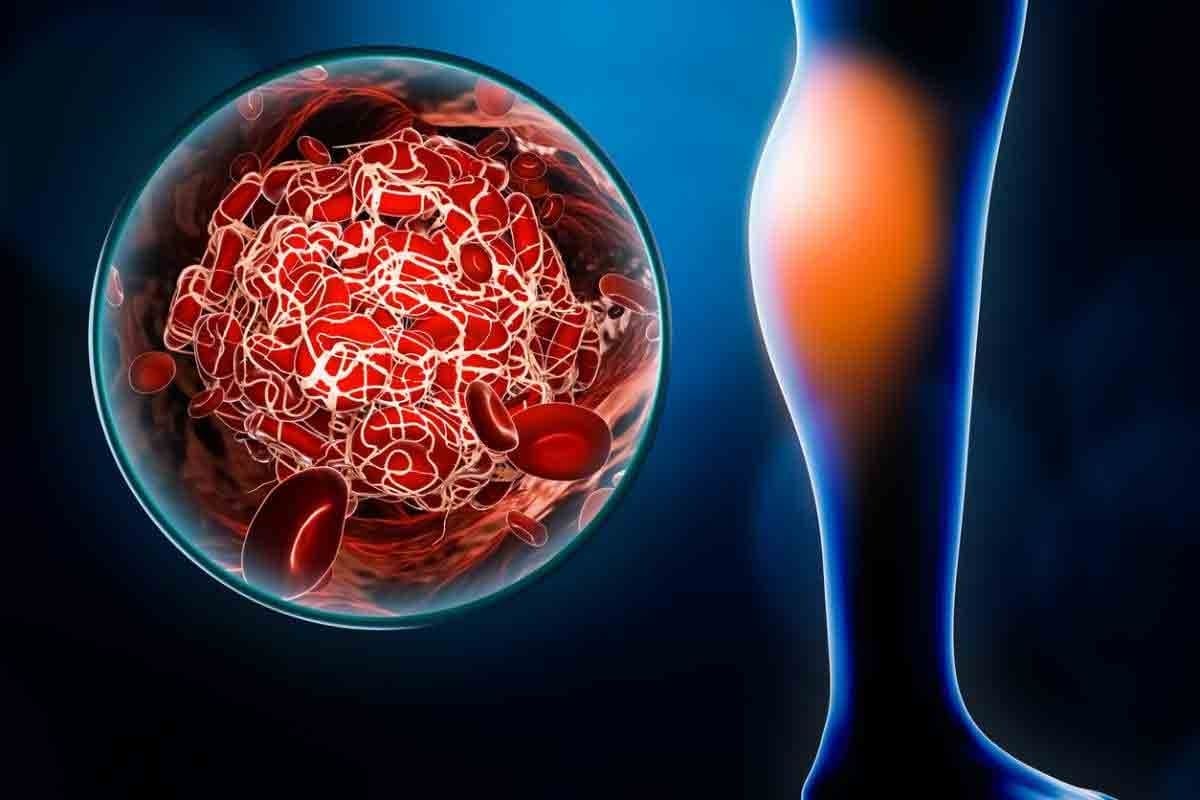
Hepatoblastoma can spread to places like the lungs and lymph nodes. This shows we need to check how far it has spread.
Looking into hepatoblastoma’s bad side, we see it needs a team effort to treat. This involves many doctors and a detailed care plan.
Cellular Origins and Pathophysiology
Hepatoblastoma starts with the wrong development of liver cells in embryos. This is due to genetic changes and broken molecular paths. Knowing these causes helps us find better treatments for this rare liver cancer in kids.
Embryonal Tissue Development
Hepatoblastoma comes from liver cells that don’t grow right during fetal life. These cells can form tumors with different levels of maturity. They can be very young or almost adult-like.
Embryonal liver development is a complex process. It needs many genetic and environmental factors to work right. When it goes wrong, it can cause hepatoblastoma.
Genetic Mutations in Hepatoblastoma
Genetic changes are key in making hepatoblastoma. The CTNNB1 gene, which makes β-catenin, is often changed in these tumors. This change turns on the Wnt/β-catenin pathway, making cells grow and tumors grow too.
“The Wnt/β-catenin pathway is very important in making hepatoblastoma. Its wrong working is a big sign of this disease.”
Other changes, like in the TP53 gene and the MYC oncogene, also help make hepatoblastoma.
Molecular Pathways Involved
Many molecular paths help make and grow hepatoblastoma. The Wnt/β-catenin pathway is a big one. The Notch, Hedgehog, and PI3K/AKT paths also play a part.
| Molecular Pathway | Role in Hepatoblastoma |
| Wnt/β-catenin | Promotes cell proliferation and tumor growth |
| Notch | Involved in cell differentiation and survival |
| Hedgehog | Regulates cell growth and development |
Knowing these paths is key to making targeted treatments for hepatoblastoma. It helps improve liver tumor treatment and hepatoblastoma prognosis in kids.
Risk Factors for Developing Hepatoblastoma
Some genetic conditions and syndromes raise the risk of getting hepatoblastoma. Knowing these risk factors helps find kids at higher risk. This can lead to early screening.
Genetic Predisposition
Genetic predisposition is key in hepatoblastoma. Kids with certain genetic syndromes face a higher risk. Genetic counseling and testing might be suggested for families with such histories.
Familial Adenomatous Polyposis
Familial adenomatous polyposis (FAP) causes many polyps in the colon. It raises the risk of hepatoblastoma, mainly in children. Early diagnosis of FAP is vital for managing cancer risks.
Beckwith-Wiedemann Syndrome
Beckwith-Wiedemann syndrome is a genetic disorder leading to overgrowth. It also increases cancer risk, including hepatoblastoma. Kids with this syndrome need regular monitoring for tumors.
Other Associated Conditions
Other genetic conditions, like Glycogen storage disease type I and some chromosomal abnormalities, also raise hepatoblastoma risk. Knowing these links helps in early detection and management.
Identifying kids at higher risk due to genetics or other conditions helps. Healthcare providers can then use surveillance to catch hepatoblastoma early. This makes treatment more effective.
Signs and Symptoms of Hepatoblastoma in Children
It’s important to know the signs of hepatoblastoma in kids for early treatment. This rare liver cancer can be hard to spot early because its symptoms are not clear-cut.
Early Warning Signs
The first signs of hepatoblastoma can be hard to notice. Kids might lose their appetite and start losing weight. These signs can mean many things, making it hard to catch the disease early.
Abdominal Manifestations
As the disease gets worse, the belly symptoms get clearer. You might see:
- The belly gets bigger because of the tumor
- Pain or discomfort in the upper right belly
- A mass in the belly that you can feel
These signs happen because the tumor is growing and pressing on other parts.
Systemic Symptoms
Kids with hepatoblastoma might also feel tired, have fever, lose weight, and not want to eat. These signs show how the body is reacting to the tumor.
When to Seek Medical Attention
Parents and caregivers need to know when to get medical help. If a child has ongoing or severe belly pain, loses a lot of weight, or has a big belly mass, they need to see a doctor right away.
| Symptom | Description | Action |
| Abdominal Distension | Swelling of the abdomen due to tumor growth | Consult a pediatrician |
| Weight Loss | Unexplained loss of weight | Schedule a medical check-up |
| Fatigue | Persistent feeling of tiredness | Discuss with a healthcare provider |
Finding and treating hepatoblastoma early can really help kids. If you think your child might have symptoms of this disease, see a doctor fast.
“Early diagnosis of hepatoblastoma is critical for effective treatment and improved survival rates in children.”Expert Opinion
Diagnostic Approaches for Hepatoblastoma
Diagnosing hepatoblastoma in children involves several steps. We use physical exams, lab tests, and imaging studies. This multi-disciplinary approach helps ensure accurate diagnosis and guides treatment.
Physical Examination Findings
A thorough physical exam is the first step. We look for signs like abdominal swelling or a mass. Children might also show jaundice or other symptoms that need further checks.
Laboratory Tests and Tumor Markers
Laboratory tests are key in diagnosing. We focus on tumor markers, like alpha-fetoprotein (AFP), which is often high in children with this cancer. We also do liver function tests and complete blood counts to check overall health.
Tumor markers like AFP are critical in diagnosing and monitoring hepatoblastoma. High levels show the tumor’s presence and help track treatment success.
Imaging Studies
Imaging studies help us see the tumor and its size. Ultrasound is often the first choice because it’s non-invasive and shows images in real-time. MRI or CT scans might follow to see the tumor’s details and check for spread.
Biopsy and Histological Examination
A biopsy and histological exam confirm the diagnosis. We look at the tumor cells to confirm they are cancerous and classify the tumor. This info is key for choosing the right treatment.
Diagnosing hepatoblastoma is complex and needs a team effort. By combining physical exams, lab tests, imaging, and biopsy results, we can accurately diagnose and stage the cancer. This guides treatment decisions.
Staging Systems for Hepatoblastoma
Staging hepatoblastoma accurately is key for doctors to choose the right treatment. Staging systems show how far the disease has spread. This is important for knowing the patient’s chances and treatment options.
PRETEXT Staging System
The PRETEXT system is a common way to stage hepatoblastoma. It looks at how much of the liver the tumor effects before treatment starts. The system divides tumors into stages based on how many liver sectors are involved.
- PRETEXT I: Three adjoining sectors are free.
- PRETEXT II: Two adjoining sectors are free.
- PRETEXT III: One sector is free, or two non-adjoining sectors are free.
- PRETEXT IV: All four sectors are involved.
This helps doctors plan surgery and guess how well the patient will do.
COG Staging System
The Children’s Oncology Group (COG) staging is also used for hepatoblastoma. It looks at if the tumor can be removed and if there are distant metastases.
- Stage I: Completely resected tumor.
- Stage II: Tumor is resected but with microscopic residual disease.
- Stage III: Tumor is not completely resected or has gross residual disease.
- Stage IV: Distant metastatic disease is present.
The COG system helps predict how well a patient will do and guides treatment.
Importance of Accurate Staging
Accurate staging of hepatoblastoma is very important. It helps predict how well a patient will do, plan treatment, and see if the disease will come back. Both PRETEXT and COG systems are used together to fully understand the disease.
Accurate staging means patients get treatments that fit their needs. Doctors, radiologists, surgeons, and oncologists work together to consider all parts of the disease.
In conclusion, staging systems for hepatoblastoma are essential in managing this rare liver cancer. Accurate staging lets doctors create effective treatment plans, which improves patient outcomes.
Treatment Modalities for Hepatoblastoma
Effective treatment of hepatoblastoma needs a mix of local and systemic treatments. Surgery and chemotherapy are key. We’ll look at these options and how they help manage this complex disease.
Surgical Approaches
Surgery is a mainstay in treating hepatoblastoma, aiming to remove the tumor fully. Surgical resection is tricky due to the tumor’s size and location. But, new surgical methods have made treatment better. We use preoperative imaging to plan surgery well.
The goal of surgery is to remove the tumor completely. Sometimes, liver transplantation is needed for tumors that can’t be removed.
Chemotherapy Protocols
Chemotherapy is vital in treating hepatoblastoma. It’s used before surgery to shrink tumors and after to kill any cancer cells left. Cisplatin-based regimens are often used and work well.
We customize chemotherapy for each patient. This depends on the tumor and the patient’s health. Monitoring for response and adjusting treatment is key.
Radiation Therapy
Radiation therapy is used less often but can be effective. It’s used when surgery isn’t possible. We use advanced techniques to protect healthy tissues.
Novel and Targeted Therapies
Research into novel and targeted therapies is promising. These therapies target specific weaknesses in cancer cells. This could reduce side effects of traditional treatments.
We’re looking into targeted agents that kill cancer cells without harming normal tissues. Clinical trials are important to check if these treatments are safe and work well.
Survival Rates and Prognosis Factors
Survival rates for hepatoblastoma depend on several factors. These include the stage at diagnosis and how well the body responds to treatment. Knowing these factors helps patients and their families understand the treatment journey.
Overall Survival Statistics
In recent years, survival rates for hepatoblastoma have greatly improved. Studies show that the survival rate for children with this disease is now over 80% in some cases. This improvement is thanks to better treatments like surgery, chemotherapy, and radiation therapy.
Key statistics include:
- Overall 5-year survival rate: approximately 70-80%
- Survival rate for localized disease: up to 90%
- Survival rate for metastatic disease: around 50-60%
Factors Affecting Prognosis
Several factors impact the prognosis of hepatoblastoma. These include:
- Stage at Diagnosis: Early diagnosis greatly improves chances of survival.
- Response to Therapy: Patients who respond well to chemotherapy have a better outlook.
- Tumor Biology: The type of tumor and genetic mutations can affect prognosis.
- Age at Diagnosis: Younger children generally have a better prognosis.
Long-term Survival Outcomes
Thanks to better treatments, long-term survival for hepatoblastoma patients has improved. Yet, it’s vital to keep up with long-term follow-ups. This is to watch for late effects of treatment and any possible recurrence. Many children with hepatoblastoma can live long, healthy lives with the right treatment.
“The improvement in survival rates for hepatoblastoma is a testament to the advancements in pediatric oncology. Continued research and follow-up care are essential for the best outcomes.” -A leading pediatric oncologist
We stress the need for complete care and follow-up for children with hepatoblastoma. This ensures the best possible results for them.
Potential Complications and Long-term Effects
Treatment for hepatoblastoma saves lives but can also cause problems. It’s important to know the challenges patients face after treatment. This rare liver cancer treatment is complex.
Treatment-related Complications
Treatment for hepatoblastoma includes surgery, chemotherapy, and sometimes radiation. These treatments save lives but can cause issues. For example, chemotherapy can lead to myelosuppression, causing anemia and other blood problems.
Surgery can result in infections, bleeding, and adhesions. Some patients may lose their hearing due to ototoxicity from certain chemotherapy agents. Treatments can also harm the liver, leading to cirrhosis or liver failure in severe cases.
Growth and Development Concerns
Children treated for hepatoblastoma may have growth and developmental issues. Chemotherapy and radiation can affect bone growth, leading to short stature or skeletal problems. Treatments during critical periods can also impact cognitive and emotional development.
Risk of Secondary Malignancies
One major concern is the risk of secondary cancers from treatment. Chemotherapy and radiation can increase this risk. Long-term surveillance is key for survivors.
Quality of Life Considerations
The quality of life for survivors can be affected by treatment. Physical, emotional, and social challenges are common. Healthcare providers must offer support to address these issues.
To understand long-term effects and complications, let’s look at some statistics:
| Complication | Frequency | Impact on Quality of Life |
| Ototoxicity | 20-30% | High |
| Growth Abnormalities | 15-25% | Moderate to High |
| Secondary Malignancies | 5-10% | Very High |
Knowing these complications and long-term effects is key to providing care. Healthcare providers can better support patients and their families. This support is vital throughout the treatment journey and beyond.
Recurrence and Follow-up Care
Managing hepatoblastoma is not just about the first treatment. It also includes ongoing care to watch for recurrence. A good follow-up plan is key to catch any signs early and handle them well.
Monitoring for Recurrence
Regular checks are vital to spot recurrence early. This means physical exams, lab tests, and imaging. Sticking to a follow-up plan helps catch any changes quickly.
Key components of monitoring include:
- Regular physical examinations to check for any abnormalities
- Laboratory tests, including tumor markers like alpha-fetoprotein (AFP)
- Imaging studies such as ultrasound, CT scans, or MRI
Recommended Follow-up Schedule
The follow-up plan depends on the patient’s risk and how they first responded to treatment. Here’s a general outline:
- Frequent visits in the first two years, every 3-6 months
- Less often as time goes on, but keep watching
- Adjust the schedule based on the patient’s health and risk
It’s vital for patients and their families to stick to the follow-up plan. This helps achieve the best results.
Management of Recurrent Disease
If recurrence happens, we create a plan just for that case. This might include:
- Checking how far the recurrence has spread with imaging and biopsy
- Looking into second treatments like more chemo, surgery, or radiation
- Trying new treatments in clinical trials if it’s a good fit
Dealing with recurrent hepatoblastoma is tough, but with the right plan and quick action, we can help patients do better. Our team is here to offer the care and support needed every step of the way.
Current Research and Future Directions
Research into hepatoblastoma is moving fast, leading to new discoveries. These findings are helping us understand the disease better and find new treatments.
Advances in Molecular Understanding
Recent studies have greatly improved our knowledge of hepatoblastoma’s molecular basis. They’ve found genetic mutations and pathways that could be treated. For example, the CTNNB1 gene is often mutated, pointing to the Wnt/β-catenin pathway as a possible treatment target.
Next-generation sequencing has also helped us see the disease’s genetic makeup more clearly. This has uncovered new genetic changes that could help diagnose or treat the disease.
Emerging Treatment Approaches
Treatment for hepatoblastoma is getting more personalized. New methods include targeted therapies and immunotherapy. Researchers are looking into drugs that target specific genetic changes in the disease, like the Wnt/β-catenin pathway.
- Targeted therapies aimed at specific genetic mutations
- Immunotherapy approaches, including checkpoint inhibitors
- Novel chemotherapy regimens with improved efficacy and reduced toxicity
Clinical Trials for Hepatoblastoma
Clinical trials are key to improving hepatoblastoma treatment. They’re testing new treatments, like targeted agents and immunotherapies. For instance, a recent study showed a new chemotherapy regimen greatly improved outcomes for high-risk patients.
“The integration of new therapeutic agents into clinical practice is expected to improve outcomes for patients with hepatoblastoma.”
Precision Medicine Applications
Precision medicine is changing how we treat hepatoblastoma. It tailors treatment to each patient’s unique genetic profile. By analyzing a tumor’s genetics, doctors can choose the best targeted therapies.
The future of treating hepatoblastoma looks bright with precision medicine leading the way. Ongoing research aims to find new targets and treatments. As we learn more, we’ll see better patient outcomes and less side effects from treatment.
Conclusion: The Journey with Hepatoblastoma
Learning about hepatoblastoma, a rare liver cancer in kids, is key for early detection and treatment. We’ve looked into its dangerous nature, where it starts, and what increases the risk.
Diagnosing hepatoblastoma requires imaging, lab tests, and biopsies. Knowing how far the cancer has spread helps doctors choose the best treatment. Treatments include surgery, chemotherapy, and sometimes radiation. Researchers are also exploring new, targeted treatments.
Thanks to research, more kids with hepatoblastoma are surviving. But, we need to keep working to beat the disease’s return, long-term side effects, and find better treatments.
We must support families and deepen our knowledge of this complex disease. This will help improve care for kids with hepatoblastoma, liver cancer, and other childhood cancers.
FAQ
What is hepatoblastoma, and is it benign or malignant?
Hepatoblastoma is a rare liver cancer found mainly in children. It’s considered malignant because it grows aggressively and can spread to other parts of the body.
What are the risk factors for developing hepatoblastoma?
Certain genetic conditions, like familial adenomatous polyposis, increase the risk. Also, conditions like Beckwith-Wiedemann syndrome can play a role.
What are the common signs and symptoms of hepatoblastoma in children?
Symptoms include swelling, pain, or discomfort in the abdomen. Children may also lose weight, feel tired, or have less appetite.
How is hepatoblastoma diagnosed?
Doctors use physical exams, lab tests, and imaging like ultrasound and CT scans. A biopsy is also needed for a diagnosis.
What are the treatment options for hepatoblastoma?
Treatments include surgery, chemotherapy, and sometimes radiation. New, targeted therapies are also being tested.
What is the prognosis for children diagnosed with hepatoblastoma?
The outlook depends on the tumor’s stage, how well it responds to treatment, and if it has spread. Thanks to modern treatments, survival rates have gotten better.
What are the long-term effects of hepatoblastoma treatment?
Children may face complications from treatment, like growth issues. There’s also a risk of getting another cancer later. Their quality of life can be affected too.
Why is follow-up care important in hepatoblastoma?
Follow-up care helps catch any signs of the cancer coming back. It also helps manage any lasting effects from treatment and keeps the child’s overall health in check.
What are the current research directions in hepatoblastoma?
Researchers are studying the cancer’s molecular makeup and testing new treatments. They’re also looking into precision medicine and running clinical trials.
How does staging impact treatment decisions and prognosis in hepatoblastoma?
Staging systems like PRETEXT and COG help doctors understand how far the cancer has spread. This information guides treatment plans and gives a better idea of the child’s chances of recovery.
What is the role of chemotherapy in treating hepatoblastoma?
Chemotherapy is a key part of treating hepatoblastoma. It’s often used along with surgery and other treatments to get the best results.
Can hepatoblastoma be treated with targeted therapies?
Yes, researchers are exploring targeted therapies in clinical trials. These new treatments might offer hope for children with hepatoblastoma.
References:
- Djouder, N., & Rigual, M. del Mar. (2025). CNIO researchers discover a new mechanism for rapid liver regeneration triggered by glutamate. Nature. https://www.cnio.es/en/news/cnio-researchers-discover-a-new-mechanism-for-rapid-liver-regeneration-triggered-by-glutamate/