Hepatoblastoma is a rare liver cancer that mainly hits young kids, often in the first two years. A surprising fact is that it’s the most common liver cancer in kids. This makes it a big worry for parents and doctors.
To understand hepatoblastoma, we need to look at genetics and the environment. Studying this rare cancer is key to finding better treatments and helping kids get better.
Exploring hepatoblastoma shows it’s a complex issue. We’ll look at the different things that can lead to this disease.
Defining liver scarring (cirrhosis) and listing common Hepatoblastoma symptoms in children.
Key Takeaways
- Understanding hepatoblastoma requires knowledge of its genetic and environmental factors.
- Hepatoblastoma is the most common liver cancer in children under the age of three.
- Research into the causes of hepatoblastoma is vital for finding effective treatments.
- Spotting liver cancer signs early can greatly improve a child’s chances.
- Kids with a family history of certain genetic conditions might be at higher risk.
Understanding Hepatoblastoma: A Rare Pediatric Liver Cancer
It’s important to know about hepatoblastoma to catch it early and treat it well. We’ll look at what it is, how common it is, its types, and how it’s classified. This will give you a full picture.
Definition and Prevalence in Children
Hepatoblastoma is a cancer that starts in the liver. It’s mostly found in kids under three. It’s the top liver cancer in kids, but it’s rare. About 1.2 to 1.5 kids under 15 get it every million.
Key statistics on hepatoblastoma prevalence include:
- Accounts for about 1% of all pediatric cancers
- Most common liver cancer in children under 3 years old
- Increased incidence in children with certain genetic syndromes
Types and Classification of Hepatoblastoma
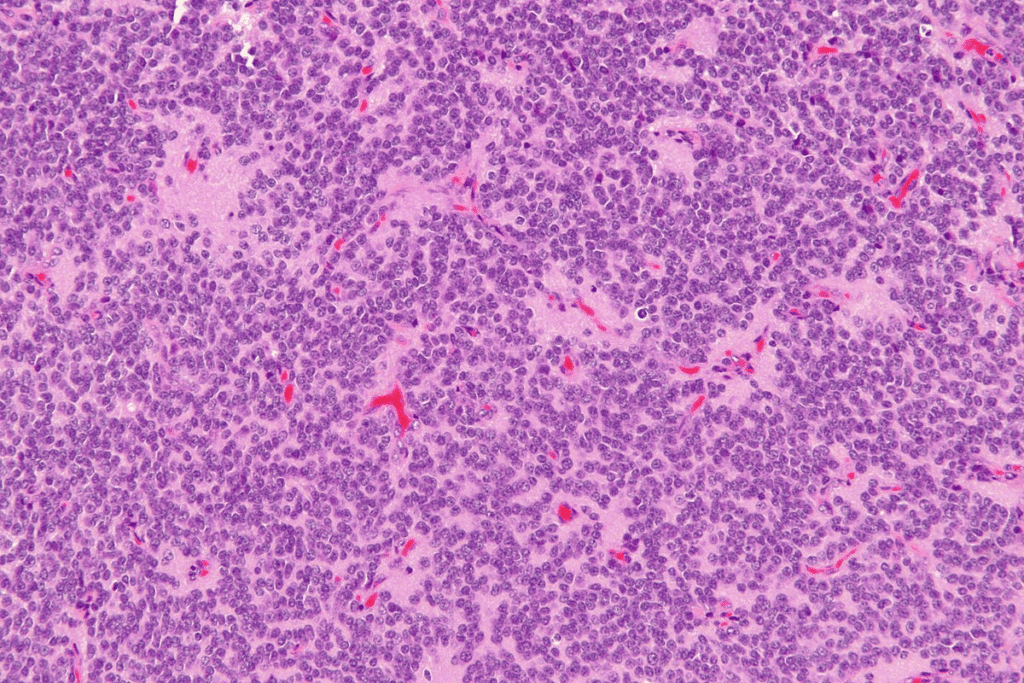
Hepatoblastoma has different types based on how it looks under a microscope. The main types are:
- Epithelial type: This breaks down into fetal and embryonal subtypes
- Mixed epithelial and mesenchymal type: It has both epithelial and mesenchymal parts
Knowing the exact type of hepatoblastoma is key for figuring out the treatment. The PRETEXT staging system helps figure out how big the tumor is. This guides how to treat it.
Early signs of hepatoblastoma include a big tummy, not wanting to eat, and losing weight. Doctors use imaging, blood tests, and biopsies to diagnose it. Knowing about the types and how to classify them is vital for managing and treating the disease.
The Genetic Basis of Hepatoblastoma

Exploring the genetic roots of hepatoblastoma shows a complex mix of chromosomal and gene changes. This rare liver cancer mainly hits young kids and babies. Knowing the genetic causes helps us understand the disease better and might lead to new treatments.
Chromosomal Abnormalities
Chromosomal issues are key in hepatoblastoma’s development. Some genetic syndromes and changes in chromosomes raise the risk of this cancer. For example, trisomy 18 and other chromosomal problems have been linked to hepatoblastoma. These issues can disrupt normal cell control, possibly causing tumors.
Also, kids with familial adenomatous polyposis (FAP) face a higher risk of getting hepatoblastoma. FAP causes many polyps in the colon due to APC gene mutations. This link shows how genetics play a big role in the disease.
Gene Mutations Associated with Liver Tumor Development
Some genes are more likely to be mutated in hepatoblastoma. The CTNNB1 gene, which codes for β-catenin, is often changed in these tumors. These changes can turn on the Wnt/β-catenin pathway, making cells grow and tumors grow.
Other genetic changes in different pathways might also start and grow hepatoblastoma. Learning about these genetic shifts helps us understand the disease’s molecular roots. It also guides us in finding new treatments.
Studying the genetics of hepatoblastoma helps us understand this cancer better. It also helps in managing and treating young patients. As we learn more about the genetic causes, we get closer to better outcomes for those with this tough disease.
Risk Factors for Developing Hepatoblastoma
Hepatoblastoma can be caused by several prenatal and perinatal factors. Knowing these risk factors is key for early detection and prevention. We will look at the main factors that increase the risk of this rare liver cancer in children.
Premature Birth and Low Birth Weight
Studies show that premature birth and low birth weight raise the risk of hepatoblastoma. Kids born early or with low weight are more likely to get this cancer. Spotting hepatoblastoma symptoms early in these high-risk children is vital for timely treatment.
Research links lower birth weights with a higher risk of hepatoblastoma. This shows why it’s important to watch children with low birth weight for early signs of liver tumors.
Familial Adenomatous Polyposis (FAP)
Familial Adenomatous Polyposis (FAP) is a genetic condition that leads to many polyps in the colon. It also raises the risk of hepatoblastoma. Families with FAP history should be aware of the risk of liver cancer in their kids.
The gene causing FAP can make kids more likely to get cancers, including hepatoblastoma. Families with FAP should get genetic tests and watch for signs early.
Other Genetic Syndromes and Predispositions
Other genetic syndromes, like Beckwith-Wiedemann syndrome, also increase the risk of hepatoblastoma. Kids with these conditions need regular checks for liver cancer signs.
Knowing about genetic risks and watching for symptoms can help catch hepatoblastoma early. Families with genetic syndromes should talk to doctors about how to watch for signs.
Environmental and Maternal Factors
Recent studies have shown how environmental exposures and maternal health during pregnancy might affect the risk of hepatoblastoma. This rare liver cancer in kids is influenced by both genetic and environmental factors.
Parental Exposures to Toxins
Research has looked into how toxins affect parents and their children. Occupational exposures to chemicals like solvents, pesticides, and heavy metals are being studied. These chemicals might increase the risk of liver tumors in kids.
Mitophagy, a process that removes damaged mitochondria, is also being studied. It’s thought to play a role in how toxins affect cancer development. Scientists are looking into how toxins impact mitophagy and hepatoblastoma.
| Toxin | Potential Impact | Study Findings |
| Solvents | Increased risk of liver cancer | Some studies suggest a link between paternal solvent exposure and increased risk of hepatoblastoma in children. |
| Pesticides | Possible carcinogenic effects | Research is ongoing to determine if there’s a direct link between pesticide exposure and hepatoblastoma. |
| Heavy Metals | Cancer risk due to bioaccumulation | Some heavy metals have been associated with an increased risk of various cancers, including potentially hepatoblastoma. |
Maternal Health Conditions During Pregnancy
Maternal health during pregnancy is also being studied. Conditions like pre-eclampsia, gestational diabetes, and infections are being looked at. They might affect the risk of hepatoblastoma in kids.
Maternal nutrition and health behaviors, like smoking or drinking, are also being studied. These factors could influence liver tumor development in children. Knowing this can help find ways to prevent hepatoblastoma and improve outcomes for at-risk kids.
Hepatoblastoma Symptoms: What Parents Need to Know
It’s key for parents to know the symptoms of hepatoblastoma to get their child the right care fast. This rare liver cancer mainly hits kids and can be tricky to spot early because its symptoms are not clear-cut.
Abdominal Signs and Discomfort
One big sign of hepatoblastoma is when a child’s belly gets bigger. This can hurt or feel off. You might see their belly looks bigger than usual, or they might say their tummy hurts.
- Abdominal swelling or distension
- Pain or discomfort in the abdomen
- Loss of appetite
Systemic Manifestations
Hepatoblastoma can also show up in other ways. These signs include:
- Weight loss or not gaining weight like they should
- Fever
- Fatigue or feeling really tired
These signs can look like other common kid illnesses. So, it’s very important to see a doctor if you’re worried.
Late-Stage Clinical Presentations
Sometimes, hepatoblastoma is found when it’s already grown a lot. Signs of this include:
- Jaundice (yellowing of the skin and eyes)
- Severe abdominal pain
- Vomiting
If doctors think a child might have hepatoblastoma, they’ll do lots of tests. This helps figure out how far the cancer has spread and what treatment to use.
We really stress how important it is to catch and treat hepatoblastoma early. Knowing the signs and acting fast can help a lot. Parents are a big part of their child’s care.
Early Signs of Hepatoblastoma in Infants and Children
It’s important to spot the early signs of hepatoblastoma in young ones. This rare liver cancer mainly hits kids, and catching it early can make a big difference in treatment success.
Physical Changes to Watch For
One key sign is an abnormal swelling in the belly. This swelling is often due to a growing tumor. Parents might see their child’s belly looks bigger or feels hard when touched.
Key physical changes include:
- Abdominal swelling or distension
- A palpable mass in the abdomen
- Weight loss or failure to gain weight at a normal rate
Behavioral and Appetite Changes
Children with hepatoblastoma might also show behavioral and appetite changes. These signs can be small but important:
- Loss of appetite
- Irritability or lethargy
- Changes in energy levels
Parents should watch for these signs and talk to a doctor if they’re worried.
Knowing these early signs can lead to quicker detection and treatment of hepatoblastoma. If you see any unusual changes in your child, get medical help right away.
| Signs | Description |
| Abdominal Swelling | Noticeable enlargement or distension of the abdomen due to the tumor. |
| Palpable Mass | A mass can be felt in the abdomen upon examination. |
| Loss of Appetite | Children may show less interest in feeding or eating. |
The Diagnostic Journey for Pediatric Liver Cancer
Diagnosing hepatoblastoma involves a few key steps. We use physical exams, lab tests, and imaging studies. Understanding liver cancer in kids is complex.
Initial Assessment and Physical Examination
The first step is a detailed physical exam and initial check-up. We look for signs like an enlarged belly, which might mean a liver tumor. The child’s past health is also important, as some conditions raise the risk of hepatoblastoma.
During the exam, we check for any unusual findings in the belly. Finding a mass could mean a liver tumor, leading to more tests.
Blood Tests and Tumor Markers (Alpha-fetoprotein)
Blood tests are key in diagnosing hepatoblastoma. We check for alpha-fetoprotein (AFP), a marker often high in kids with this cancer. High AFP levels help us see if the disease is present or growing.
The table below shows how AFP levels help diagnose and track hepatoblastoma:
| AFP Level | Interpretation |
| Normal | Typically indicates absence of hepatoblastoma or successful treatment |
| Elevated | May indicate presence of hepatoblastoma or other conditions |
| Very High | Often associated with hepatoblastoma, requires further investigation |
Advanced Imaging Studies
Advanced imaging is vital for diagnosing and understanding hepatoblastoma. Ultrasound, CT scans, and MRI give us detailed liver images. They help us see how big the tumor is and if it has spread.
A study in a medical journal says imaging is key for managing pediatric liver tumors. It helps us know how far the disease has spread and what treatment to choose.
“Imaging plays a critical role in the diagnosis and management of pediatric liver tumors.”
These studies show us the tumor’s size, where it is, and if it has spread. This info is essential for planning the best treatment.
Biopsy and Staging of Childhood Liver Tumors
Biopsy is key in diagnosing hepatoblastoma. It gives vital info about the tumor. If a child is thought to have liver cancer, a biopsy is done. It confirms the diagnosis and shows the tumor’s details.
Biopsy Procedures and Techniques
A biopsy takes a tumor tissue sample for study. There are several ways to do a biopsy:
- Needle biopsy, where a thin needle collects tissue.
- Surgical biopsy, where a part of the tumor is removed surgically.
These methods help figure out the tumor type and how aggressive it is. This info is key for treatment planning.
Understanding the PRETEXT Staging System
After diagnosis, the tumor is staged with the PRETEXT system. PRETEXT stands for PRE-Treatment EXTent of disease. It’s a system for liver tumors in kids.
The PRETEXT system looks at the liver in four sectors. It checks how many sectors the tumor involves. This info is vital for knowing the disease extent and treatment planning.
| PRETEXT Stage | Description |
| I | One sector involved, three adjoining sectors free |
| II | Two sectors involved, two adjoining sectors free |
| III | Three sectors involved, one sector free or two non-adjoining sectors free |
| IV | All four sectors involved |
Knowing the PRETEXT stage helps doctors predict the outcome. It helps choose the best treatment for kids with hepatoblastoma.
Treatment Approaches for Hepatoblastoma
Dealing with hepatoblastoma needs a team effort. This includes surgery, chemotherapy, and sometimes liver transplant. The right treatment depends on the disease stage, the child’s health, and more.
Surgical Resection Options
Surgery is key in treating hepatoblastoma. The goal is to remove the tumor fully. Complete surgical resection is tough due to tumor size and location but is vital for survival.
When planning surgery, we look at the tumor size and the child’s liver health. New surgical methods have helped improve outcomes for kids with this disease.
Chemotherapy Protocols and Regimens
Chemotherapy is also essential in treating hepatoblastoma. It’s used alone or with surgery. Cisplatin-based chemotherapy is often used, along with doxorubicin.
| Chemotherapy Regimen | Agents Used | Typical Use |
| Cisplatin-based | Cisplatin, Doxorubicin | Primary chemotherapy for hepatoblastoma |
| Alternative Regimens | Various combinations | For patients who cannot tolerate cisplatin |
Liver Transplantation Considerations
When the tumor can’t be removed or has spread, liver transplantation might be an option. This choice is made based on the disease extent and the child’s health.
We weigh the benefits and risks of liver transplant. This includes the need for lifelong drugs to prevent rejection and the chance of cancer coming back.
It’s important for families to know about the different treatments for hepatoblastoma. By using surgery, chemotherapy, and sometimes liver transplant, we can create a treatment plan that fits each child’s needs.
Innovative Therapies and Clinical Trials for Pediatric Liver Cancer
New treatments, like targeted molecular therapies and immunotherapy, are being tested to help kids with liver cancer. We’re learning more about hepatoblastoma, a rare liver cancer in kids. This means we need better, less harsh treatments.
Targeted Molecular Therapies
Targeted molecular therapies are a big step forward in treating liver cancer in kids. They aim to hit cancer cells directly, sparing healthy ones. This could lead to fewer side effects and better survival rates.
Scientists are focusing on finding genetic flaws in hepatoblastoma. By pinpointing these, they can create drugs that target them. This could lead to more effective treatments.
Immunotherapy Approaches and Developments
Immunotherapy uses the body’s immune system to fight cancer. It’s being studied for treating liver cancer in kids. This method has shown promise in other cancers too.
Immunotherapy includes different types, like checkpoint inhibitors and CAR-T cell therapy. These are being tested in clinical trials to see if they work for kids with hepatoblastoma.
By combining these new therapies, we might see better results for kids with liver cancer. Ongoing research and trials are key to finding the best treatments. This way, kids can get the care they need.
Long-term Prognosis and Survival Rates
The long-term outlook for kids with hepatoblastoma depends on several important factors. Knowing these factors helps families and doctors plan the treatment journey better.
Factors Affecting Treatment Outcomes
Several factors impact the long-term outlook for children with hepatoblastoma. These include:
- Stage at Diagnosis: The extent of the disease at diagnosis is key to the prognosis.
- Response to Treatment: The child’s response to initial treatment greatly affects the long-term outlook.
- Tumor Biology: The genetic makeup of the tumor can influence treatment outcomes.
- Age and Overall Health: The child’s age and health at diagnosis also play a role in prognosis.
Long-term Monitoring and Follow-up Care
Long-term follow-up care is vital for managing treatment side effects and watching for recurrence. This includes:
- Regular imaging studies to check for tumor return.
- Blood tests to track tumor markers, like alpha-fetoprotein.
- Monitoring for late effects of chemotherapy and other treatments.
Understanding the factors that affect long-term prognosis and following a detailed follow-up care plan helps families face the challenges of hepatoblastoma treatment.
Coping with a Hepatoblastoma Diagnosis
When a family finds out about hepatoblastoma, they face a lot of emotions and challenges. It’s important for them to have a strong support system. This helps them deal with the news.
Resources and Support for Families
Families need help in many ways after a hepatoblastoma diagnosis. They need medical advice, emotional support, and help with everyday tasks. Many organizations and healthcare providers offer these services.
Some key resources include:
- Support groups for families and patients
- Access to counseling and psychological services
- Educational materials about hepatoblastoma and its treatment
- Financial assistance programs for families dealing with medical expenses
One parent said in a support group, “Getting a hepatoblastoma diagnosis felt like being in a storm. But with the right support, we got through it together.”
“The support from the hospital and support groups really helped us cope with the diagnosis.”
Psychological Support for Children and Parents
Psychological support is key for kids with hepatoblastoma and their parents. The news and treatment can deeply affect everyone’s mental health. It’s important to help the whole family.
| Support Type | Description | Benefit |
| Counseling | One-on-one or group therapy sessions | Emotional support and coping strategies |
| Support Groups | Group meetings for families and patients | Shared experiences and community |
| Educational Programs | Programs educating about hepatoblastoma | Understanding and empowerment |
We know how important it is to offer care that meets all family needs. By providing a wide range of support, we help families on their tough journey.
Prevention Strategies and Future Research Directions
Right now, we don’t have many ways to prevent hepatoblastoma. But, research is moving forward. It’s important to learn about the genetic and environmental causes of this disease. This knowledge can help us find ways to prevent it.
Potential Preventive Measures
We don’t have any proven ways to stop hepatoblastoma yet. But, scientists are studying the genetic and environmental factors that might cause it. They think things like being born too early or being underweight might increase the risk.
To find ways to prevent it, researchers are doing a lot of studies. Screening high-risk babies early could help improve their chances of survival.
Emerging Research and Clinical Advances
New research is trying to understand the disease at a molecular level. Thanks to genetic sequencing and molecular biology, scientists can find specific genetic changes linked to hepatoblastoma. This is key for creating targeted treatments and maybe even prevention methods.
Clinical trials are testing new treatments. For example, targeted molecular therapies and immunotherapy are being looked at for treating hepatoblastoma. These new treatments not only help patients but also help us learn more about preventing the disease.
| Research Area | Potential Impact |
| Genetic Sequencing | Identification of genetic mutations for targeted therapies |
| Molecular Biology Advances | Understanding molecular mechanisms for preventive strategies |
| Clinical Trials | Evaluation of new treatment protocols and therapies |
As we learn more about hepatoblastoma, we might find new ways to prevent it. Using research in real-world treatments is key to helping kids with this rare liver cancer.
Conclusion
Understanding hepatoblastoma, a rare and complex pediatric liver cancer, is key to improving outcomes for kids. We’ve looked at the genetic and environmental factors that lead to it. This includes symptoms and signs of pediatric liver cancer.
Early detection and diagnosis are vital. They involve various diagnostic tools and techniques. These help find the best liver cancer treatment options.
Treatment methods range from surgery and chemotherapy to liver transplantation. Often, these are used together. As research grows, new therapies and clinical trials offer hope for kids with hepatoblastoma.
By keeping up with the latest in liver cancer treatment, families and healthcare providers can give the best care. This teamwork is essential for helping children with this disease.
FAQ
What is hepatoblastoma and how common is it in children?
Hepatoblastoma is a rare liver cancer in kids. It’s usually found in the first two years of life. The exact cause is being researched.
What are the risk factors for developing hepatoblastoma?
Risk factors include being born early, being underweight, and having certain genetic syndromes. Knowing these can help catch it early.
What are the symptoms of hepatoblastoma that parents should be aware of?
Look out for swelling or pain in the belly. Babies and young kids might act differently or show physical signs.
How is hepatoblastoma diagnosed?
Doctors use a physical check, blood tests, imaging, and a biopsy to diagnose. The PRETEXT system helps classify the disease.
What are the treatment options for hepatoblastoma?
Treatment includes surgery, chemotherapy, and sometimes liver transplant. New treatments like targeted therapies are being tested.
What is the long-term prognosis for children with hepatoblastoma?
The outlook depends on treatment success. Regular follow-ups are key for managing long-term effects.
How can families cope with a hepatoblastoma diagnosis?
Families need support, resources, and counseling. It’s important to help both kids and parents.
Are there any preventive measures for hepatoblastoma?
Not yet, but research is ongoing. It might find ways to prevent it in the future.
What is the role of genetic factors in hepatoblastoma development?
Genetics are key, with some mutations raising the risk. Studying these can help understand the disease.
How do environmental and maternal factors influence hepatoblastoma risk?
Pregnancy and environmental factors might also affect risk. Research into these areas is ongoing.
National Center for Biotechnology Information. Hepatoblastoma etiology genetics and treatment directions. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8335155/
National Center for Biotechnology Information. Hepatoblastoma etiology a common pediatric hepatic malignancy. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8335155/
Nature. Hepatoblastoma etiology incidence genetics and future treatments. Retrieved from https://www.nature.com/articles/s41467-021-25430-9
ScienceDirect. Hepatoblastoma etiology genetics and environmental factors. Retrieved from https://www.sciencedirect.com/science/article/pii/S1043661811000751
References
Benoist, M. (2002). The natural history of lumbar degenerative spinal stenosis: A comprehensive review. Joint Bone Spine, 69(5), 450-457. https://www.sciencedirect.com/science/article/abs/pii/S1297319X02004293




































