Last Updated on November 4, 2025 by mcelik

Herniated disc surgery last resort is a term used when all other treatment options have been tried and failed. A herniated disc occurs when the gel-like cushion between vertebrae slips out, putting pressure on nearby nerves, which can cause pain, numbness, and weakness.
Millions of Americans suffer from herniated discs, with symptoms ranging from mild to severe. Some patients find relief through non-surgical treatments, while others may require surgery.
Surgery is typically recommended only when conservative treatments fail to relieve symptoms or if nerve damage is progressing. Understanding when herniated disc surgery is a last resort helps patients make informed decisions about their care.
Key Takeaways
- Herniated discs can cause significant pain and discomfort.
- Non-surgical treatments are often the first line of treatment.
- Surgery may be considered for severe or persistent symptoms.
- Understanding the available treatment options is key.
- Talking to a healthcare professional about surgery is important.
Understanding Herniated Discs: Causes and Symptoms
Knowing about herniated discs is key to managing them well. A herniated disc, also called a slipped or ruptured disc, affects the spine. It leads to symptoms that can really hurt your quality of life.
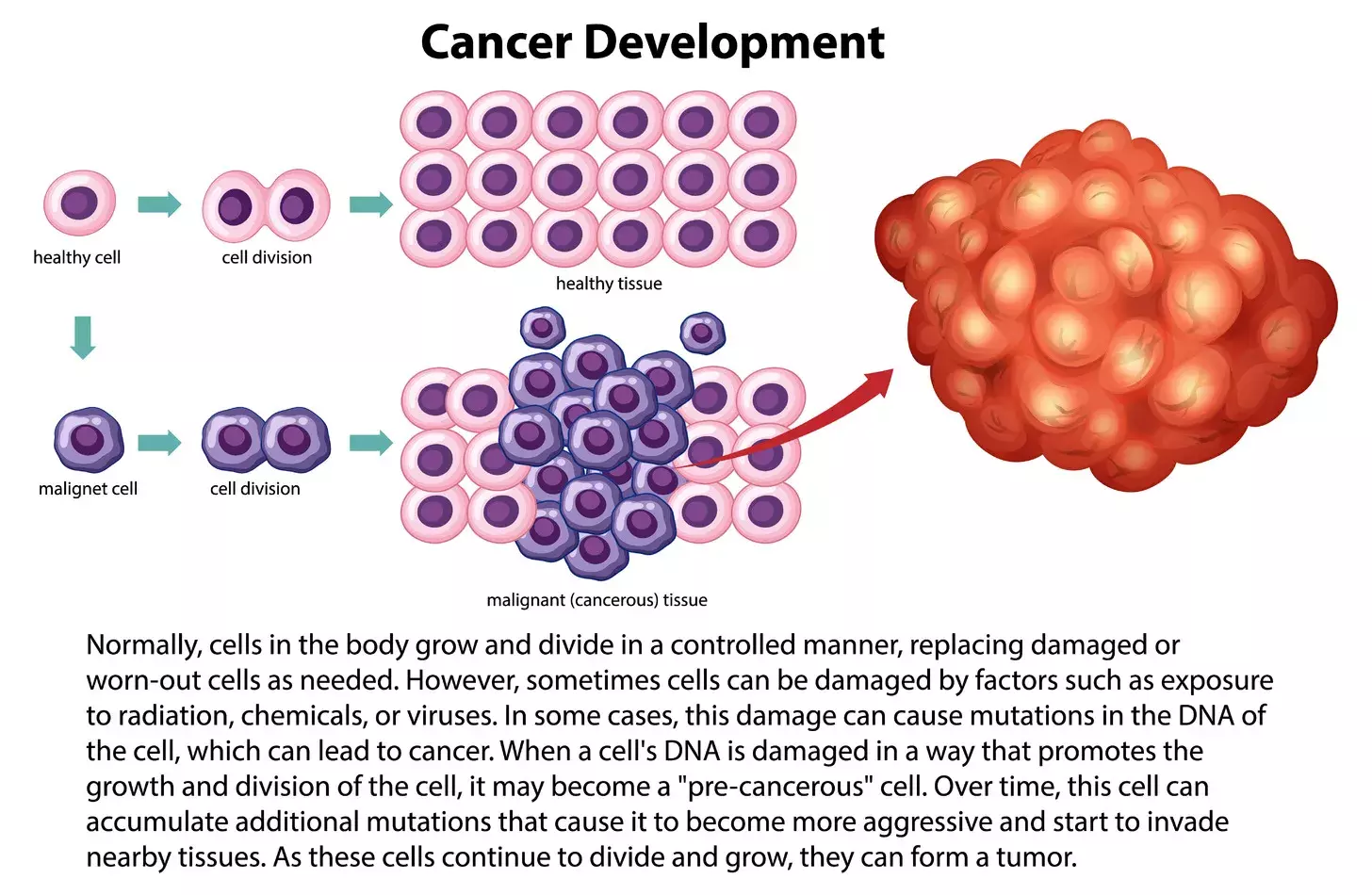
What Happens When a Disc Herniates
A herniated disc happens when the soft inner gel leaks out through a tear. This can irritate nerves, causing pain, numbness, or weakness in the back or legs. It can happen due to age, injury, or strain.
Herniation is a complex process. As we age, our discs lose water and become more likely to tear. When a tear happens, the inner gel can leak out, pressing on nerves.
Common Symptoms of Herniated Discs
The symptoms of a herniated disc vary. They depend on where the herniation is, how big it is, and if it’s pressing on a nerve. Common symptoms include:
- Back pain that can range from mild to severe
- Numbness or tingling sensations in the extremities
- Muscle weakness in the affected area
- Pain that radiates to the arms or legs, depending on the location of the herniated disc
In some cases, a herniated disc can cause more severe symptoms. These include significant muscle weakness or loss of bladder/bowel control. These need immediate medical attention.
Risk Factors for Developing Herniated Discs
Several factors can increase the risk of getting a herniated disc. These include:
- Age: The risk goes up with age because of spinal disc degeneration.
- Physical activity: Jobs or activities that involve heavy lifting, bending, or twisting can increase the risk.
- Genetics: A family history of herniated discs can make you more likely to get one.
- Smoking: Smoking can reduce oxygen to the discs, speeding up degeneration.
- Obesity: Being overweight can put extra strain on the spine.
Knowing these risk factors can help you prevent herniated discs. It also helps you seek early treatment if symptoms show up.
Diagnosing a Herniated Disc: The Path to Treatment

To find out if you have a herniated disc, doctors use several methods. They check your body, ask about your health history, and use special imaging. This way, they can make sure they know what’s wrong and how to fix it.
Physical Examination Techniques
First, doctors do a physical check-up. They see how well you can move and if it hurts. They also do tests like the straight leg raise to see if nerves are being squeezed.
They also check your nerves by looking at muscle strength, reflexes, and how you feel things. This helps them see if the disc is hurting your nerves.
Imaging Studies: MRI, CT Scans, and X-rays
Imaging tests are key to confirming a herniated disc. Magnetic Resonance Imaging (MRI) is top choice because it shows soft tissues well, like discs and nerves.
Computed Tomography (CT) scans are used when MRI can’t be done. They show the bones of the spine. X-rays help check for other problems like fractures or tumors, but they’re not as good for discs.
Neurological Tests and Their Significance
Neurological tests are important to see how a herniated disc affects your nerves. They check muscle strength, reflexes, and sensation. If these tests show problems, it means nerves might be hurt or squished.
For example, if you have a herniated disc, you might have weak muscles or feel numbness. These signs help doctors know where the problem is and how to treat it.
The Conservative Treatment Approach
The conservative treatment approach is a strategy to manage herniated disc symptoms without surgery. It’s less invasive and can be very effective. It helps reduce pain and improve function.
Rest and Activity Modification
Resting the affected area and modifying activities are key steps. Avoid heavy lifting, bending, or twisting. This allows the spine to heal and can bring significant pain relief.
It’s important to find a balance between rest and activity. This prevents stiffness and promotes healing.
Over-the-Counter Pain Medications
OTC pain medications like ibuprofen or acetaminophen are often recommended. They help manage pain and inflammation from herniated discs. These medications allow people to keep up with their daily activities.
“Using OTC pain relievers is a simple and effective way to manage herniated disc pain. It’s important to follow the recommended dosage to avoid side effects.”
-As advised by professionals.
Heat and Cold Therapy
Applying heat or cold to the affected area can help manage pain. Cold therapy, like an ice pack, reduces inflammation. Heat therapy, such as a warm bath or heating pad, relaxes muscles and improves blood flow.
Switching between heat and cold therapy can offer the best relief, depending on how you respond.
Lifestyle Adjustments for Pain Management
Making lifestyle changes is important for managing pain and preventing future episodes. This includes staying at a healthy weight, improving posture, and exercising regularly. Regular exercise strengthens back muscles and improves flexibility.
- Maintaining a healthy weight reduces strain on the spine.
- Improving posture helps distribute weight evenly.
- Regular exercise strengthens muscles that support the spine.
By using these conservative treatment methods, many people find relief from herniated disc symptoms. They can also improve their overall quality of life.
Physical Therapy for Herniated Discs
Physical therapy is key in treating herniated discs. It’s a non-invasive way to ease pain and improve function. Physical therapists use various techniques to help patients manage their symptoms and live better lives.
Core Strengthening Exercises
Core strengthening is a big part of herniated disc treatment. Exercises that target the abdominal and back muscles help stabilize the spine. This reduces strain on the herniated disc and surrounding areas.
Examples of these exercises include:
- Planks
- Bridges
- Pelvic tilts
These exercises aid in recovery and also help prevent future herniations.
Flexibility and Stretching Programs
Flexibility and stretching exercises improve range of motion and reduce stiffness. Techniques like hamstring stretching and knee to chest stretches help ease tension on the lower back. This provides relief from herniated disc symptoms.
| Stretching Exercise | Benefit |
| Hamstring Stretch | Reduces tension on the lower back |
| Knee to Chest Stretch | Relieves pressure on the spine |
Manual Therapy Techniques
Manual therapy involves hands-on techniques used by physical therapists. Methods like massage, joint mobilization, and soft tissue mobilization help reduce pain and inflammation. They also improve circulation and promote healing.
McKenzie Method and Other Specialized Approaches
The McKenzie Method is a specialized approach for spinal disorders, including herniated discs. It uses specific exercises and techniques tailored to each individual. The goal is to reduce pain and improve spinal mechanics.
By using these physical therapy methods, people with herniated discs can see big improvements in their symptoms and spinal health.
Pain Management Strategies for Herniated Discs
Managing pain from herniated discs needs a mix of treatments. It’s key to improve life quality for those with this condition.
Prescription Medications
Prescription medications are often used to manage herniated disc pain. They can include muscle relaxants, oral steroids, or stronger pain relievers for severe cases.
The right medication depends on the pain level, health history, and any health issues. It’s important for patients to talk with their doctor to find the best treatment with minimal side effects.
Epidural Steroid Injections
Epidural steroid injections are a helpful pain management option for herniated discs. They put corticosteroids near the spinal cord to reduce inflammation and pain.
These injections are often used when other treatments don’t work well enough.
Nerve Blocks and Other Interventional Procedures
Nerve blocks and other procedures might be suggested for some patients. Nerve blocks inject medication around nerves to block pain signals.
Other procedures like radiofrequency ablation or spinal cord stimulation can help with chronic pain that other treatments can’t manage.
| Pain Management Strategy | Description | Benefits |
| Prescription Medications | Muscle relaxants, oral steroids, pain relievers | Effective for managing pain and inflammation |
| Epidural Steroid Injections | Corticosteroids injected into epidural space | Reduces inflammation, relieves pain |
| Nerve Blocks | Medication injected into or around nerves | Prevents pain signals to the brain |
Alternative and Complementary Treatments
There are many alternative and complementary treatments for herniated discs. These methods can work alongside traditional treatments to help manage symptoms.
Chiropractic Care
Chiropractic care focuses on spinal adjustments to improve alignment and reduce disc pressure. Many people find relief from their herniated disc symptoms through regular chiropractic visits.
Acupuncture
Acupuncture is an ancient method that uses thin needles to stimulate healing and pain relief. Some studies show it can help manage chronic pain from herniated discs.
- Stimulates natural pain-relieving chemicals
- Enhances blood flow to affected areas
- Promotes relaxation and reduces stress
Massage Therapy
Massage therapy can ease muscle tension around the spine, helping to reduce discomfort from herniated discs. Deep tissue massage and myofascial release are common techniques used.
| Therapy Type | Benefits |
| Deep Tissue Massage | Relieves muscle tension, improves circulation |
| Myofascial Release | Reduces scar tissue, improves flexibility |
Yoga and Pilates for Spinal Health
Yoga and Pilates can help with spinal health by strengthening core muscles and improving flexibility. They can also help with posture. Certain exercises are great for people with herniated discs.
It’s important for people with herniated discs to talk to healthcare professionals before trying new therapies or exercises. This ensures they’re safe and right for their condition.
When Conservative Treatments Fail: Decision Points
If treatments for a herniated disc don’t work, it’s time to think about other options. Patients and doctors need to decide what to do next to manage the condition well.
Persistent Pain Despite Treatment
Persistent pain after trying different treatments is a big sign that something needs to change. This pain can make everyday tasks hard, so it’s important to look at other ways to treat it.
People with ongoing pain might need more tests to find out why they’re feeling this way. Doctors might use special scans or tests to see how serious the nerve damage is.
Progressive Neurological Symptoms
Progressive neurological symptoms mean you need to see a doctor right away. Signs like numbness, weakness, or tingling in your limbs could mean your nerves are getting worse.
Seeing a doctor quickly is key if you’re noticing these symptoms. Sometimes, surgery is needed to stop nerve damage from getting worse.
Red Flags That Indicate Urgent Surgical Evaluation
Some red flags mean you need to see a surgeon fast. These include big problems like weakness or paralysis, and cauda equina syndrome. This is when you lose feeling in your legs and have trouble with your bowels or bladder.
If you see these signs, get help right away. Surgery can help prevent lasting damage and improve your health.
Is Herniated Disc Surgery a Last Resort?
Herniated disc surgery is often seen as a last option. But what does this really mean today? With new surgical methods and technology, the view on surgery has changed a lot.
The Evolution of Surgical Approaches
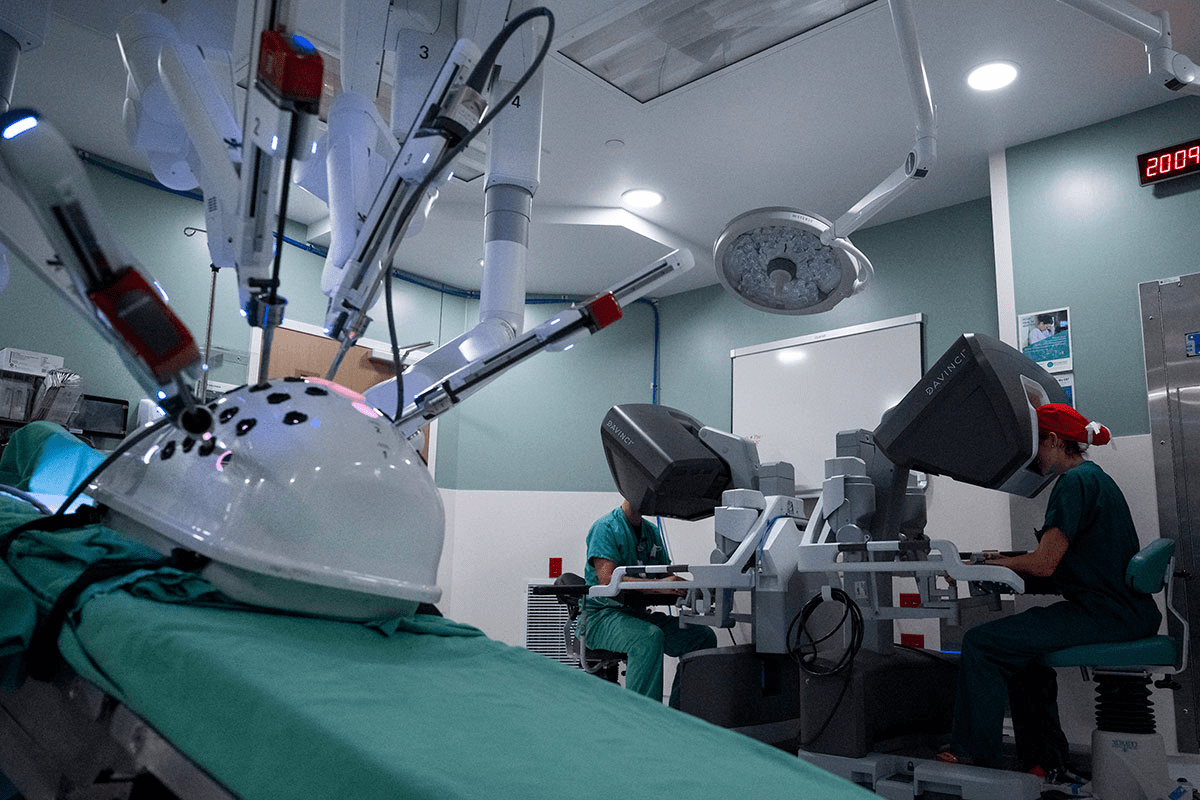
Surgeries for herniated discs have gotten better. Minimally invasive procedures now offer safer and more effective ways to treat patients. They help patients recover faster and reduce the chance of complications.
New techniques like endoscopic discectomy and tubular microdiscectomy are making treatments less invasive. This means patients can get back to their normal lives sooner.
Current Medical Consensus
Doctors now think surgery should be considered when other treatments don’t work. Shared decision-making between doctors and patients is key. It helps create treatment plans that fit each person’s needs.
Patient-Specific Considerations
Every patient’s situation is different when it comes to surgery. Factors like how bad the symptoms are, the patient’s overall health, and any neurological issues are important. Personalized treatment plans are vital to meet each patient’s unique needs.
The Concept of “Last Resort” in Modern Spine Care
The idea of surgery as a “last resort” is changing in spine care today. New surgical methods and technology make surgery a more viable option sooner for some patients.
Whether or not to have herniated disc surgery depends on a detailed look at the patient’s condition. It also depends on a thorough talk between the patient and their doctor.
Surgical Options for Herniated Discs
When other treatments don’t work, surgery might be needed for herniated discs. Surgery aims to ease pressure on nerves and stabilize the spine.
Microdiscectomy
Microdiscectomy is a small surgery to remove the herniated part of the disc. It’s chosen often because it works well and recovery is quick.
Laminectomy
A laminectomy removes part of the vertebrae to make room for nerves. It’s used for severe spinal stenosis or when a herniated disc presses hard on nerves.
Spinal Fusion
Spinal fusion joins two or more vertebrae together with bone grafts and hardware. It stabilizes the spine and can reduce pain. But, it takes longer to recover and is for more serious cases.
Artificial Disc Replacement
Artificial disc replacement swaps the damaged disc with an artificial one. It tries to keep the spine mobile and reduce pain. It’s for those with serious disc problems.
Each surgery has its own reasons, benefits, and risks. The right surgery depends on the herniation’s severity, the patient’s health, and the doctor’s advice.
Minimally Invasive Spine Surgery: A Game Changer?
The arrival of minimally invasive spine surgery has changed how we treat herniated discs. It’s a new way to fix problems without the big cuts of old surgeries. This method is getting a lot of attention because it might help people heal faster and with less pain.
Endoscopic Discectomy
Endoscopic discectomy uses a special camera to see inside the body. It lets doctors take out the bad disc without hurting too much of the surrounding tissue.
Tubular Microdiscectomy
Tubular microdiscectomy uses a small tube to get to the disc. It’s done with a tiny cut, which means less damage and a quicker recovery for the patient.
Advantages Over Traditional Open Surgery
Minimally invasive spine surgery has big benefits. It means smaller cuts, less blood loss, and a quicker recovery. These perks make the healing process easier and faster for patients.
- Smaller incisions result in less tissue damage and scarring.
- Reduced risk of infection due to less invasive nature.
- Less post-operative pain and discomfort.
- Faster return to normal activities.
Technological Advancements in Spine Surgery
Spine surgery has seen big tech improvements. Better imaging and tools make these new surgeries safer and more precise. This makes them a good choice for many patients.
As tech keeps getting better, minimally invasive spine surgery will play a bigger role in spinal care. It promises to offer better and faster ways to treat spinal problems.
Weighing the Risks and Benefits of Herniated Disc Surgery
It’s important to know the risks and benefits of herniated disc surgery. This helps you make a smart choice about treatment. Surgery can help many people, but it also has risks and long-term effects.
Potential Complications
Herniated disc surgery has risks, like any surgery. Complications can include infection, nerve damage, and bleeding. Sometimes, the surgery might not solve the problem or could cause new issues.
Infection is a risk with any surgery. Doctors do their best to prevent it, but it’s something to think about.
Nerve damage is another risk. It can cause numbness, weakness, or ongoing pain. The chance of this happening depends on the surgery and the patient.
Long-Term Considerations
It’s also key to think about the long-term effects of herniated disc surgery. This includes the chance of the problem coming back or new issues at other levels.
- Recurrence of herniation at the same level
- Degenerative changes at adjacent levels
- Instability or chronic pain
Knowing these possibilities helps set realistic goals for recovery and long-term health.
Risk Factors That May Affect Surgical Outcomes
Some things can change how well herniated disc surgery works. These include the patient’s health, age, and lifestyle, like smoking or being overweight.
For example, smoking can slow healing and raise the risk of problems. Being very overweight can also stress the spine, affecting the surgery’s success.
Healthcare providers can give better advice by considering these factors. They can help patients understand the risks and benefits based on their own situation.
Recovery After Herniated Disc Surgery
Recovering from herniated disc surgery takes time, effort, and a good plan. It involves taking care of yourself right after surgery, slowly getting back to normal, and keeping up with maintenance to avoid future problems.
Immediate Post-Operative Period
The first few days after surgery are very important. Patients usually stay in the hospital for a few hours or overnight. Medical staff help manage pain, watch for complications, and teach how to care for yourself after surgery.
Key aspects of immediate post-operative care include:
- Effective pain management through medication and other interventions
- Monitoring for signs of infection or other complications
- Gradual mobilization to prevent stiffness and promote healing
Return to Normal Activities
As you get better, you’ll start doing more things. It’s important to balance rest with activity to avoid hurting yourself again.
Tips for a successful return to activities:
- Follow the surgeon’s specific instructions regarding activity levels and restrictions.
- Engage in physical therapy to strengthen the back muscles and improve flexibility.
- Gradually increase activity levels, avoiding heavy lifting, bending, or twisting.
Long-Term Maintenance and Prevention
Keeping your spine healthy long-term means making lifestyle changes. This includes staying at a healthy weight, exercising regularly, and keeping good posture.
Long-term maintenance strategies:
- Regular exercise, such as walking, swimming, or yoga, to maintain flexibility and strength
- Dietary adjustments to maintain a healthy weight and reduce inflammation
- Ergonomic adjustments at work and home to reduce strain on the spine
Patient Stories: Recovery Experiences
Listening to others who have had herniated disc surgery can be very helpful. Many people say they feel much better and have a better quality of life after surgery and a good recovery plan.
“I was back to my normal activities within a few weeks, and the pain I had been experiencing for years was gone. The recovery process was challenging, but with the right support and guidance, it was manageable.”
— A herniated disc surgery patient
The Doctor-Patient Partnership in Treatment Decisions
Fixing a herniated disc needs teamwork between the patient and doctor. This teamwork is key to making choices that fit the patient’s needs and wishes.
A good doctor-patient relationship is based on respect, trust, and clear talk. It lets patients play a big part in their care. This makes them more likely to follow the treatment plan and get better results.
Shared Decision-Making Models
Shared decision-making is becoming more popular. It’s a way for doctors and patients to work together. They share info, talk about options, and decide together.
This approach leads to happier patients, better treatment following, and care that’s more tailored to them. It also lets patients share their values and preferences, which can really affect the outcome.
Questions to Ask Your Healthcare Provider
Patients should ask questions to understand their condition and treatment choices. Some important questions include:
- What are the good and bad sides of each treatment?
- How will the treatment change my daily life?
- Are there other treatments or therapies that could help?
- What results can we expect, and how will we know if it’s working?
Getting a Second Opinion
Getting a second opinion is common and can offer new insights. It’s useful when the diagnosis is unsure or when treatments are complex or risky.
Patients should feel free to ask for a second opinion. It’s a normal part of making decisions. It also lets them talk over worries or questions with another doctor.
Insurance and Financial Considerations
Insurance and money matters can affect treatment choices. Patients should talk about their insurance and costs with their doctor.
Knowing the financial side of treatments helps patients make choices that fit their budget. This way, they can pick options that work for them financially.
Conclusion
Dealing with a herniated disc needs a full plan, mixing both non-surgical and surgical steps. Knowing what causes and shows the problem is key to picking the right treatment.
First, doctors often try non-surgical ways like physical therapy and managing pain. They also suggest making lifestyle changes. If these don’t work, surgery might be next.
Deciding on surgery is a significant choice that requires careful consideration of the benefits and risks. New, less invasive surgery methods have made results better.
Having a treatment plan made just for you is essential. It should be worked out with your doctor. This plan helps get the best results, whether it’s through non-surgical methods or surgery.
FAQ
What are the non-surgical treatments for a herniated disc?
Non-surgical treatments include rest and pain management with medication. Physical therapy and lifestyle changes are also options. Chiropractic care, acupuncture, massage therapy, and yoga or Pilates are alternatives.
When should I consider surgery for a herniated disc?
Consider surgery if conservative treatments don’t work. Look for persistent or worsening neurological symptoms. Red flags that need urgent surgery are also important.
What are the surgical options for a herniated disc?
Surgical options include microdiscectomy and laminectomy. Spinal fusion and artificial disc replacement are also choices. Minimally invasive options like endoscopic discectomy and tubular microdiscectomy are available too.
Is surgery a last resort for a herniated disc?
Surgery is considered when other treatments fail. It’s for when the condition greatly affects your life. The decision depends on symptom severity, health, and personal preferences.
What are the benefits and risks of herniated disc surgery?
Surgery can relieve pain and symptoms. But, it carries risks like infection and nerve damage. Discuss long-term risks and outcomes with your healthcare provider.
What is the recovery process like after herniated disc surgery?
Recovery starts with immediate care after surgery. It involves gradually returning to normal activities. Long-term strategies for maintenance and prevention are also important.
How do I make informed decisions about my herniated disc treatment?
Making informed decisions means understanding your diagnosis and treatment options. It’s about working with your healthcare provider. This includes asking questions and considering second opinions.
What are the alternatives to surgery for a herniated disc?
Alternatives include physical therapy and pain management. Chiropractic care, acupuncture, and massage therapy are also options.
Can a herniated disc be managed without surgery?
Yes, many manage symptoms without surgery. This is through conservative treatments and lifestyle changes.
How do I know if I need surgery for my herniated disc?
The need for surgery depends on your symptoms and response to treatments. A healthcare provider can help decide based on
References
- Emerging Issues Questioning the Current Treatment Strategies for Lumbar Disc Herniation. (2022). Frontiers in Surgery. https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2022.814531/full
- Management of Lumbar Disc Herniation: A Systematic Review. (n.d.).. https://pmc.ncbi.nlm.nih.gov/articles/PMC10683841/
- Yoon, W. W., & colleagues. (2021). Herniated discs: when is surgery necessary? Bone & Joint Research. Retrieved from https://eor.bioscientifica.com/view/journals/eor/6/6/2058-5241.6.210020.xml