Last Updated on November 4, 2025 by mcelik
About 2% of adults experience a herniated disc, which occurs when the soft inner gel of the disc leaks through a tear in its outer layer.
Determining the herniated disc surgery necessity is a complex decision. It requires considering both traditional and modern medical approaches. The choice to undergo surgery depends on the severity of symptoms and whether non-surgical treatments have been effective.
Understanding herniated disc surgery necessity is crucial for patients dealing with this condition. Timely decisions can significantly impact recovery and long-term outcomes.
Key Takeaways
- Understanding the severity of a herniated disc is key to finding the right treatment.
- Trying non-surgical treatments first is usually the best approach.
- Surgery might be needed for those with very bad or lasting symptoms.
- It’s important to look at all options to decide if surgery is right.
- Acting fast can greatly improve the outcome for someone with a herniated disc.
Understanding Herniated Discs: Anatomy and Causes

Understanding herniated discs is crucial for selecting the appropriate treatment. The spine has many discs that help it move and stay strong. These discs act like shock absorbers between the vertebrae.
What happens when a disc herniates
A herniated disc happens when the soft center leaks out. This can make the disc bulge or break. It might press on nerves, causing pain, numbness, or weakness in the back or legs.
The herniated disc symptoms can be mild or very severe. It depends on where and how much the disc is herniated. Knowing this helps choose the right disc herniation treatment options.
Common causes of disc herniation
Disc herniation can come from aging, wear and tear, or injury. As we get older, our discs dry out and can tear more easily. A sudden injury can also cause a disc to herniate if the discs are already worn.
Doing heavy lifting or making sudden movements can stress the discs. This can make them more likely to herniate. Genetics can also play a part in getting disc problems.
Risk factors for developing herniated discs
Some things can make you more likely to get a herniated disc. Being between 30 and 50 years old is a big risk. Jobs that involve heavy lifting or twisting also increase the risk. Being overweight or having a family history of disc problems can also play a role.
Knowing these risks can help prevent herniated discs or make them less severe. If you do get a herniated disc, trying non-surgical treatment herniated disc options first is usually best. Surgery is usually for more serious cases or when other treatments don’t work.
Recognizing Symptoms of a Herniated Disc
It’s important to know the signs of a herniated disc to choose the right treatment. A herniated disc can lead to various symptoms that affect daily life. These symptoms can be different in severity and impact.
Pain Patterns and Characteristics
The pain from a herniated disc can change based on where and how severe it is. The pain often follows the path of the compressed nerve. This can cause herniated disc pain that feels sharp, dull, or burning.
For example, a herniated disc in the lower back can cause sciatica. This is a sharp pain that goes down the sciatic nerve.
In some cases, pain is focused in one area. In others, it spreads to other parts of the body. Knowing these pain patterns helps doctors diagnose and decide on treatment. This includes whether nerve compression surgery is needed.
Neurological Symptoms: Numbness, Tingling, and Weakness
A herniated disc can also cause neurological symptoms. These include numbness, tingling, and weakness in the affected limb. For example, a herniated disc in the neck can cause numbness or tingling in the arm or hand.
These symptoms happen because the herniated disc presses or irritates nearby nerves. This disrupts normal nerve function. The presence and severity of these symptoms help doctors understand the extent of nerve compression and the needed treatment.
How Symptoms Vary by Location of Herniation
The location of the herniated disc affects the symptoms. Herniations in the lower back often cause lower back pain and sciatica. Those in the neck can lead to neck pain and arm symptoms. Knowing how symptoms vary by location is key to diagnosing and treating herniated discs effectively.
The severity and progression of symptoms, known as progressive symptoms herniated disc, are also important. They help decide between non-surgical treatments or surgery.
The Natural History of Herniated Discs
It’s important to know how herniated discs progress naturally. Many people see their symptoms improve without surgery. This is thanks to the body’s own healing abilities.
Natural Healing of Herniated Discs
Studies show that many herniated discs can heal on their own. The body’s healing can fix symptoms, even with big herniations. This healing comes from less inflammation and the disc material getting absorbed.
What affects healing includes the herniation’s size and where it is. Smaller herniations heal better than big ones. Also, herniations that don’t break through the outer layer have a better chance of healing.
Timeline for Symptom Improvement
How fast symptoms get better varies a lot. Usually, the biggest improvements happen in the first few weeks or months. Many see their pain and function get better in 6 to 12 weeks.
A study found that many people with herniated discs get a lot better in 6 months. Some keep getting better after that. Knowing this timeline helps patients and doctors decide if surgery is needed.
In summary, many herniated discs can heal naturally with time. But whether to try non-surgical treatments or surgery depends on many things. These include how bad the symptoms are, how they affect daily life, and if there are any warning signs. Understanding healing and improvement timelines helps people make the best choices for their care.
Conservative Treatment Options
For many with herniated discs, non-surgical treatments are a good start. These methods help manage symptoms and improve function. They also avoid the risks of surgery.
Medication Management Strategies
Medicine is key in treating herniated disc pain. Doctors often prescribe:
- Over-the-counter pain relievers like ibuprofen or acetaminophen
- Muscle relaxants to ease spasms
- Oral steroids to cut down inflammation
These drugs can help lessen symptoms. This lets patients do physical therapy and other non-surgical treatments.
Physical Therapy Approaches
Physical therapy is a big part of non-surgical treatment. Therapists use different methods to:
- Boost flexibility and strength
- Improve posture and body mechanics
- Lessen pain with manual therapy and other treatments
A custom physical therapy plan can greatly help with symptoms and function.
Injection Therapies and Their Effectiveness
Injection therapies, like epidural steroid injections, target herniated disc symptoms. They inject anti-inflammatory medication directly to the area. This reduces pain and swelling.
| Treatment | Description | Effectiveness |
| Medication Management | Use of oral medications to manage pain and inflammation | High |
| Physical Therapy | Personalized exercise and manual therapy programs | High |
| Injection Therapies | Targeted injections to reduce inflammation and pain | Moderate to High |
Non-surgical treatments offer many ways to manage herniated disc symptoms. By using medication, physical therapy, and injections, many people find relief without surgery.
Herniated Disc Surgery Necessity: Key Indicators
There are several key indicators that suggest the need for herniated disc surgery. These signs are important in deciding if non-surgical treatments will work or if surgery is needed.
Red Flag Symptoms Requiring Immediate Surgical Evaluation
Certain symptoms, known as red flags, need immediate medical attention. They may require urgent surgery. These symptoms include:
- Progressive neurological deficits, such as increasing numbness or weakness
- Loss of bladder or bowel control
- Severe or worsening pain that does not improve with conservative treatment
Cauda equina syndrome, a condition where the nerves in the lower spine are compressed, is a medical emergency. It requires immediate surgical intervention.
When Conservative Treatment Fails
If treatments like medication, physical therapy, and injections don’t help, surgery might be considered. The time spent trying these treatments before surgery can vary. Usually, it’s a few weeks to a few months.
Factors influencing the decision to proceed with surgery include the severity of symptoms, how much they affect daily life, and the presence of any red flag symptoms.
Quality of Life Considerations
The impact of a herniated disc on a person’s quality of life is a big factor in deciding on surgery. If symptoms make daily activities, sleep, or overall well-being hard, surgery might be an option.
| Indicator | Description | Implication for Surgery |
| Red Flag Symptoms | Progressive neurological deficits, loss of bladder/bowel control | Immediate surgical evaluation is necessary |
| Failure of Conservative Treatment | Symptoms persist or worsen despite conservative treatment | Surgery is considered after several weeks to months |
| Quality of Life Impact | Significant impairment in daily activities and well-being | Surgical options explored for relief |
Diagnostic Procedures to Determine Surgical Need
To figure out if surgery is needed for a herniated disc, a detailed approach is key. This includes using advanced imaging, thorough neurological checks, and electrodiagnostic tests. These steps help doctors understand the condition well and choose the best treatment.
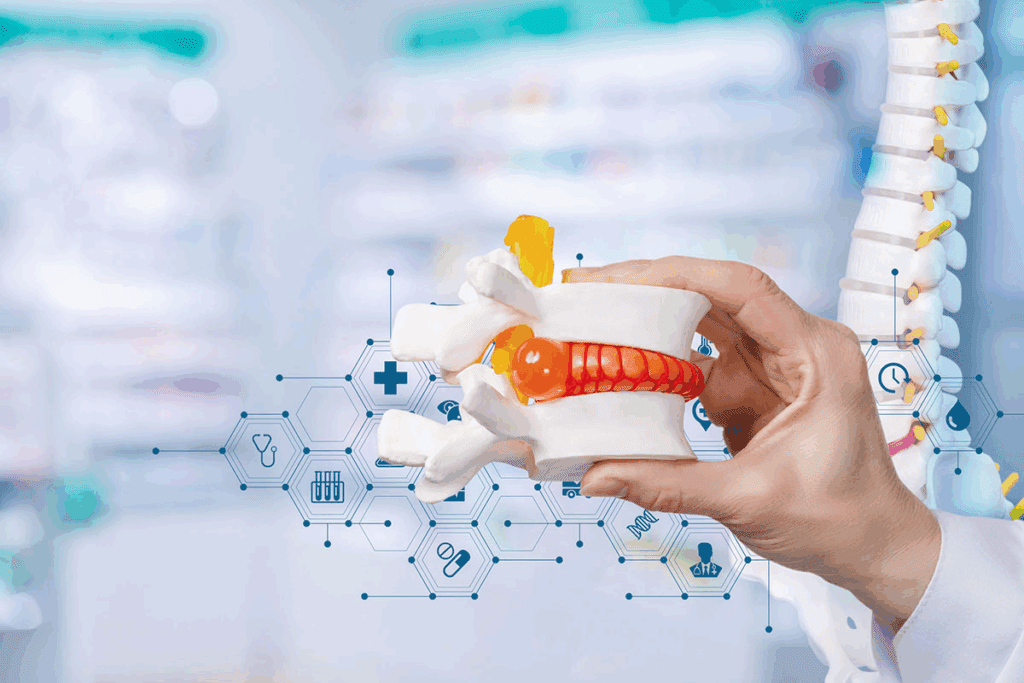
The Role of MRI and Other Imaging
Magnetic Resonance Imaging (MRI) is a top tool for checking herniated discs. It shows detailed pictures of the spine. This helps doctors see the disc and its effect on nerves and other parts.
Knowing the disc’s location and how bad it is helps decide if surgery is needed. Other tests like CT scans and X-rays, also help by showing more about the spine’s structure and any bone issues.
Neurological Examination Findings
A detailed neurological exam is very important. It checks muscle strength, feeling, and reflexes to see how nerves are affected. This helps doctors match symptoms with what imaging shows.
It guides them in deciding if surgery is needed.
Electrodiagnostic Testing (EMG/NCS)
Electrodiagnostic tests, like EMG and NCS, are key in checking nerve function. They show how nerve compression from a herniated disc affects nerves. These tests help doctors see how bad the damage is and if nerves can recover.
This info is important in deciding if surgery is the right choice.
The Decision-Making Process: Surgery vs. Continued Conservative Care
When you get a herniated disc diagnosis, you face a tough choice. You must decide between surgery and keeping up with conservative care. This choice is not easy and requires thinking about many things.
Shared Decision-Making with Your Healthcare Team
Shared decision-making means working together with your healthcare team. You talk about your diagnosis, treatment options, and what matters most to you. Good communication is essential to make sure you’re well-informed and can decide what’s best for you.
Your healthcare providers will share the latest research and treatment choices. They’ll talk about the good and bad sides of surgery versus conservative care. It’s important to ask questions and share your worries.
Weighing Risks and Benefits
Thinking about surgery for a herniated disc means looking at the risks and benefits. Surgery can lead to complications like infection or nerve damage. But, it might also help a lot with pain and moving better.
On the other hand, conservative care like physical therapy and medicine can also help a lot. It doesn’t have the surgery risks. But, how well it works depends on how bad the herniation is and your health.
Second Opinions and Their Importance
Getting a second opinion is a smart move. It lets you check your diagnosis and look at other treatment options. A second opinion can also make you feel more sure or point out risks you hadn’t thought of.
Don’t be afraid to ask for more info or talk to spinal care specialists. Being proactive can help you make better choices and get better results.
Types of Surgical Procedures for Herniated Discs
Surgery for herniated discs has changed a lot. Now, there are many procedures to fit each patient’s needs. The right surgery depends on where and how bad the herniation is, and the patient’s health.
Microdiscectomy: The Gold Standard
Microdiscectomy is seen as the top choice for herniated discs. It’s a small surgery that removes the part of the disc pressing on a nerve. It has smaller cuts, less damage, and faster healing than old surgeries.
- Lower chance of infection
- Less pain after surgery
- Back to normal sooner
Minimally Invasive Options
New, small surgeries for herniated discs are becoming popular. They promise less time to heal and less pain after. These surgeries use tiny cuts and special tools to take out the bad disc part.
Endoscopic Procedures
Endoscopic surgery for herniated discs is another small surgery. It uses a thin tube with a camera and light to see the disc. This method lets doctors remove the bad part carefully without hurting the rest of the area.
| Surgical Procedure | Key Benefits | Typical Recovery Time |
| Microdiscectomy | Smaller incisions, less tissue damage | 2-6 weeks |
| Minimally Invasive Surgery | Reduced post-operative pain, faster recovery | 2-4 weeks |
| Endoscopic Surgery | Minimal tissue disruption, precise removal of herniated material | 1-3 weeks |
Each surgery has its own good points and is right for different people. Talking to a doctor is key to finding the best surgery for a herniated disc.
Risks and Complications of Herniated Disc Surgery
It’s important to know the risks of herniated disc surgery before deciding. Surgery can help many people feel better, but it’s not without risks.
Common Surgical Complications
Herniated disc surgery comes with some risks. These include infection, bleeding, and nerve damage. Infections are rare but can need antibiotics or more surgery.
Bleeding can happen during or after surgery. This might cause a hematoma, which can press on nerves and worsen symptoms. Nerve damage is a big worry because of the surgery’s close work with nerves. Surgeons try hard to avoid it, but there’s always a chance.
Long-term Risks
There are long-term risks too. Some people might have pain again or new symptoms because of scar tissue or not fully healing.
Another risk is adjacent segment disease. This is when the discs or joints next to the surgery area wear out faster because of how the spine moves.
Factors that Increase Surgical Risk
Some things can make surgery riskier. These include being older, not being very healthy, and having other health issues like diabetes or heart disease.
Smoking is a big risk because it slows healing and can cause more problems. Being overweight can also make surgery harder and recovery slower because of extra stress on the spine.
Having had spinal surgery before or a lot of scar tissue can make future surgeries harder.
Recovery and Rehabilitation After Herniated Disc Surgery
Recovering from herniated disc surgery involves several steps. These include immediate care, physical therapy, and slowly getting back to normal. Knowing what to expect can help patients prepare and get the best results.
Immediate Post-Operative Period
The first hours after surgery are critical. Patients are watched closely in the recovery room to catch any problems early. Managing pain is a big focus, with medicines to help keep discomfort low.
Most patients go home the same day. But some might need to stay overnight, depending on the surgery and their health. It’s important to have someone to drive them home and help for the first day or two.
Physical Therapy and Rehabilitation Protocols
Physical therapy is key after surgery. It helps patients build strength, improve flexibility, and get back to normal. The exercises and plans depend on the surgery and the patient’s needs.
Physical therapy usually starts a few weeks after surgery. It starts with easy exercises and gets harder as the patient gets stronger.
Timeline for Return to Normal Activities
How long it takes to get back to normal varies. It depends on the surgery, the patient’s health, and their job. Here’s a general idea of what to expect:
| Activity Level | Timeline |
| Light activities (e.g., walking, light housekeeping) | Within 1-2 weeks |
| Moderate activities (e.g., bending, lifting light objects) | Within 4-6 weeks |
| Strenuous activities (e.g., heavy lifting, contact sports) | Within 8-12 weeks or as advised by the surgeon |
It’s important to follow the surgeon’s advice on when to start activities again. This ensures a safe and effective recovery.
Patient Experiences and Case Studies
Looking at patient experiences and case studies helps us see how herniated disc treatments work. These stories give us insights into what treatments are most effective. They help patients make better choices about their care.
Success Stories After Surgery
Many people have found relief from herniated disc symptoms through surgery. For example, a 45-year-old office worker had a microdiscectomy. He was back to normal in just six weeks. These success stories after herniated disc surgery show that surgery can be a good option when other treatments don’t work.
A 30-year-old athlete also found success with surgery. He had a herniated disc in his lower back. After trying other treatments, he had an endoscopic discectomy. He was training again in just three months. His story shows the importance of finding the right surgery for each person.
When Conservative Treatment Worked
Not everyone needs surgery; many find relief with non-surgical treatments. A 50-year-old woman with a herniated cervical disc improved with physical therapy and medication. Her story is just one of many conservative treatment success stories that show non-surgical methods can work well.
- Physical therapy helped improve mobility and strength.
- Medication management reduced pain and inflammation.
- Lifestyle changes, like ergonomic adjustments and regular exercise, helped her recover long-term.
Lessons Learned from Patient Experiences
Looking at patient experiences teaches us important lessons. One key lesson is the need for personalized treatment plans. What works for one person might not work for another. This shows the importance of treatments that are tailored to each individual.
Also, patient experiences highlight the value of complete care. This includes rehabilitation and making lifestyle changes. These steps are key to achieving and keeping recovery.
- Acting early can prevent serious damage.
- Using a team approach often leads to the best results.
- Teaching patients and empowering them is vital for recovery.
By studying these varied experiences, healthcare providers can improve their treatment plans. Patients can also better understand what to expect from their treatment journey.
Emerging Treatments and Technologies
New breakthroughs in regenerative medicine and minimally invasive surgery are changing how we treat herniated discs. Medical research keeps moving forward, bringing new treatments that help patients recover faster and feel better.
Regenerative Medicine Approaches
Regenerative medicine is leading the way in herniated disc treatments. It uses the body’s own healing powers to fix damaged disc tissue. Platelet-rich plasma (PRP) therapy and stem cell therapy are being studied for their ability to heal discs and ease pain.
PRP therapy uses the patient’s own blood to create a growth factor-rich solution. This solution is injected into the disc to help it heal. Early studies show it can help reduce pain and improve function for those with herniated discs.
Advances in Minimally Invasive Techniques
Minimally invasive surgery is getting better, giving patients less invasive options than traditional surgery. New endoscopic and percutaneous procedures mean smaller incisions. This leads to less damage, less pain, and quicker recovery times.
These techniques are precise, targeting the herniated disc without harming nearby tissues. This precision improves results and lowers the risk of complications. It makes these procedures a good choice for those needing surgery.
Future Directions in Herniated Disc Treatment
The future of herniated disc treatment looks bright. Research into biomaterials and tissue engineering might bring new implants and devices. Better imaging and diagnostic tools will also help diagnose and treat herniated discs more effectively.
As these new treatments and technologies grow, they will shape the future of herniated disc care. It’s important for patients and doctors to stay updated on these advancements for the best results.
Preventing Recurrence After Treatment
To stop herniated discs from coming back, you need to make lifestyle changes and adjust your workspace. After treatment, it’s key to keep your spine healthy. This helps avoid future disc problems.
Lifestyle Modifications
Changing your lifestyle can help a lot. Here are some tips:
- Keep a healthy weight to ease spine pressure
- Stop smoking to help discs heal
- Avoid long periods of sitting or lying down
- Do low-impact exercises to strengthen your back
“A healthy lifestyle is key to avoiding back pain and herniated discs.”
-Experts advise.
Ergonomic Considerations
Improving your workspace is also important. Here’s how:
- Make sure your workspace supports good posture, with your monitor at eye level and a chair that supports your back.
- Use the right lifting techniques, bending at the knees, and keeping things close to your body.
- Take breaks when sitting or standing for a long time.
Exercise and Core Strengthening
Exercise is vital to prevent herniated discs from coming back. Focus on exercises that strengthen your core and improve flexibility:
- Do exercises that work your abdominal and back muscles, like planks and bridges.
- Try low-impact activities like walking, swimming, or cycling.
- Physical therapy can help with exercises made just for you.
| Exercise | Benefit | Frequency |
| Plank | Strengthens core muscles | 3 times a week |
| Bridges | Strengthens back and gluteal muscles | 3 times a week |
| Swimming | Improves cardiovascular health without straining the spine | 2-3 times a week |
“Regular exercise and maintaining a healthy weight are key factors in preventing the recurrence of herniated discs.”
– Spine Health Experts
By following these tips, you can lower the chance of herniated discs coming back. This helps you stay healthy and active.
Conclusion: Making an Informed Decision About Herniated Disc Surgery
Choosing to have surgery for a herniated disc is a big decision. We’ve looked at many things that help make this choice, like what a herniated disc is and why it happens. We’ve also talked about symptoms, treatments that don’t involve surgery, and what surgery is like.
Understanding the risks and benefits of surgery is key. It’s important to talk to doctors, including top surgeons for herniated disc surgery. They can help figure out the best treatment for you.
By looking at both sides and thinking about your own situation, you can make a good choice. This way, you can find the best treatment for your herniated disc.
FAQ
What are the signs that indicate I need herniated disc surgery?
You might need surgery if you have severe pain that doesn’t go away. Also, if you feel numbness, tingling, or weakness in your limbs. Losing control of your bladder or bowel is another sign. If treatments don’t help, surgery might be needed.
How do I know if my herniated disc will heal on its own?
Some herniated discs can heal with time and treatment. The size and location of the herniation matter. So does how bad your symptoms are.
What are the conservative treatment options for a herniated disc?
Treatments like medicine, physical therapy, and injections can help. Making lifestyle changes is also important. These methods aim to ease pain and help you heal.
When is surgery considered necessary for a herniated disc?
Surgery is needed if treatments don’t work. Or if you have severe symptoms like weakness or loss of bladder control.
What diagnostic procedures are used to determine the need for herniated disc surgery?
Doctors use MRI and other tests to check if you need surgery. They also do neurological exams and tests like EMG/NCS. These help see how bad the herniation is and its effect on nerves.
What are the different types of surgical procedures for herniated discs?
There are several surgeries, like microdiscectomy and minimally invasive discectomy. The right one depends on the herniation and your health.
What are the risks and complications associated with herniated disc surgery?
Surgery can lead to infection, bleeding, nerve damage, and the herniation coming back. Older age and poor health increase these risks.
How long does it take to recover from herniated disc surgery?
Recovery time varies. It depends on the surgery and your health. Most people can get back to normal in weeks to months.
Can I prevent the recurrence of a herniated disc after treatment?
Yes, you can prevent it by staying healthy and exercising. Good posture and avoiding heavy lifting also help.
What are the emerging treatments and technologies for herniated disc treatment?
New treatments include regenerative medicine and advanced surgery. These aim to improve results and reduce recovery time.
How do I make an informed decision about herniated disc surgery?
Talk to a doctor to understand your options. Weigh the pros and cons. Think about what’s best for you.
References
- Awadalla, A. M., Al-Dandan, R., Morsi, A. H., & Al-Sarraf, N. (2023). Management of Lumbar Disc Herniation: A Systematic Review. PMC, 1–18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10683841/
- Yoon, W. W., & colleagues. (2021). Herniated discs: when is surgery necessary? Bone & Joint Research. https://eor.bioscientifica.com/view/journals/eor/6/6/2058-5241.6.210020.xml