Last Updated on November 4, 2025 by mcelik
Every year, thousands of people undergo herniated disc surgery to relieve their pain. However, one serious risk that concerns many is herniated disc surgery paralysis. While rare, this potential complication highlights the importance of understanding the surgery fully.
Herniated disc surgery is generally safe, but knowing the risks is crucial. The possibility of herniated disc surgery paralysis can make patients carefully weigh the benefits of surgery against potential complications, ensuring informed decisions about their care.
Key Takeaways
- Understanding the risks associated with herniated disc surgery.
- The possibility of paralysis as a surgery complication.
- What increases the risk of paralysis after surgery.
- Signs to watch for before and after surgery.
- Steps to take before surgery to lower risks.
Understanding Herniated Discs and Their Impact
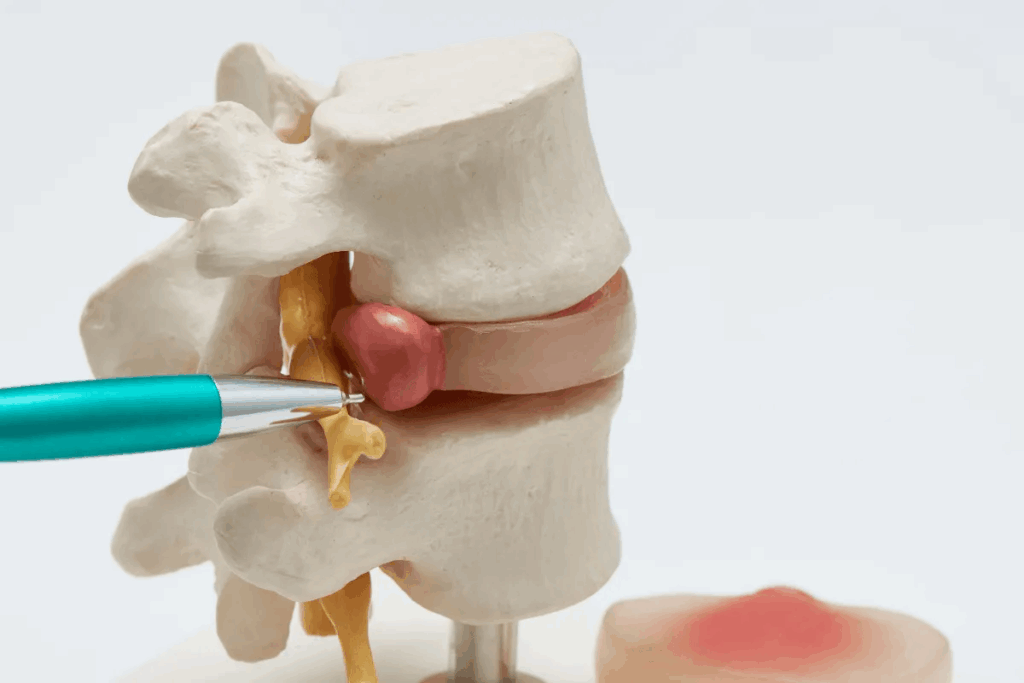
The spine is a complex structure, and herniated discs are a big challenge in spinal health. A herniated disc happens when the soft, jelly-like center of a spinal disc bulges out. This is because of a tear in the outer, tougher layer. This can put pressure on the spinal cord and nerves, causing pain, numbness, and weakness.
What Is a Herniated Disc?
A herniated disc occurs when the soft inner material of a spinal disc bulges out. This can happen because of aging, injury, or wear and tear on the spine. The herniation can occur in any part of the spine, but it’s most common in the lower back (lumbar spine) and neck (cervical spine).
The symptoms of a herniated disc can vary a lot. They depend on where and how bad the herniation is. Common symptoms include pain in one spot, pain that spreads along the nerve, numbness, tingling, and muscle weakness.
How Herniated Discs Affect the Spinal Cord
When a disc herniates, it can press on or irritate nearby nerves, including those in the spinal cord. The spinal cord is a key part of the central nervous system. Any compression or injury to it can lead to serious neurological symptoms.
The impact of a herniated disc on the spinal cord can vary. It can range from mild discomfort to severe neurological deficits. In some cases, it may cause:
- Radicular pain or numbness in the limbs
- Muscle weakness or paralysis in severe cases
- Loss of bladder or bowel control in extreme instances
Understanding herniated discs and their impact on the spinal cord is key. It helps determine the right treatment and manage risks of complications, like paralysis.
When Surgery Becomes Necessary for Herniated Discs

When treatments for herniated discs don’t work, surgery might be needed. Herniated discs often get better with treatments, but sometimes surgery is necessary. This is true for severe symptoms or emergencies.
Conservative Treatment Options
Before surgery, patients try many treatments. These include:
- Physical therapy to improve mobility and strength
- Medications such as pain relievers and muscle relaxants
- Epidural steroid injections to reduce inflammation
- Lifestyle modifications, including diet and exercise changes
These treatments aim to lessen pain and help the body heal. But if symptoms don’t get better, surgery might be next.
Indications for Surgical Intervention
Surgery is usually recommended when:
- Conservative treatments have failed to provide relief after 6-12 weeks
- There is significant nerve compression, causing muscle weakness or numbness
- Pain is severe and interferes with daily activities
Choosing surgery is a big decision. It’s made with a healthcare provider’s advice, considering your health and condition.
Emergency Situations Requiring Immediate Surgery
Emergency surgery is needed for serious conditions. Cauda equina syndrome is one. It’s when nerves in the lower spine are compressed. This can cause severe pain, numbness, and permanent nerve damage if not treated quickly.
| Condition | Description | Urgency |
| Cauda Equina Syndrome | Compression of nerves in the lower spine | Emergency Surgery Required |
| Severe Nerve Compression | Significant nerve damage or risk of damage | Urgent Surgical Intervention |
| Progressive Neurological Deficit | Worsening neurological symptoms | Surgery Often Recommended |
It’s important to know when surgery is needed. Understanding the risks and benefits helps make a good choice. Talk to your healthcare provider to decide the best treatment for you.
Common Types of Herniated Disc Surgeries
There are many surgeries for herniated discs, each with its own benefits and risks. The right surgery depends on where and how bad the herniation is, and the patient’s health.
Microdiscectomy
Microdiscectomy is a small surgery for herniated discs. It removes the damaged part of the disc that’s pressing on nerves. This surgery is done with a microscope or endoscope, making the cut smaller and causing less damage.
Benefits: It causes less pain after surgery, heals faster, and leaves fewer scars.
Laminectomy and Laminotomy
Laminectomy and laminotomy remove parts of the vertebrae to relieve nerve pressure. Laminectomy takes out the whole lamina, while laminotomy just takes a piece of it.
Risks and Benefits: These surgeries can greatly reduce nerve pressure. But they can also make the spine unstable and risk nerve damage.
Spinal Fusion
Spinal fusion joins two or more vertebrae together with bone grafts, rods, or other devices. It’s often done with other surgeries, like laminectomy to prevent spine instability.
Considerations: Spinal fusion makes the spine stable but limits movement. It can also put more stress on other vertebrae.
| Surgical Procedure | Primary Benefit | Potential Risks |
| Microdiscectomy | Minimally invasive, with less postoperative pain | Nerve damage, infection |
| Laminectomy/Laminotomy | Relieves pressure on spinal nerves | Spinal instability, nerve damage |
| Spinal Fusion | Provides spinal stability | Limited range of motion, stress on adjacent vertebrae |
Knowing about the different herniated disc surgeries is key to making the right choice. Each surgery has its own good points and possible downsides. The best surgery depends on the patient’s specific situation and needs.
Herniated Disc Surgery Paralysis: Understanding the Risk
Herniated disc surgery is usually safe, but there’s a rare risk of paralysis. This risk is serious and needs to be understood well.
The surgery aims to ease pressure on the spinal cord or nerves from a herniated disc. It often works well, but there are risks, including paralysis.
Statistical Likelihood of Paralysis
It’s hard to say exactly how likely paralysis is after surgery. This is because of different surgeries, patients, and how reports are done. But most studies say the risk is less than 1%.
- A study in the Journal of Neurosurgery: Spine found paralysis risk to be under 0.5%.
- The Spine Journal also reported a low rate of major complications.
These numbers show paralysis is rare after herniated disc surgery. But knowing what increases this risk is key.
Factors That Increase Paralysis Risk
Several things can make paralysis more likely after surgery. These include:
- Pre-existing spinal conditions, like spinal stenosis or past surgeries, which can make the surgery harder.
- The complexity of the surgery, with more complex surgeries being riskier.
- Patient health factors, like age, overall health, and conditions like diabetes or vascular disease.
A spine specialist says, “Knowing these risk factors is important for surgeons and patients to make good decisions about surgery.”
“The key to lowering paralysis risk is a detailed check before surgery and careful planning.”
-A spine surgeon highlights
By knowing these factors and taking steps to prevent them, the risk of paralysis can be lowered. This helps ensure the best results for patients having herniated disc surgery.
Types of Paralysis That Can Result from Spinal Surgery

It’s important for patients and doctors to know about the risk of paralysis after spinal surgery. This surgery is often needed for many spinal problems. But, it can lead to serious complications, like paralysis.
Paralysis from spinal surgery can take two main forms. These are paraplegia and quadriplegia. The type depends on where and how badly the spinal cord is hurt.
Paraplegia vs. Quadriplegia
Paraplegia means you can’t move your lower body. This usually happens when the spinal cord is damaged in the thoracic or lumbar areas. On the other hand, quadriplegia, or tetraplegia, means you can’t move your arms or legs. This is because of injuries in the cervical spine.
Knowing the difference between these two is very important. It affects how well you can live and how much you can recover.
Complete vs. Incomplete Spinal Cord Injury
Spinal cord injuries can also be classified as complete or incomplete. A complete injury means you have no feeling or movement below the injury. An incomplete injury means some feeling or movement might be left.
The type of injury greatly affects your chances of getting better. A complete injury is much harder to recover from than an incomplete one.
| Type of Paralysis | Description | Typical Cause |
| Paraplegia | Paralysis of the lower half of the body | Injuries to the thoracic or lumbar spine |
| Quadriplegia | Paralysis of both arms and legs | Injuries to the cervical spine |
| Complete Spinal Cord Injury | Total loss of sensory and motor function below the injury site | Severe damage to the spinal cord |
| Incomplete Spinal Cord Injury | Partial damage to the spinal cord with some remaining sensory or motor function | Partial injury to the spinal cord |
Mechanisms of Paralysis During Disc Surgery
It’s important to know why paralysis can happen during disc surgery. This can be due to direct harm to the spinal cord or because of vascular issues. These problems can be very serious, so both doctors and patients need to understand the risks.
Direct Spinal Cord Injury
Direct injury to the spinal cord is a big worry during disc surgery. This can happen if surgical tools accidentally harm the spinal cord or nearby nerves. The risk is higher if the herniated disc is big or presses directly on the spinal cord. Doctors work hard to avoid these injuries, but the surgery’s complexity and the spinal’s delicate nature make it tough.
“The area where surgery happens is close to the spinal cord, making it risky,” says a top neurosurgeon. “Doctors must be very careful to not hurt the spinal cord.”
Vascular Complications Leading to Paralysis
Vascular issues during disc surgery can also cause paralysis. These problems might come from damage to blood vessels that feed the spinal cord, leading to not enough blood flow. Not enough blood can seriously harm the spinal cord, causing paralysis or other nerve problems. The chance of vascular issues highlights the need for careful surgery and planning before the operation.
- Vascular injury during surgery
- Ischemia due to compromised blood flow
- Potential for paralysis or neurological deficits
Understanding these causes helps doctors manage risks and improve results for patients having disc surgery. It’s key for patients to talk about their specific risks and worries with their healthcare team.
Pre-Existing Conditions That Increase Paralysis Risk
Health issues before surgery, like those affecting the spine, can raise the chance of paralysis. It’s key to know these conditions to understand the risks of surgery.
Spinal Stenosis
Spinal stenosis narrows the spinal canal, pressing on the spinal cord and nerves. Patients with this condition face a higher risk of paralysis during herniated disc surgery. It’s important to plan carefully before and during surgery to lower this risk.
Osteoporosis
Osteoporosis weakens bones, making them more likely to break. During herniated disc surgery, this can make the procedure harder. It’s important to consider this condition and take extra precautions during surgery.
Previous Spinal Surgeries
Those who have had spinal surgery before may face a higher risk of paralysis in future surgeries. This is due to scar tissue, changes in the spine, and nerve damage. Reviewing the patient’s past surgeries is key to managing these risks.
In summary, conditions like spinal stenosis, osteoporosis, and past spinal surgeries greatly affect the risk of paralysis in herniated disc surgery. Healthcare providers can better manage these risks by understanding these factors. This helps in making informed decisions about surgery and reducing complications.
Surgeon Experience and Its Impact on Surgical Outcomes
The skill and experience of the surgeon are key in herniated disc surgery. Spinal surgery is complex and requires a lot of expertise. The surgeon’s ability to handle both routine and unexpected complications greatly affects the outcome.
Many studies have looked into the link between surgeon experience and surgical results. They show that more experienced and trained surgeons usually get better results.
The Importance of Specialized Training
Specialized training in spinal surgery is vital for the best results. Surgeons with advanced training can handle complex cases better and reduce complications. Specialized training programs keep surgeons updated with the latest techniques and technologies.
- Advanced fellowship programs in spinal surgery
- Continuous education and training in new surgical techniques
- Participation in workshops and conferences focused on spinal surgery
Surgeons with specialized training are skilled in using advanced tools and techniques. This includes intraoperative neuromonitoring and navigation-assisted surgery. These technologies improve the precision and safety of spinal surgeries.
Volume-Outcome Relationship in Spine Surgery
The volume-outcome relationship in spine surgery shows a link between the number of surgeries and outcomes. Studies indicate that surgeons and hospitals with more surgeries have better results, fewer complications, and happier patients.
“The evidence suggests that for complex surgical procedures like spine surgery, the experience of the surgeon and the volume of procedures performed are critical determinants of outcome.”
A big factor in this relationship is the surgeon’s ability to manage complications. Experienced surgeons can better handle unexpected problems during surgery. This greatly affects patient outcomes.
When choosing a surgeon for herniated disc surgery, look at their experience, training, and volume of procedures. Patients should ask about their surgeon’s qualifications and experience. This helps them make informed decisions about their care.
Technological Advances Reducing Paralysis Risk
Technological advancements have greatly helped lower the risk of paralysis in herniated disc surgery. These new tools have made surgeries more precise and safer for patients.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring (IONM) is a key technology that has cut down paralysis risks in spinal surgeries. It uses electrophysiological methods to check the spinal cord and nerve roots in real-time during surgery.
Key benefits of IONM include:
- Real-time feedback to surgeons
- Early detection of nerve damage
- Ability to adjust surgical technique
IONM has been linked to fewer neurological problems, like paralysis. It lets surgeons act fast if they see any nerve issues.
Navigation-Assisted Surgery
Navigation-assisted surgery, or computer-assisted surgery, is another big step forward. It uses advanced imaging to guide surgeons in real-time during the surgery.
| Feature | Conventional Surgery | Navigation-Assisted Surgery |
| Precision | Limited by the surgeon’s experience | Enhanced by real-time imaging |
| Risk of Complications | Higher due to less precision | Lower due to improved accuracy |
| Surgical Time | Variable, often longer | Often shorter due to better planning |
Navigation-assisted surgery makes surgeries more precise and lowers the risk of complications. This means a lower chance of paralysis in herniated disc surgery.
In conclusion, new technologies like intraoperative neuromonitoring and navigation-assisted surgery have made herniated disc surgery safer. They reduce paralysis risks and improve patient results.
Anesthesia Complications That Can Lead to Paralysis
Anesthesia problems during herniated disc surgery can lead to paralysis. Anesthesia is key for patient comfort and safety during surgery. But, its complications can be severe.
Hypotension and Spinal Cord Ischemia
Hypotension, or low blood pressure, is a major anesthesia complication. It can cause spinal cord ischemia. This is when the spinal cord doesn’t get enough blood, leading to damage or paralysis.
- Risk Factors: Vascular disease, blood loss during surgery, and dehydration can raise the risk of hypotension.
- Prevention Strategies: Keeping an eye on blood pressure, staying hydrated, and using vasopressors when needed can help prevent this.
Positioning-Related Injuries
Positioning-related injuries are another risk with anesthesia. If the patient is not positioned correctly during surgery, it can harm nerves or the spinal cord. This could lead to paralysis.
- Using the right supports and checking the patient’s position often during long surgeries.
- Using intraoperative neuromonitoring to spot nerve damage early.
Knowing these risks and taking steps to prevent them can lower the chance of anesthesia-related paralysis. This ensures safer outcomes for patients with herniated discs.
Post-Operative Complications That May Cause Delayed Paralysis
Herniated disc surgery is generally safe but can lead to complications. These complications may cause paralysis. It’s important for patients and healthcare providers to understand these risks.
Epidural Hematoma
An epidural hematoma is a blood collection outside the dura mater. This membrane protects the spinal cord but is within the spinal canal. It can compress the spinal cord, causing neurological issues like paralysis.
Symptoms include severe back pain, weakness or numbness in the legs, and loss of bladder or bowel control. Quick surgery is often needed to relieve the spinal cord’s pressure.
Infection and Abscess Formation
Infections can happen after surgery, including herniated disc surgery. An infection in the spinal area can form an abscess. This is a pocket of pus that can also compress the spinal cord.
Signs of infection or abscess include fever, increased pain, redness, swelling, and neurological symptoms. Quick diagnosis and treatment with antibiotics or surgery are key to prevent lasting damage.
Post-Operative Edema
Post-operative edema, or swelling, is common after surgery. In spinal surgery, too much swelling can compress the spinal cord, potentially causing paralysis.
Managing swelling involves monitoring and may include corticosteroids. In some cases, more surgery is needed to relieve the spinal cord’s pressure.
| Complication | Symptoms | Treatment |
| Epidural Hematoma | Severe back pain, progressive weakness or numbness, loss of bladder or bowel control | Surgical intervention to relieve pressure |
| Infection and Abscess Formation | Fever, increased pain, redness, swelling, neurological symptoms | Antibiotics or surgical drainage |
| Post-Operative Edema | Swelling, possible neurological deficits | Corticosteroids, monitoring, possible surgical intervention |
Knowing about these complications helps patients and healthcare providers manage risks. This is important for herniated disc surgery.
Signs and Symptoms of Post-Surgical Spinal Cord Injury
Post-surgical spinal cord injury symptoms can vary. It’s important to recognize them quickly for effective treatment. After herniated disc surgery, patients should watch out for possible complications.
Immediate Warning Signs
Look out for severe pain, numbness, or weakness in your limbs. You might also notice loss of bladder or bowel control. These are serious signs.
- Numbness or tingling sensations in the extremities
- Muscle weakness or paralysis
- Difficulty walking or maintaining balance
Delayed Manifestations of Spinal Cord Damage
Sometimes, symptoms of spinal cord injury show up later. Delayed manifestations can include chronic pain, persistent numbness, or progressive weakness in limbs.
It’s vital for patients to keep an eye on their condition after surgery. Tell your healthcare provider about any unusual symptoms. Early action can greatly improve outcomes for post-surgical spinal cord injuries.
Emergency Management of Post-Surgical Paralysis
Post-surgical paralysis is a serious issue that needs quick action. When it happens after herniated disc surgery, acting fast is key to avoid lasting harm.
Diagnostic Procedures
Diagnostic tests are vital to find out why paralysis happens after surgery. Imaging studies like MRI or CT scans check the spinal cord and nearby areas for any blockages or injuries.
These tests help doctors understand how bad the damage is. They also guide what treatment to use next. Sometimes, electrophysiological tests like electromyography (EMG) are used to check nerve function.
Medical Interventions
Medical treatments are often the first step for post-surgical paralysis. Doctors might give corticosteroids to reduce swelling around the spinal cord.
They also work on managing pain and keeping the spinal cord well-supplied with blood. If paralysis is due to an epidural hematoma, quick medical help is needed to stop more damage.
Surgical Decompression
In some cases, surgical decompression is needed to take pressure off the spinal cord. This surgery removes any blockages or stabilizes the spine to prevent more harm.
Whether to do surgery depends on the patient’s health and the reason for paralysis. Each case is different.
Long-Term Rehabilitation After Spinal Cord Injury
Effective long-term rehabilitation is key to maximizing recovery and improving quality of life after a spinal cord injury. It’s vital for helping individuals regain independence and adapt to any lasting changes.
Physical Therapy Approaches
Physical therapy plays a vital role in the rehabilitation process. It focuses on improving mobility, strength, and flexibility. Physical therapists use various techniques, including exercises, stretches, and manual therapy, to help patients achieve their goals.
A key component of physical therapy is the development of a personalized exercise program. This program is tailored to the individual’s specific needs and abilities. It aims to enhance functional capacity and promote overall well-being.
“Physical therapy is not just about recovering from injury; it’s about regaining the ability to live life to the fullest.”
-A physical therapist advises
Occupational Therapy and Adaptive Equipment
Occupational therapy is another essential aspect of rehabilitation. It focuses on enabling individuals to perform daily activities and participate in meaningful occupations. Occupational therapists work with patients to identify strategies and adaptive equipment that can facilitate independence.
Adaptive equipment, such as wheelchairs, walkers, and specialized utensils, can significantly enhance an individual’s ability to engage in daily tasks. The selection of appropriate adaptive equipment is a critical component of the occupational therapy process.
| Type of Adaptive Equipment | Purpose | Examples |
| Mobility Aids | Enhance mobility and accessibility | Wheelchairs, walkers, canes |
| Bathroom Adaptations | Improve safety and independence in the bathroom | Grab bars, shower chairs, and raised toilet seats |
| Daily Living Aids | Facilitate performance of daily tasks | Adaptive utensils, dressing aids, and reachers |
The integration of physical therapy, occupational therapy, and adaptive equipment into a holistic rehabilitation plan is essential for optimizing outcomes after spinal cord injury.
Alternative Treatments to Consider Before Surgery
Before surgery for a herniated disc, think about alternative treatments. These include non-surgical methods and complementary approaches. They might help ease symptoms and improve your life without the risks.
Advanced Non-Surgical Interventions
There are many non-surgical ways to manage herniated disc symptoms. These include:
- Physical Therapy: Personalized exercises to boost flexibility and strength.
- Epidural Steroid Injections: To cut down inflammation and ease pain.
- Chiropractic Care: Spinal adjustments to align the spine and lessen disc pressure.
Complementary and Integrative Approaches
Complementary and integrative methods can boost the effect of regular treatments. Some of these include:
- Acupuncture: To encourage healing and lessen pain.
- Yoga and Meditation: To enhance flexibility and lower stress.
- Herbal Supplements: Some supplements may help reduce inflammation and aid in healing.
When to Persist with Conservative Treatment
Knowing when to stick with non-surgical treatments and when to consider surgery is key. The choice depends on symptom severity, daily life impact, and how well alternative treatments work.
| Factors to Consider | Conservative Treatment | Surgical Intervention |
| Symptom Severity | Mild to moderate | Severe |
| Impact on Daily Life | Minimal | Significant |
| Effectiveness of Alternative Treatments | Effective | Limited or no relief |
By weighing these factors, patients can make smart choices about their treatment.
Minimizing Your Risk of Complications
To lower the risk of problems during and after herniated disc surgery, careful planning is key. Several important steps can help reduce the chance of bad outcomes.
Choosing the Right Surgeon and Facility
Finding a skilled surgeon is essential. Choose a surgeon who is board-certified and has a good success rate. The place where you have surgery also matters. It should have the latest technology and a knowledgeable team.
Pre-Operative Preparation
Getting ready for surgery is important. Follow your surgeon’s advice on medications, food, and other steps. Be ready to share your medical history, including past surgeries or health issues.
Post-Operative Care Compliance
It’s important to follow your surgeon’s post-surgery advice. This might mean not moving too much, taking care of your wound, and keeping appointments. Sticking to these instructions can prevent issues like infections or slow healing.
Conclusion
It’s important to know the risks of herniated disc surgery, like paralysis. This article has covered many aspects of the surgery. We talked about the different types of surgeries and possible complications.
The chance of paralysis is low but serious. Things like your spinal health, the surgeon’s skill, and new technology can help lower this risk.
Knowing these factors helps patients make better choices. It’s key to talk to a doctor about the surgery’s benefits and risks. This way, you can find the best treatment for your situation.
FAQ
What are the risks associated with herniated disc surgery?
Herniated disc surgery can lead to paralysis, infection, bleeding, and nerve damage. It’s important to know these risks before surgery.
Can herniated disc surgery cause paralysis?
Yes, surgery can cause paralysis, but it’s rare. The risk depends on the surgery type, surgeon’s skill, and your health.
What is the likelihood of paralysis after herniated disc surgery?
Paralysis risk after surgery is low, from less than 1% to a few percent. It varies based on the surgery and your health.
What are the symptoms of paralysis after spinal surgery?
Symptoms include numbness, weakness, or loss of limb function. Look out for severe pain, trouble walking, or bladder issues.
How can the risk of paralysis be minimized during herniated disc surgery?
Choose an experienced surgeon and use advanced monitoring tools. Also, manage any health issues before surgery.
What are the alternative treatments to surgery for herniated discs?
Try physical therapy, pain meds, acupuncture, or chiropractic care first. These can help avoid surgery.
When is surgical intervention necessary for herniated discs?
Surgery is needed when other treatments fail or in emergencies like cauda equina syndrome. It’s urgent to prevent permanent damage.
What is the role of intraoperative neuromonitoring in reducing paralysis risk?
It detects nerve damage during surgery. This allows for quick action to prevent paralysis.
How does a surgeon’s experience impact the outcome of herniated disc surgery?
More experienced surgeons have better results and fewer complications. This includes a lower risk of paralysis.
What are the signs of post-surgical spinal cord injury?
Look for sudden numbness, weakness, loss of bladder or bowel control, and severe pain. Quick action is key.
What is the recovery process like after spinal surgery?
Recovery includes rest, physical therapy, and possibly rehab. It depends on the surgery and your health.
Can pre-existing conditions increase the risk of paralysis during herniated disc surgery?
Yes, conditions like spinal stenosis or osteoporosis can raise the risk of paralysis during surgery.
What are the long-term rehabilitation strategies after spinal cord injury?
Strategies include physical therapy, occupational therapy, and using adaptive equipment. These help regain independence.
References
- Sulaiman, W. I., Chen, H., Peng, Y., & Wu, Y. (2021). Analysis of long-term results of lumbar discectomy with and without annular repair: a retrospective cohort. Journal of Orthopaedic Surgery and Research, 16(1), 303. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9421207/





