Blog
Liv Hospital aspires to lead the way in providing reliable and high-quality healthcare by combining a patient-centered approach, an experienced team of physicians, and the strength of multidisciplinary collaboration. With our commitment to applying advanced diagnostic and treatment methods in step with global standards, our ultimate focus remains clear: your health.
Sort By Letter
 Pediatrics
PediatricsBrain Fog And Dementia: Scary Chemo Link
Many cancer survivors worry about the effects of chemotherapy on their brains. This is known as “chemo brain.&#...
 Cancer
CancerIs MRI And CT Scan The Same? Crucial Comparison Revealed
Understanding the difference between MRI and CT scans is key for your health. At Liv Hospital, we use the latest MRI ...
 Ophthalmology
OphthalmologyOculomotor Cranial Nerve Function: Amazing Guide
The oculomotor nerve, also known as the third cranial nerve, is key for eye movements and functions. It starts in the...
 Cancer
CancerBone Scan: Quick And Detailed Full Body Imaging
A full body nuclear scan, like a whole-body PET/CT, is a test that gives detailed images. These images are key for fi...
 Cancer
CancerCT Scan Results: How to Read Cancer & Abnormalities
Understanding CT scan results is key for both patients and doctors. At Liv Hospital, we help our patients understand ...
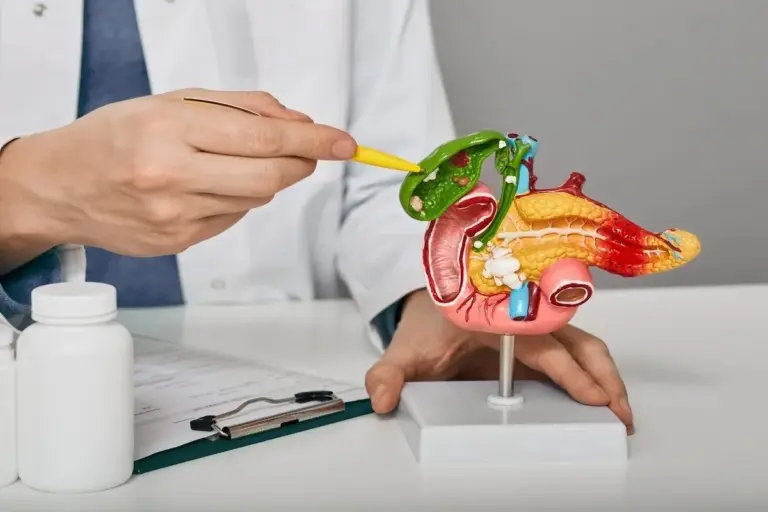
 Gallstones
GallstonesDefine Choledocholithiasis: 15 Critical, Key Facts
Choledocholithiasis is when gallstones block the common bile duct (CBD). It happens in about 15% of people with galls...
 General Surgery
General SurgeryHepatobiliary Surgery: Best Safety Secrets
Hepatobiliary surgery, including liver and biliary resections, comes with big risks. These complex surgeries can caus...
 Ear Nose Throat
Ear Nose ThroatHow to Clean Ears with a Syringe: Step-by-Step Guide
Effectively remove excess earwax with a syringe ear cleaner. Our step-by-step guide explains the safe and effective t...
 Pediatrics
PediatricsBleeding Conditions — 8 Key Facts You Must Know
Bleeding disorders are medical issues that make it hard for the body to stop bleeding. This can cause bleeding that l...
No posts found
Try different filters



