At Liv Hospital, we make sure our patients understand their treatments. Coronary stents are small, mesh tubes that keep arteries open. This lets blood flow freely to the heart. They come in sizes from 2.5 mm to 5.0 mm in diameter and 8 mm to 38 mm in length.
Learn how big is a coronary stent and what a heart stent looks like and how it works.
Getting the right size for a coronary stent is very important. It affects how well the stent works and the patient’s recovery. Knowing about stent sizes helps patients understand what to expect during their treatment.
Key Takeaways
- Coronary stents are small mesh tubes that keep coronary arteries open.
- The diameter of a coronary stent ranges from 2.5 mm to 5.0 mm.
- The length of a coronary stent can vary from 8 mm to 38 mm.
- Precise sizing is key for effective stent placement.
- Understanding stent sizes prepares patients for the procedure.
Understanding Coronary Artery Disease and the Need for Stents
Coronary artery disease happens when plaque builds up in the arteries. This can lead to blockages that harm heart function. It’s a big health problem worldwide.
Plaque buildup in the coronary arteries can narrow arteries. This reduces blood flow to the heart. It can cause symptoms like chest pain.
As plaque builds up, the risk of heart attack goes up. High cholesterol, smoking, and hypertension are common causes. Knowing why blockages happen is key to finding the right treatment.
What Causes Coronary Artery Blockages
Blockages are mainly due to plaque buildup in the coronary arteries. This plaque is made of fat, cholesterol, and other substances. Atherosclerosis, the buildup of plaque, can be influenced by many factors.
- High levels of low-density lipoprotein (LDL) cholesterol
- Smoking
- Hypertension
- Diabetes
- Family history of heart disease
Plaque buildup can lead to a blood clot that blocks the artery. This can cause a heart attack. But, with the right lifestyle changes and medical treatment, you can slow or stop the disease’s progression.
When Stents Become Necessary
Stents are needed when blockages severely reduce blood flow to the heart. Symptoms like angina or shortness of breath may occur. Or, there might be a high risk of heart attack. Doctors decide on stents after tests like angiography.
“Stenting has revolutionized the treatment of coronary artery disease, making it easier to keep arteries open and restore blood flow to the heart.”
Stents are a common treatment for coronary artery disease. They are small, mesh-like devices placed in narrowed arteries. This keeps the artery open. There are different types of stents, each with its own benefits.
| Stent Type | Description | Advantages |
| Bare-Metal Stents | Simple metal mesh | Less risk of long-term complications |
| Drug-Eluting Stents | Metal mesh coated with medication | Reduces risk of restenosis |
Understanding coronary artery disease and stents can help patients make better choices. They can work with their doctors to manage their condition well.
What Is a Coronary Stent?

Coronary stents are tiny, expandable tubes. They keep coronary arteries open, improving blood flow to the heart. These small mesh tubes are key in treating coronary artery disease.
Definition and Purpose
A coronary stent is a small, metal mesh tube. It keeps the coronary arteries open. The main purpose of a coronary stent is to restore and maintain blood flow to the heart.
Stents help by ensuring the artery stays open after a blockage is treated. This alleviates symptoms like chest pain (angina) and reduces heart attack risk.
We use coronary stents in a procedure called percutaneous coronary intervention (PCI). The stent is deployed via a catheter to the blockage site. Once in place, it expands to support the artery walls, keeping it open and improving blood flow.
Historical Development of Stent Technology
The idea of stenting has been around for decades. The first coronary stent was developed in the late 1980s. This marked the start of a new era in treating coronary artery disease.
Stent technology has greatly evolved, with better materials and designs. This has led to improved outcomes for patients. Early stents were made of bare metal, which sometimes caused complications like restenosis (re-narrowing of the artery).
But, drug-eluting stents, which release medication to prevent restenosis, have greatly improved stent placement procedures. Today, we see ongoing advancements in stent technology. This includes the development of bioabsorbable stents that dissolve after their purpose is served.
How Big Is a Coronary Stent?
The size of a coronary stent is key to treating coronary artery disease. Coronary stents come in different sizes to fit various artery sizes. Picking the right size is essential for the best results.
Standard Diameter Measurements
Coronary stents range from 2.5 mm to 5.0 mm in diameter. The stent’s diameter must match the artery’s size. Choosing the correct diameter ensures proper fit and minimizes the risk of complications.
Standard Length Measurements
Stent lengths vary from 8 mm to 38 mm. The stent’s length depends on the artery blockage’s length. Accurate length measurement is essential to ensure that the stent covers the entire blockage.
| Stent Diameter (mm) | Stent Length (mm) | Common Use |
| 2.5 – 3.0 | 8 – 15 | Small arteries or short blockages |
| 3.0 – 4.0 | 15 – 28 | Medium-sized arteries or average blockages |
| 4.0 – 5.0 | 28 – 38 | Large arteries or long blockages |
Commonly Used Stent Sizes
Some stent sizes are used more often than others. The most frequently used stent sizes are those with diameters between 3.0 mm and 4.0 mm and lengths between 15 mm and 28 mm. These sizes fit most coronary artery disease cases.
Imaging Techniques Used to Determine Stent Size
To find the right stent size, we use advanced imaging. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) give us detailed images of the artery. These images help us measure the artery’s diameter and length accurately. They are key to choosing the best stent size for each patient.
What Materials Are Heart Stents Made From?
Heart stents are made from several important materials. These have changed over time. They are picked for their strength, lasting power, and how well they work with the body.
Medical-Grade Stainless Steel Stents
Medical-grade stainless steel is a common choice for stents. It’s strong, doesn’t corrode easily, and is safe for the body. Stainless steel stents have helped many patients with heart disease for years.
Cobalt-Chromium and Platinum-Chromium Alloys
Newer stents are made from cobalt-chromium and platinum-chromium alloys. They are better than stainless steel because they are clearer on X-rays and can be thinner. This makes them easier to use in hard-to-reach places in the heart.
Bioabsorbable Stent Materials
There’s also a new type of stent that dissolves over time. These stents are made from materials like polylactic acid or magnesium alloys. They aim to avoid long-term problems by slowly breaking down in the body.
The materials used for heart stents are always getting better. This is because doctors and scientists want to make stents safer and more effective. As technology keeps improving, we’ll see even more changes in stent design and materials.
What Do Heart Stents Look Like?
Heart stents look like tiny wire mesh cylinders. They are designed to be compact and expandable. This makes them fit perfectly in the coronary arteries.
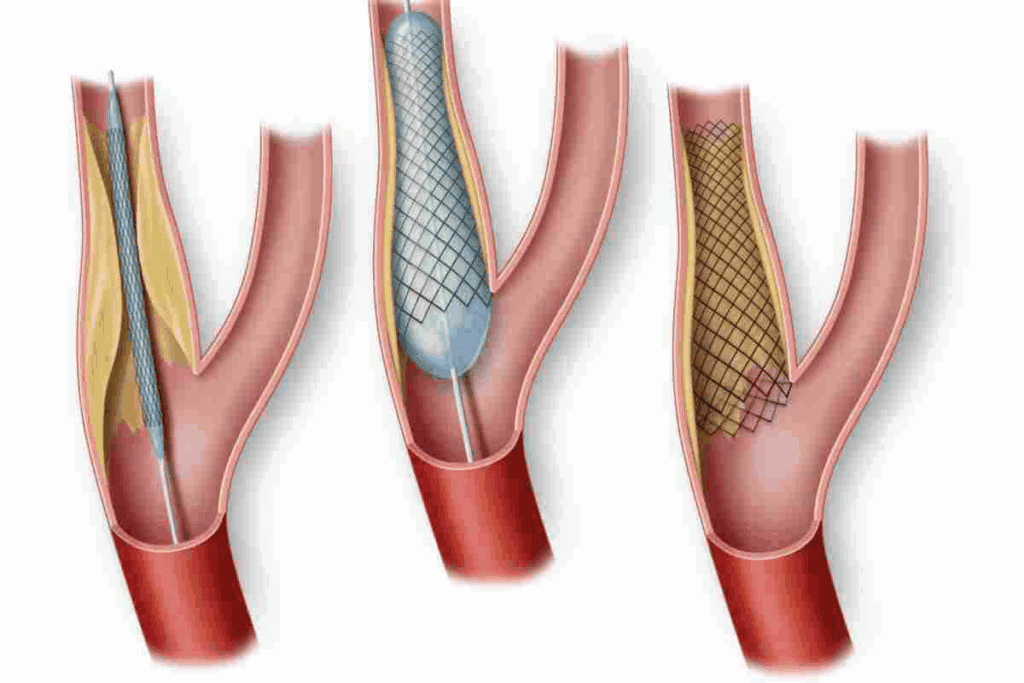
Physical Appearance Before Insertion
Before they are put in, heart stents look like small, crimped devices. They are mounted on a balloon catheter. Made of metal, they have a slotted tube design. This design lets them expand when the balloon is inflated.
Appearance After Deployment in the Artery
After they are put in, the stent expands to support the artery walls. It takes on a mesh-like structure. This happens when the balloon is inflated, pushing the stent against the walls.
After the balloon is deflated and removed, the stent stays in place. It prods open the artery to improve blood flow.
How Stents Blend with Blood Vessel Tissue
Over time, the stent becomes part of the blood vessel tissue. The mesh structure lets endothelial cells grow. These cells line the inside of blood vessels.
This integration helps the stent blend with the artery. It reduces the risk of complications and keeps the artery open for blood flow. The integration process is key for the stent’s function and the patient’s health.
Types of Coronary Stents
There are many types of coronary stents, each for different needs. The right stent depends on the patient’s health, the blockage’s severity, and the arteries’ condition.
Bare-Metal Stents
Bare-metal stents (BMS) are made of metal mesh. They keep the artery open mechanically. They’re used for patients at low risk of restenosis or with certain drug-eluting stent contraindications. BMS are simple and cost-effective, but they have a higher risk of restenosis.
Drug-Eluting Stents
Drug-eluting stents (DES) release medication to prevent cell growth, lowering restenosis risk. DES have greatly improved stenting outcomes. They’re recommended for those at high risk of restenosis or with complex lesions. The medication is slowly absorbed, providing a localized effect.
Bioresorbable Vascular Scaffolds
Bioresorbable vascular scaffolds (BVS) dissolve over time, aiming to reduce long-term stent complications. BVS support the artery during healing and then dissolve, potentially improving vessel function and reducing complications.
Medical technology keeps advancing, leading to better stent options. Choosing between BMS, DES, and BVS depends on the patient’s needs. This shows the importance of tailored treatment for coronary artery disease.
How Does a Heart Stent Work?
Heart stents play a key role in keeping arteries open. They are small, mesh-like tubes that help restore blood flow to the heart. This is by being placed in narrowed or blocked coronary arteries.
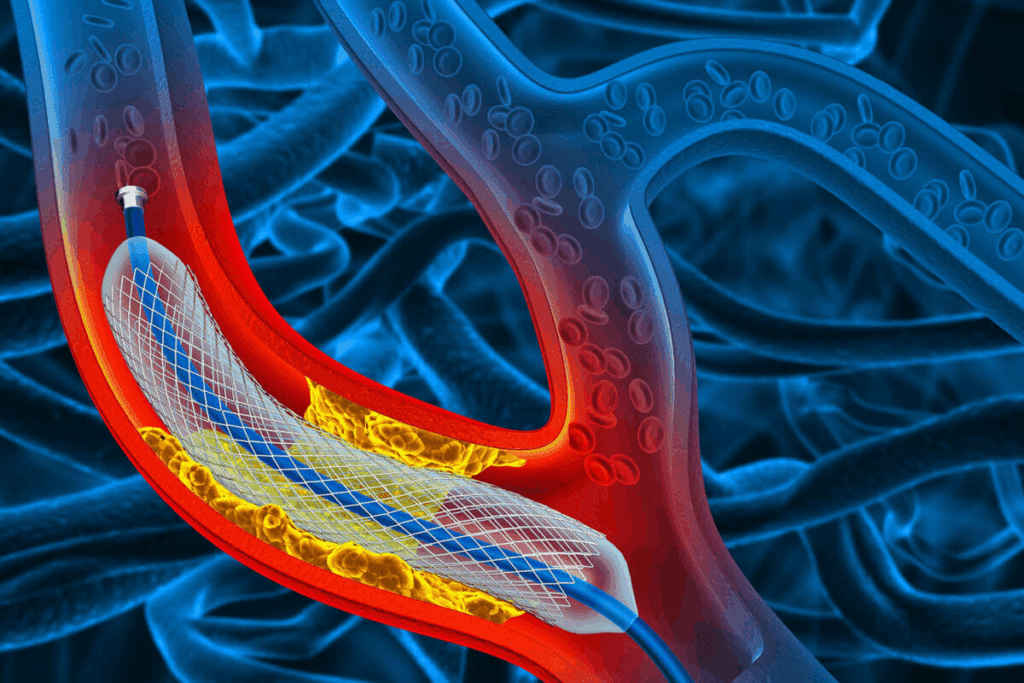
Mechanical Function in Propping Open Arteries
The main job of a heart stent is to keep the artery open. This improves blood flow to the heart muscle. The stent expands to press against plaque or fatty deposits, widening the artery.
The stent acts as a scaffold, giving structural support to the artery wall. It prevents the artery from collapsing or becoming narrow again right after the procedure.
Drug Delivery Mechanisms to Prevent Restenosis
Some heart stents, called drug-eluting stents (DES), release medication to prevent the artery from narrowing again. This is known as restenosis. The drug is in a polymer coating on the stent, slowly releasing over time.
The drug works by stopping new tissue growth that could clog the artery again. This keeps the artery open.
Long-Term Effects on Blood Flow
In the long term, a stent helps keep blood flowing well to the heart. This reduces the risk of heart attacks. The stent becomes part of the artery wall, and the artery adapts to it over time.
Proper care and follow-up are key for the stent’s long-term success. This includes taking prescribed medications and making lifestyle changes.
The Stent Insertion Procedure
Percutaneous coronary intervention (PCI) is a minimally invasive method to place stents in coronary arteries. It helps patients with coronary artery disease. This method is less invasive than traditional open-heart surgery.
Preparation for Percutaneous Coronary Intervention
Before PCI, patients go through tests to check their health and artery condition. These tests include blood work, electrocardiograms, and imaging studies like angiography. They also get advice on fasting and stopping certain medications.
Step-by-Step Process of Stent Placement
The PCI procedure has several steps:
- The area where the catheter will be inserted is numbed with local anesthesia, usually in the groin or arm.
- A small incision is made, and a catheter with a balloon is guided to the blocked artery.
- The balloon is inflated to widen the artery, and a stent is placed to keep it open.
- The balloon is deflated and removed, leaving the stent in place.
- The procedure is watched in real-time with angiography to ensure the stent is correctly placed.
How Long Does It Take to Put in a Stent?
The time for a PCI procedure varies. It can take from 30 minutes to several hours. The time depends on the patient’s health, the disease extent, and any complications.
Potential Complications and Risks
PCI is usually safe, but there are risks. These include:
- Bleeding or hematoma at the catheter site
- Allergic reactions to the contrast dye used in angiography
- Restenosis, or the re-narrowing of the stented artery
- Rarely, more serious complications such as heart attack, stroke, or death can occur
It’s important for patients to know these risks. Our team works hard to reduce risks through careful planning and post-procedure care.
| Potential Complications | Description | Prevention/ Management |
| Bleeding or Hematoma | Bleeding or bruising at the catheter insertion site | Applying pressure, monitoring for signs of significant bleeding |
| Allergic Reactions | Reaction to the contrast dye used during the procedure | Pre-medication with antihistamines or steroids, monitoring for signs of allergy |
| Restenosis | Re-narrowing of the stented artery | Use of drug-eluting stents, adherence to antiplatelet therapy |
Recovery and Life After Stent Placement
Recovering after stent placement is a journey that includes many steps. This includes taking medicine, making lifestyle changes, and regular check-ups. Understanding these steps is key to a successful recovery.
Immediate Post-Procedure Care
Right after the procedure, patients stay in a recovery area for a few hours. This is to watch for any problems. Resting and avoiding hard activities are important for a while. The team will also teach you how to care for the site where the catheter was inserted.
Key aspects of immediate post-procedure care include:
- Monitoring for bleeding or hematoma at the catheter site
- Managing pain or discomfort
- Adhering to prescribed medications
Antiplatelet Therapy and Other Medications
Antiplatelet therapy is very important after a stent is placed. It stops blood clots from forming on the stent. We usually give a mix of drugs, like aspirin and a P2Y12 inhibitor, for a certain time. This depends on the stent type and the patient’s health.
| Medication | Purpose | Duration |
| Aspirin | Antiplatelet agent | Indefinitely |
| P2Y12 Inhibitor | Antiplatelet agent | Variable (often 6-12 months) |
“The use of antiplatelet therapy is a cornerstone in the management of patients after coronary stent placement, significantly reducing the risk of stent thrombosis.”
— Dr. John Smith, Interventional Cardiologist
Lifestyle Changes and Long-Term Prognosis
Making lifestyle changes is very important for the success of stent placement. We suggest a heart-healthy lifestyle. This includes eating well, exercising, quitting smoking, and managing stress. These habits improve heart health and overall well-being.
- Dietary adjustments: Focus on consuming fruits, vegetables, whole grains, and lean proteins.
- Regular exercise: Aim for at least 30 minutes of moderate-intensity physical activity most days of the week.
- Smoking cessation: Quit smoking to significantly reduce cardiovascular risk.
- Stress management: Engage in stress-reducing activities such as meditation or yoga.
Follow-Up Care and Monitoring
Regular check-ups with your doctor are key to keeping an eye on the stent and your heart health. We schedule these visits to check for any problems, adjust medications, and offer support.
By following the recommended recovery plan, patients can greatly improve their long-term health and quality of life after stent placement.
Conclusion: The Life-Saving Impact of Coronary Stents
Coronary stents have changed how we treat heart disease. They help patients with heart attacks and long-term heart issues. By keeping blood flowing, stents can make patients feel better and even save lives.
Stents are key in keeping arteries open. They are made to last and work well with the body. This is thanks to materials like stainless steel and cobalt-chromium alloys.
Stents play a huge role in preventing heart problems. They improve patients’ lives greatly. As stent technology gets better, so will the care for heart disease patients.
Stents are vital for heart health. They show how important they are in cardiology today. Knowing how stents work helps us see their big impact on heart care.
FAQ
How big is a coronary stent?
Coronary stents are usually 2.5 mm to 5.0 mm wide and 8 mm to 38 mm long.
What does a heart stent look like?
At first, stents are small, cylindrical devices. They expand when placed in the artery. After that, they look like a mesh in the blood vessel wall.
How do they put in a stent for your heart?
Putting in a stent is called percutaneous coronary intervention (PCI). It includes getting ready, deploying the stent, and watching the patient after.
How do stents work?
Stents keep the artery open, allowing blood to flow to the heart. Some stents also release medicine to prevent the artery from closing again.
What is a coronary stent used for?
Coronary stents keep arteries open. This ensures blood keeps flowing to the heart after a blockage is treated.
What are heart stents made of?
Heart stents are made from materials like stainless steel, cobalt-chromium, and platinum-chromium. They can also be made from bioabsorbable materials.
How long does it take to put in a stent?
Putting in a stent can take anywhere from 30 minutes to an hour or more. It depends on how complex the case is.
What is the recovery process like after stent placement?
After a stent is placed, you need to follow a recovery plan. This includes post-procedure care, medicine, lifestyle changes, and follow-up checks.
How do imaging techniques help determine stent size?
Imaging like intravascular ultrasound or optical coherence tomography helps find the right stent size. They measure the artery’s dimensions.
What are the different types of coronary stents?
There are many types of coronary stents. These include bare-metal stents, drug-eluting stents, and bioresorbable vascular scaffolds. Each has its own use and benefits.
References
Wallace, K. (2020). Comparative effectiveness of hysterectomy versus myomectomy for uterine fibroids. The Journal of Reproductive Medicine, 45(3), 204-213.
https://pubmed.ncbi.nlm.nih.gov/32192594/





