Last Updated on November 27, 2025 by Bilal Hasdemir

Atrial fibrillation (AFib) is a heart condition that makes the heart beat irregularly and fast. This can cause blood flow to be less efficient. It might lead to hypotension, or low blood pressure.
It’s important to understand how AFib affects blood pressure. At Liv Hospital, we focus on top-notch healthcare. We support international patients with the latest care methods.
Key Takeaways
- Atrial fibrillation can disrupt normal heart rhythm, leading to inefficient blood flow.
- Inefficient blood flow may result in hypotension or low blood pressure.
- Comprehensive care is essential for managing AFib and related hypotension.
- Liv Hospital offers advanced diagnosis and treatment for heart rhythm and blood pressure challenges.
- Our team is dedicated to providing personalized care for international patients.
Understanding Atrial Fibrillation: The Basics
Atrial fibrillation, or AFib, is a heart rhythm disorder affecting millions. It causes an irregular and fast heart rate. This can lead to serious health issues if not treated.
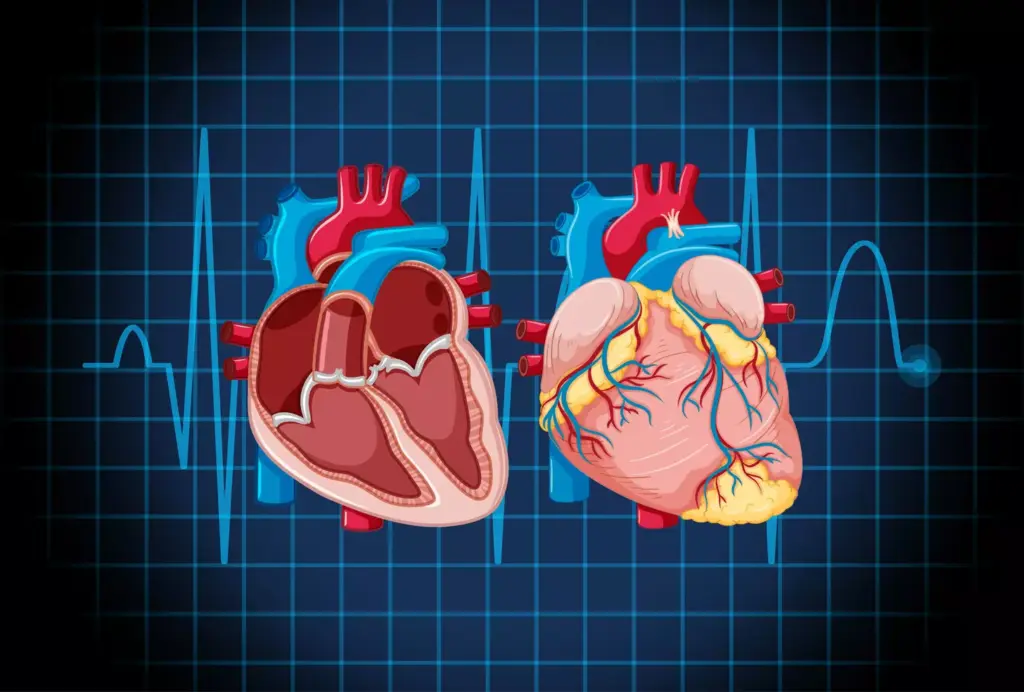
What Happens During Atrial Fibrillation?
In AFib, the heart’s upper chambers beat chaotically. This makes it hard for blood to move into the ventricles. It can cause low blood pressure, leading to dizziness or weakness.
The irregular heartbeat also makes blood pool in the atria. This raises the risk of stroke.
Common Causes and Risk Factors
Many factors can lead to atrial fibrillation. Some common causes and risk factors include:
- Hypertension: High blood pressure is a big risk factor for AFib.
- Heart Disease: Heart problems like coronary artery disease and valve issues can raise the risk.
- Obesity: Being overweight or obese increases the risk of AFib.
- Age: AFib risk grows with age, more so after 65.
| Risk Factor | Description | Impact on AFib Risk |
|---|---|---|
| Hypertension | High blood pressure | Increases risk significantly |
| Heart Disease | Coronary artery disease, heart valve problems | Moderately increases risk |
| Obesity | Being overweight or obese | Increases risk |
Knowing the basics of AFib is key to understanding its effects. Recognizing causes and risk factors helps manage the condition. It also reduces the risk of related health problems.
The Relationship Between Heart Rhythm and Blood Pressure
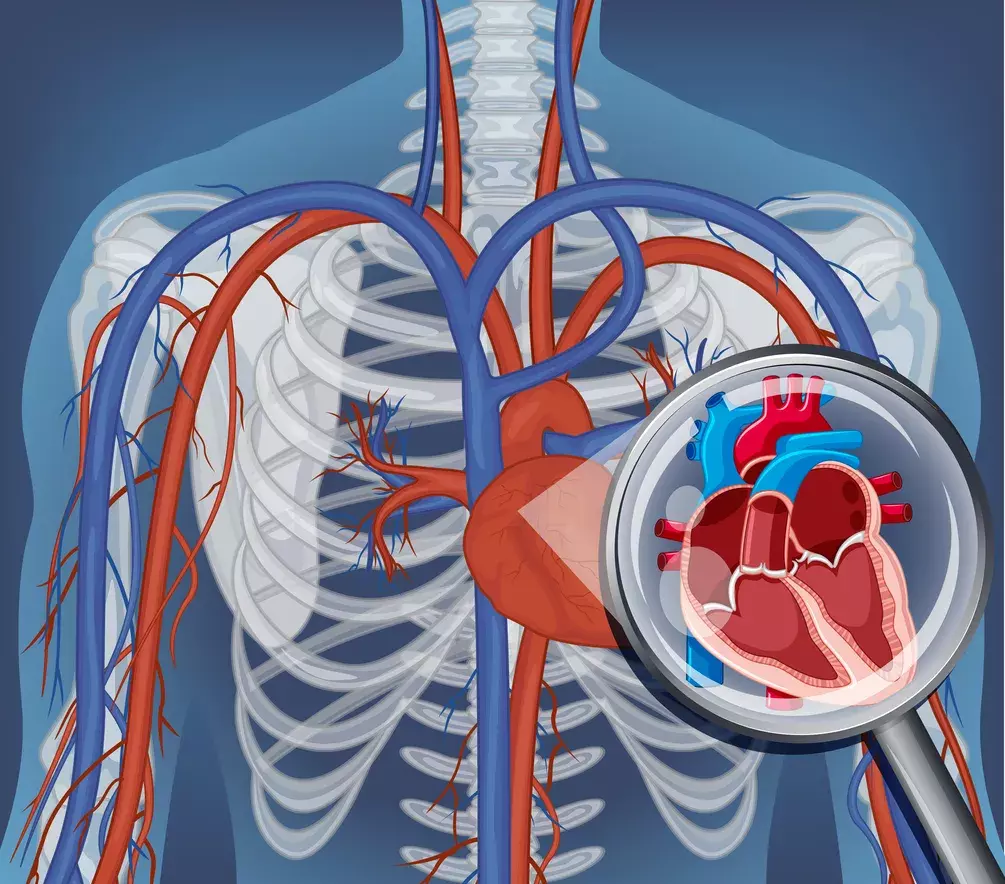
Heart rhythm is key to keeping blood pressure in check. It helps the heart pump blood well, keeping blood pressure healthy.
Normal Heart Function and Blood Pressure Regulation
The heart’s rhythm is controlled by the SA node, its natural pacemaker. It sends signals to the atria, making them contract and push blood into the ventricles. Then, the ventricles contract, sending blood to the lungs and body.
This process is vital for keeping blood pressure right.
Key factors in blood pressure regulation include:
- Cardiac output: The amount of blood pumped by the heart per minute.
- Vascular resistance: The resistance to blood flow in the blood vessels.
- Blood volume: The total amount of blood in the circulatory system.
How Cardiac Arrhythmias Affect Circulation
Cardiac arrhythmias, like AFib, mess up the heart’s rhythm. This makes blood pumping less efficient and can change blood pressure.
The impact of AFib on circulation includes:
- Reduced cardiac efficiency due to irregular heartbeats.
- Potential for decreased blood pressure due to reduced cardiac output.
- Increased risk of thromboembolic events due to blood stasis.
Understanding heart rhythm and blood pressure is vital for heart health, mainly for those with AFib. Knowing how arrhythmias affect blood flow helps doctors create better treatment plans.
Can AFib Cause Low Blood Pressure?
Atrial fibrillation can cause many heart problems, including changes in blood pressure. We will look at how AFib affects blood pressure and why it happens.
Atrial fibrillation (AFib) means your heart beats irregularly and fast. This can make your heart pump less blood. A study found that “AFib can cause a reduction in cardiac output, contributing to hypotension.”
Mechanisms Behind AFib-Related Hypotension
The irregular heart rhythm of AFib can mess with how well the heart works. This can lead to several reasons for low blood pressure:
- Reduced cardiac output due to inefficient heartbeats
- Inadequate ventricular filling
- Mitral regurgitation
So, people with AFib might have low blood pressure. It’s important to know these reasons to manage AFib well and keep blood pressure stable.
Frequency of Low Blood Pressure in AFib Patients
Research shows low blood pressure is a big problem for AFib patients. Studies found that more AFib patients have low blood pressure than others. A recent study said, “hypotension is a common comorbidity in patients with AFib, affecting their overall cardiovascular health.”
Knowing how often and why low blood pressure happens in AFib patients is key. Healthcare providers can then make better treatment plans. This can help improve how AFib patients feel and do better overall.
Recognizing Low Blood Pressure in AFib Patients
It’s key for AFib patients to know the signs of low blood pressure. Atrial fibrillation, or AFib, makes it harder to spot hypotension because of its irregular heartbeats. But, knowing the common symptoms can help patients get the right care.
Common Symptoms and Warning Signs
AFib patients with low blood pressure might feel dizzy, weak, or faint. These feelings happen because the heart isn’t pumping enough blood. Other signs include:
- Lightheadedness or feeling like you might pass out
- Fatigue or a general feeling of being unwell
- Shortness of breath
- Chest pain or discomfort
AFib patients should watch their condition closely. They should tell their doctor about any new or getting worse symptoms.
When to Seek Medical Attention
If you’re feeling any of these, get medical help right away:
- Severe dizziness or fainting
- Chest pain or pressure
- Severe shortness of breath
- Confusion or difficulty speaking
Prompt medical attention is vital to avoid serious problems. AFib patients should work closely with their healthcare team to manage their condition well.
The Bidirectional Relationship: Orthostatic Hypotension and AFib Risk
Recent studies have found a link between orthostatic hypotension and AFib risk. This means people with orthostatic hypotension are more likely to get AFib. Also, those with AFib might face a higher risk of orthostatic hypotension.
Research Findings on the 40% Increased Risk
Research shows a 40% higher risk of AFib in those with orthostatic hypotension. This highlights the need to watch and manage orthostatic hypotension to lower AFib risk.
A study in a top cardiology journal found a link between orthostatic hypotension and AFib. It looked at a big group of patients and controlled for other factors. This confirms orthostatic hypotension as a risk factor for AFib.
| Condition | Increased Risk of AFib | Study Findings |
|---|---|---|
| Orthostatic Hypotension | 40% | Significant correlation between orthostatic hypotension and AFib incidence |
| No Orthostatic Hypotension | Baseline | Lower incidence of AFib compared to those with orthostatic hypotension |
Underlying Mechanisms Connecting Both Conditions
The link between orthostatic hypotension and AFib involves several factors. Autonomic dysfunction, common in orthostatic hypotension, can disrupt heart rhythm. This can lead to AFib.
Also, heart diseases like hypertension and heart failure can worsen both conditions. They can make orthostatic hypotension and AFib more likely.
Knowing how these conditions are connected is key. It helps in finding ways to manage both at the same time.
Irregular Heart Rates and Blood Perfusion Issues
AFib can affect the body’s circulatory system in many ways. An irregular heartbeat can lead to inefficient blood circulation. This can cause problems with how well organs get blood.
Disruption of Normal Blood Flow
AFib makes the heart’s upper chambers (atria) quiver instead of beat right. This quivering makes the heart pump blood less well. It can lower the heart’s ability to pump blood.
This can mean organs don’t get the oxygen and nutrients they need. This is a big worry for people with heart problems or those at risk for blood flow issues.
Impact on Organ Perfusion and Function
AFib’s effect on the heart can lead to less blood for organs. For example, less blood to the kidneys can mess up their job of filtering waste. Less blood to the brain can cause dizziness or confusion.
| Organ | Potential Effects of Reduced Perfusion |
|---|---|
| Brain | Dizziness, confusion, possible cognitive problems |
| Kidneys | Less ability to filter waste, risk of acute kidney injury |
| Heart | More work for the heart, risk of worse heart failure |
It’s key to understand how AFib affects blood flow. Knowing the risks helps doctors create better treatment plans. This can help manage AFib and its effects on the body.
Atrial Flutter vs. Atrial Fibrillation: Impact on Blood Pressure
It’s important to know the difference between atrial flutter and atrial fibrillation to manage blood pressure. Both are abnormal heart rhythms that start in the atria. But, they affect blood pressure differently because of their unique causes.
Distinguishing Between Atrial Flutter and AFib
Atrial flutter and atrial fibrillation are both heart rhythm problems. But, they show up differently on an electrocardiogram (ECG). Atrial flutter has a regular rhythm, like a sawtooth pattern, while atrial fibrillation has an irregular rhythm with no clear P waves.
Atrial flutter has more organized electrical activity than atrial fibrillation. This can affect blood pressure differently. “The difference between these arrhythmias is not just about words; it affects treatment,” a cardiology expert said.
Blood Pressure Patterns in Different Arrhythmias
Atrial flutter and atrial fibrillation both affect blood pressure in different ways. Atrial fibrillation can cause blood pressure to change because of irregular heartbeats. On the other hand, atrial flutter tends to have a more steady effect on blood pressure.
Studies show both conditions can cause hypotension (low blood pressure) because of reduced heart function. But, how often and why might vary. For example, atrial fibrillation with fast heartbeats can lead to bigger blood pressure swings.
In summary, atrial flutter and atrial fibrillation both impact blood pressure but in different ways. Knowing these differences is essential for the best care for patients with these heart rhythm issues.
Diagnostic Approaches for AFib with Hypotension
Diagnosing atrial fibrillation (AFib) with hypotension needs a detailed approach. We must understand the causes and create a good treatment plan. This involves several key tests to see how severe the condition is.
Essential Tests and Evaluations
To find AFib with hypotension, we use important tools. An electrocardiogram (ECG) is key to spot AFib’s irregular heart rhythms. We also check blood pressure to see how low it is.
We look at echocardiography to check the heart’s function and shape. And, we do blood tests to find out if there are other issues causing AFib or low blood pressure.
Monitoring Blood Pressure in AFib Patients
Keeping an eye on blood pressure is critical for AFib patients, even more so for those with low blood pressure. We use ambulatory blood pressure monitoring or home blood pressure monitoring. This gives us important info on blood pressure patterns.
We suggest that patients keep a blood pressure diary. This helps track their readings and can show trends that help in treatment.
By using these methods, we get a clear picture of the patient’s situation. Then, we can make a treatment plan that works for both AFib and low blood pressure.
Treatment Challenges: Managing Low Blood Pressure in AFib Patients
Atrial fibrillation (AFib) and low blood pressure together make treatment hard. AFib is a heart rhythm problem that can cause low blood pressure. It’s important to treat both conditions well to help patients.
Medication Considerations and Adjustments
Medicines are key in treating AFib but can also lower blood pressure too much. We must think about the medicines used and how they affect blood pressure. For example, some drugs can make blood pressure drop, so we might need to change the treatment plan.
To show how medicines affect blood pressure, let’s look at a table:
| Medication Type | Effect on Blood Pressure | Adjustment Strategy |
|---|---|---|
| Beta Blockers | Can lower blood pressure | Monitor blood pressure closely; adjust dosage as needed |
| Anti-arrhythmic Drugs | May cause hypotension | Consider alternative medications or adjust dosage |
| Calcium Channel Blockers | Can cause vasodilation, lowering blood pressure | Careful dosage adjustment; monitor for signs of hypotension |
Balancing Rate Control and Blood Pressure Management
It’s tricky to balance controlling heart rate and blood pressure in AFib patients. We need to make sure heart rate control doesn’t hurt blood pressure, and vice versa. This balance is key to keep vital organs well.
To find this balance, we look at many things. We consider the patient’s health, how bad AFib is, and other health issues. By looking at everything, we can make good treatment plans for both AFib and low blood pressure.
Multidisciplinary Approach to AFib-Related Hypotension Management
At Liv Hospital, we believe in working together to treat AFib and low blood pressure. A complete care plan for Atrial Fibrillation (AFib) and low blood pressure needs many healthcare experts.
A multidisciplinary team is essential for patients with AFib. Our team includes cardiologists, electrophysiologists, primary care doctors, and more. They all work together to create treatment plans that fit each patient.
Effective communication among healthcare providers is key. It helps make sure every part of a patient’s condition is covered. This way, we can make our patients’ lives better.
Our method at Liv Hospital includes:
- Comprehensive evaluations to find out why AFib and low blood pressure happen.
- Custom treatment plans that might include medicine, lifestyle changes, and procedures.
- Keeping a close eye on how the treatment is working and making changes as needed.
By using a multidisciplinary care strategy, we can handle the challenges of AFib and low blood pressure better. This helps improve how well our patients do.
Lifestyle Modifications for AFib Patients with Low Blood Pressure
We suggest a lifestyle change for AFib patients with low blood pressure. This change includes diet, exercise, and staying hydrated. It’s a way to improve their health and well-being.
Dietary Considerations
Eating a balanced diet is key for AFib patients with low blood pressure. We recommend foods rich in nutrients to help keep blood pressure healthy. Increasing salt intake under doctor’s advice can also help.
Drinking enough water is important. We advise against too much caffeine and alcohol. They can lead to dehydration and affect heart rhythm.
| Dietary Component | Recommendation |
|---|---|
| Salt Intake | Increase under medical supervision |
| Fluid Consumption | Adequate hydration, avoid excessive caffeine and alcohol |
| Nutrient-Rich Foods | Focus on balanced diet with fruits, vegetables, and whole grains |
Physical Activity Recommendations
Regular exercise is important for heart health. We suggest low-impact exercises like walking, swimming, or yoga. These activities improve circulation and reduce symptoms without straining the heart too much.
Always talk to a doctor before starting new exercises, if you have heart conditions.
Hydration and Other Daily Management Strategies
Drinking enough water is vital for blood pressure and health. We advise drinking water all day. Also, avoid standing for long and manage stress with relaxation techniques.
By making these lifestyle changes, AFib patients with low blood pressure can manage their condition better. This improves their quality of life.
Conclusion: Living Well with AFib and Managing Blood Pressure
Managing Atrial Fibrillation (AFib) and low blood pressure needs a team effort. At Liv Hospital, we use the latest methods and a team of experts. This ensures our patients get the best care possible.
Understanding AFib and its symptoms is key to living well with it. We work closely with our patients to help them manage their condition. This includes keeping blood pressure in check, which is vital for heart health.
With a solid care plan, people with AFib can live full and active lives. We stress the importance of teamwork. This includes patients, caregivers, and healthcare providers working together for the best results.
FAQ
What is atrial fibrillation and how does it affect blood pressure?
Atrial fibrillation (AFib) is a heart condition with an irregular and often rapid heart rate. This can lead to low blood pressure or hypotension. We look into how AFib affects blood pressure and its impact on health.
Can AFib cause low blood pressure?
Yes, AFib can cause low blood pressure. The irregular heart rate in AFib reduces cardiac output. This can lower blood pressure.
What are the symptoms of low blood pressure in AFib patients?
AFib patients with low blood pressure may feel dizzy, weak, or faint. It’s important to recognize these symptoms to get medical help quickly.
Is there a relationship between orthostatic hypotension and AFib?
Yes, there’s a strong link between orthostatic hypotension and AFib. Studies show that orthostatic hypotension increases the risk of AFib by 40%.
How does AFib affect blood perfusion and organ function?
AFib’s irregular heart rate can disrupt blood flow. This can lead to poor organ perfusion. Inadequate blood supply can harm organ function.
What is the difference between atrial flutter and AFib in terms of blood pressure?
Atrial flutter and AFib are both arrhythmias but affect blood pressure differently. Knowing the differences is key to effective management.
How is AFib with hypotension diagnosed?
Diagnosing AFib with hypotension involves several tests and evaluations. Using the right diagnostic tools is vital for treatment planning.
What are the treatment challenges for AFib patients with low blood pressure?
Treating AFib with low blood pressure is challenging. Medications for AFib can sometimes worsen hypotension, requiring careful adjustments.
How can lifestyle modifications help manage AFib and associated low blood pressure?
Lifestyle changes are key in managing AFib and low blood pressure. Eating a balanced diet and staying hydrated can help. Tailored physical activity also improves well-being.
What is the importance of a multidisciplinary approach in managing AFib-related hypotension?
Managing AFib and hypotension needs a team effort. At Liv Hospital, we emphasize collaborative care. Specialists from different fields work together to create personalized treatment plans.