Hematopoiesis is key for making blood cells. It turns stem cells into red blood cells, white blood cells, and platelets. This process is vital for adult health.
The human skeleton is where hematopoiesis happens in the bone marrow. It’s the main place for blood cell production.
Learning about hematopoiesis helps us understand blood disorders. It shows how important the bone marrow is for our health.
Hematopoiesis is key to our survival. It makes the blood cells we need for oxygen, fighting off infections, and stopping bleeding. This process keeps our blood cell count right, helping us face health challenges.
Hematopoiesis is about making blood cells. It happens in the red bone marrow of flat and long bones. The word comes from Greek, meaning “blood” and “making.”
This process creates all blood cell types, like red and white blood cells, and platelets. These cells come from special stem cells. These stem cells can turn into different blood cell types, keeping our blood fresh.
Hematopoiesis is essential for human survival. It makes:
Without it, we’d face serious health issues. Anemia, infections, and bleeding problems could occur. Hematopoiesis is carefully controlled to meet our body’s needs.
Knowing where hematopoiesis happens is important. In adults, it occurs in the red bone marrow. This is mainly in the pelvis, vertebrae, and long bone ends like the femur and humerus.
Hematopoietic stem cells are at the core of hematopoiesis. They are multipotent, meaning they can become all types of blood cells. These cells are key to the hematopoietic system, allowing for the constant creation of blood cells throughout our lives.
Hematopoietic stem cells can grow into different blood cell types. This is important for keeping the right balance of blood cells in our bodies.
They also have the power to self-renew. This means they can keep making more cells to replace old or damaged ones. This ability is essential for hematopoiesis to continue throughout our lives.
The self-renewal and differentiation of hematopoietic stem cells are controlled tightly. Many factors, both inside and outside the cell, help manage these processes. Knowing how these are regulated is key to understanding how does hematopoiesis occur and how it’s kept going in adults.
In adults, the site of hematopoiesis is mainly the bone marrow. This is where hematopoietic stem cells live and work. The bone marrow has a special environment that helps these stem cells renew and differentiate. It’s the main hematopoiesis location in adults.
Hematopoiesis is a complex process that creates different blood cells. It’s essential for our survival. Let’s explore how it happens.
Hematopoiesis starts with hematopoietic stem cells. These cells can grow and change into different blood cells. The process has several key steps:
The paths of differentiation in hematopoiesis are carefully controlled. They lead to the creation of various blood cells, including:
Knowing these paths helps us understand how blood cells are made. The bone marrow is key in supporting these processes with the right environment and factors.
By understanding hematopoiesis, we can learn more about blood cell production and related disorders.
The main place for making blood in adults is the bone marrow. This tissue is key for making blood cells. Blood cells carry oxygen, fight infections, and keep us healthy.
In adults, blood-making happens mainly in the bone marrow of specific bones. The bone marrow is a spongy tissue inside bones like the hips and thighbones. It makes red blood cells, white blood cells, and platelets.
The bone marrow is the main spot for blood-making because of its special structure and role. It has hematopoietic stem cells that can turn into any blood cell type. The bone marrow is where these stem cells grow and become blood cells. For more on what starts blood-making, check out this link.
In adults, certain bones with red bone marrow are key for blood-making. Red bone marrow is found in the:
These bones are where most blood cells are made in adults. The way red bone marrow is spread in these bones helps with efficient blood-making.
| Bone | Role in Hematopoiesis |
|---|---|
| Pelvis | Significant site for blood cell production |
| Vertebrae | Contains red marrow, contributing to hematopoiesis |
| Sternum | Important for producing blood cells |
| Ribs | Participates in hematopoiesis, though to a lesser extent than pelvis or vertebrae |
The bone marrow is home to a complex environment called the hematopoietic niche. It’s key for making blood cells. This niche isn’t just a place for blood cell production. It actively helps develop and work hematopoietic stem cells.
The bone marrow microenvironment has many parts that help with blood cell making. These include:
Cell talks in the hematopoietic niche are key for blood cell making. Hematopoietic stem cells talk to niche cells to keep their ability to renew and grow. Important talks include:
These talks show how complex the hematopoietic niche is. It plays a big role in blood cell making. Knowing how it works can help us understand blood disorders better.
As we grow, the place where blood cells are made changes. It moves from one spot to another before settling in the bone marrow. This change is key to understanding how our blood cell system grows.
The journey starts in the yolk sac early in our development. This first spot is important for making early blood cells. Later, as we grow, blood cell making moves to the liver.
The liver is key for blood cell making until we are almost born. We’ll look at this change in more detail in the table below.
| Developmental Stage | Primary Site of Hematopoiesis |
|---|---|
| Early Embryonic | Yolk Sac |
| Fetal Development | Liver |
| Late Fetal to Adult | Bone Marrow |
As we get closer to being born and grow into adults, blood cell making moves to the bone marrow. The bone marrow is the main place for making blood cells in adults. It helps make all types of blood cells for the rest of our lives.
This change is important for a stable blood cell system. The bone marrow’s special environment helps with blood cell making. It keeps our blood cell system working well.
In summary, hematopoiesis changes from the yolk sac to the liver and then to the bone marrow. Knowing about these changes helps us understand how our blood cell system matures.
Every day, our body makes about 100 billion new blood cells. This shows how amazing the process of making blood cells is. It happens mainly in the bone marrow of adults.
Hematopoiesis is the term for making blood cells. Knowing where it happens helps us see how important it is for our health.
The number of blood cells made daily is hard to imagine. An average adult makes about 100 billion blood cells every day. This includes red, white, and platelet cells, each with its own job and life span.
This process is very precise. It changes based on what the body needs. For example, when we get sick, the body makes more white blood cells to fight off the illness.
Blood cells live for different lengths of time. This helps keep our body balanced. For example, red blood cells last about 120 days.
On the other hand, white blood cells can live anywhere from a few hours to years. Knowing how long each type lives is key to understanding blood disorders.
In summary, making blood cells every day is a remarkable process. It shows how complex and efficient our bodies are. By understanding where and how hematopoiesis happens, we can appreciate the amazing ways our bodies keep us alive.
Hematopoiesis is the process of making blood cells. It’s controlled by many factors inside and outside the cells. This ensures the right amount and type of blood cells are made.
Inside the cells, certain factors like transcription factors and signaling pathways are key. They help hematopoietic stem cells grow and change into different blood cells. For example, RUNX1 and GATA2 are important for these stem cells.
Signaling pathways like Wnt/β-catenin and Notch also play a big role. They work with transcription factors to guide the development of blood cells.
| Transcription Factor | Role in Hematopoiesis |
|---|---|
| RUNX1 | Essential for hematopoietic stem cell development and maintenance |
| GATA2 | Critical for the proliferation and survival of hematopoietic stem cells |
| PU.1 | Regulates the development of myeloid and lymphoid lineages |
Outside the cells, the bone marrow environment and systemic signals also matter. The bone marrow supports the growth and function of blood cells. Systemic signals, like cytokines and growth factors, help control how blood cells grow and survive.
For instance, erythropoietin helps make red blood cells. Granulocyte-colony stimulating factor (G-CSF) boosts the production of neutrophils.
Learning about how hematopoiesis is regulated helps us understand blood cell creation. It also guides the development of treatments for blood-related diseases.
Hematopoiesis is key in diagnosing and treating blood disorders. It mainly happens in the bone marrow of adults. Knowing how it works helps us understand blood cell production and its problems.
Diagnosing blood disorders involves several steps. Bone marrow biopsies are a key tool. They let doctors see where hematopoiesis happens. Genetic testing also plays a big role, finding specific problems in blood cell production.
The table below shows common ways to diagnose blood disorders:
| Diagnostic Method | Description | Clinical Utility |
|---|---|---|
| Bone Marrow Biopsy | Examination of bone marrow tissue | Essential for diagnosing various blood cancers and disorders |
| Genetic Testing | Identification of genetic mutations | Critical for understanding inherited blood disorders |
| Blood Cell Count | Quantification of different blood cell types | Helps in diagnosing anemia, infection, and leukemia |
Treatments for blood disorders have gotten better. Bone marrow transplantation can save lives. Targeted therapies also help by focusing on specific problems in blood cells.
Knowing where and how hematopoiesis happens is key for new treatments. Research into the bone marrow and its factors is promising. It could lead to new ways to treat blood disorders.
By learning more about hematopoiesis, we can improve how we diagnose and treat blood disorders. This will help patients get better care.
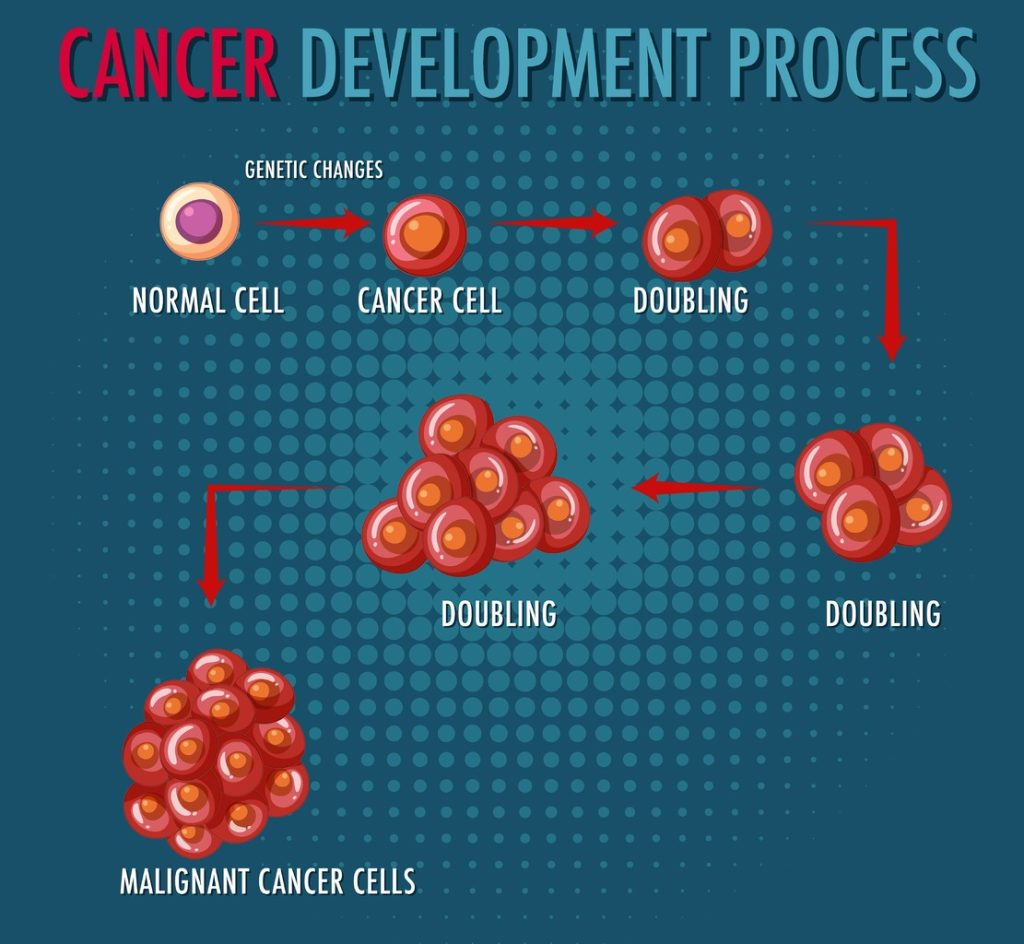
It’s important to know about the problems in hematopoiesis to diagnose and treat diseases. Hematopoiesis is how our body makes blood cells. It’s a complex process that needs to work right for our health.
We’ll look at two main issues: problems with hematopoietic stem cells and diseases that harm the bone marrow. Both are key to making blood cells properly.
Problems with hematopoietic stem cells can be serious. These cells make all blood cells. If they’re not working right, it can cause big health problems.
These conditions show how important healthy stem cells are for making blood cells.
The bone marrow’s environment is key for blood cell making. Diseases that harm this environment can stop blood cell production. Examples include:
Knowing about these diseases helps us find better treatments for hematopoietic problems.
In summary, problems with hematopoietic stem cells and bone marrow diseases are big issues in hematopoiesis. By understanding these, we can improve diagnosis and treatment, helping patients get better.
Hematopoiesis is the process of making blood cells. It’s essential for our bodies and happens all our lives. Knowing how it works helps us understand health and sickness.
In adults, this process mainly happens in the bone marrow. Here, stem cells turn into different blood cells. This complex process keeps our blood flowing, fighting off infections, and stopping bleeding.
The bone marrow is key to making blood. Keeping it healthy is vital for our bodies. Studying hematopoiesis helps us find and treat blood-related problems, even Liv Hospital states that.
Learning about hematopoiesis shows us how amazing our bodies are. They keep making blood cells to keep us healthy.
Hematopoiesis is the process of making blood cells. In adults, it mainly happens in the bone marrow. This is in the red bone marrow of flat and long bones.
It’s the making of blood cells. This includes red blood cells, white blood cells, and platelets. They come from stem cells in the bone marrow.
In adults, it happens in the bone marrow. This is mainly in the pelvis, vertebrae, and sternum.
These stem cells are key to making blood cells. They can grow, renew themselves, and turn into different blood cells.
It starts with stem cells turning into blood cells. This goes through many stages. It ends with the production of mature blood cells.
The bone marrow microenvironment supports stem cells. It helps them grow and turn into different blood cells. This is vital for hematopoiesis.
It’s controlled by both inside and outside factors. Inside factors are in the cells themselves. Outside factors include the bone marrow environment. They work together to manage blood cell creation.
Knowing about hematopoiesis helps in diagnosing and treating blood disorders. It also guides treatments.
Problems with stem cells or the bone marrow can cause issues. This shows why keeping the hematopoietic system healthy is important.
At first, it happens in the yolk sac during fetal development. Then, it moves to the liver and later to the bone marrow. It stays there in adults.
It produces billions of blood cells every day. These cells have different lifespans. They are essential for keeping the body’s blood cell count right.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us