Last Updated on October 31, 2025 by
Chemotherapy is a key treatment for many cancers. It uses strong medicines to harm and kill fast-growing cancer cells. We count on chemotherapy to treat cancers, often with other treatments too how effective is chemotherapy.
Knowing what chemotherapy does to cancer helps patients and doctors. It kills or slows down cancer cells. How well it works depends on the cancer type.
For many, chemotherapy is a big part of their treatment. It helps extend life and improve life quality. We’ll look at the good and bad sides of chemotherapy in fighting cancer.
Key Takeaways
- Chemotherapy is a widely used treatment for various types of cancer.
- It works by killing or stopping the growth of rapidly dividing cancer cells.
- The effectiveness of chemotherapy depends on the type of cancer and other factors.
- Chemotherapy can be used alone or in combination with other therapies.
- Understanding chemotherapy’s mechanism and impact is key for patients and healthcare providers.
Understanding Chemotherapy and Its Mechanism of Action
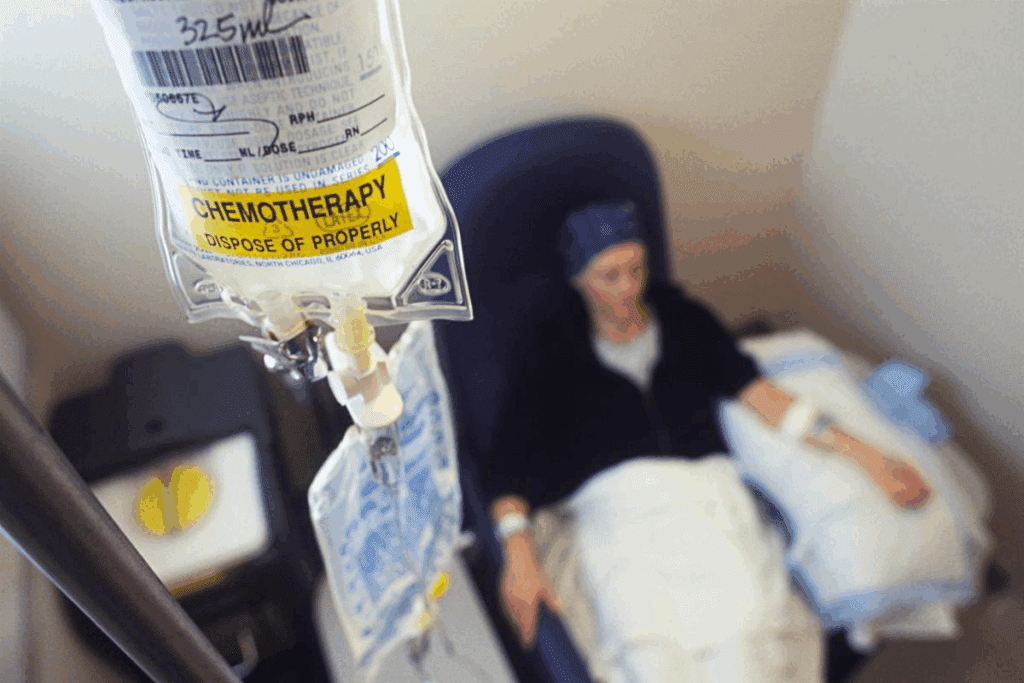
It’s important to know how chemotherapy works to understand its role in cancer treatment. Chemotherapy uses drugs to kill cancer cells or stop them from growing. It’s a key part of fighting cancer, often used with surgery and radiation therapy.
Definition and Basic Principles of Chemotherapy
Chemotherapy uses chemicals to treat diseases, mainly cancer. It works by targeting cells that grow fast, like most cancer cells. By stopping the cell cycle, chemotherapy drugs can kill cancer cells or stop them from multiplying.
The cell cycle is how cells grow, copy their DNA, and split into two. Chemotherapy drugs hit cancer cells at different stages of this cycle. This makes them good at fighting cancer cells.
How Chemotherapy Targets Rapidly Dividing Cells
Chemotherapy is great at fighting cancer cells because they grow fast. By focusing on dividing cells, chemotherapy can cut down cancer cell numbers. Different drugs target cells at different stages, attacking cancer cells from all sides.
Some drugs damage cancer cells’ DNA, stopping them from making copies. Others mess with cell division, stopping cancer cells from growing. This targeted approach makes chemotherapy a strong cancer treatment.
Knowing how chemotherapy works helps us see its value in cancer treatment. Its ability to target fast-growing cells is key to fighting cancer.
The Science Behind How Chemotherapy Kills Cancer Cells
Chemotherapy works by affecting how cancer cells divide and make DNA. It’s a key part of cancer treatment. It targets cells that grow fast, like most cancer cells.
Chemotherapy works in several ways:

Disruption of DNA Replication
Chemotherapy drugs harm the DNA of cancer cells, stopping them from making more. They do this by:
- Stopping the making of new DNA strands
- Creating cross-links in DNA that stop cell division
- Directly damaging DNA, causing cell death
Blocking Cell Division Processes
Chemotherapy also stops cell division by targeting how cells divide. It does this by:
- Disrupting the making of microtubules, key for cell division
- Stopping enzymes needed for cell cycle progression
This stops cancer cells from growing and multiplying.
Triggering Apoptosis (Programmed Cell Death)
Chemotherapy also kills cancer cells by starting apoptosis, or programmed cell death. Apoptosis is how the body gets rid of damaged or unwanted cells.
Chemotherapy starts apoptosis by:
- Causing DNA damage that can’t be fixed
- Turning on proteins that help cells die
Turning off proteins that protect cells from dying
This makes sure damaged cancer cells are removed. It helps shrink tumors and slow the disease.
In summary, chemotherapy kills cancer cells in many ways. It stops DNA replication, blocks cell division, and starts apoptosis. Knowing how it works helps us see why it’s so important in cancer treatment.
Measuring How Effective Is Chemotherapy Across Different Cancer Types
Chemotherapy works differently for each type of cancer. Its success depends on the cancer type, its stage, and the patient’s health. Knowing how chemotherapy affects different cancers is key to creating effective treatment plans.
Effectiveness in Blood Cancers (Leukemia, Lymphoma)
Blood cancers like leukemia and lymphoma often respond well to chemotherapy. Leukemia has seen big improvements in treatment, thanks to chemotherapy, mainly in kids. Lymphoma, affecting the immune system, also sees high cure rates with chemotherapy. This is because cancer cells in blood cancers divide quickly, making them easier to target.
Effectiveness in Solid Tumors (Breast, Lung, Colorectal)
Solid tumors, such as breast, lung, and colorectal cancers, are a different story. Chemotherapy is a common treatment but its success varies. For example, breast cancer without hormone receptors or with specific genetic markers may respond well. Chemotherapy is also used in lung cancer and colorectal cancer, often after surgery. The success of chemotherapy in these cancers depends on the cancer’s stage and specific traits.
Cancers Most and Least Responsive to Chemotherapy
Some cancers, like certain leukemia, lymphoma, and testicular cancer, respond very well to chemotherapy. Others, like pancreatic cancer and some brain tumors, are less responsive. The reasons for this vary, including the cancer’s biology and genetics. Understanding these factors helps improve chemotherapy’s effectiveness.
Looking at how chemotherapy works for different cancers helps us see its strengths and weaknesses. This knowledge helps doctors tailor treatments for each patient, leading to better results.
Statistical Evidence: Survival Rates and Treatment Outcomes
Statistical evidence is key to understanding how chemotherapy affects survival rates in different cancers. By looking at data from studies and trials, we learn how well chemotherapy works. This helps us see how it improves patient results.
Breast Cancer Survival Statistics
Breast cancer is a big problem for women worldwide. Chemotherapy has greatly helped breast cancer patients live longer. Studies show that chemotherapy has boosted the one-year survival rate to 51 percent. This is up from 38 percent for those without chemotherapy.
These gains come from better chemotherapy methods and new targeted treatments. Tailoring treatments to each patient helps doctors get the most out of chemotherapy.
Prostate Cancer Treatment Outcomes
Prostate cancer is a common issue for men. Chemotherapy is used for advanced prostate cancer. Research shows it can also help patients with metastatic prostate cancer live longer.
For example, chemotherapy patients lived for 30 months with a 61.6 percent survival rate. This is compared to 56 percent for those without chemotherapy. These numbers highlight chemotherapy’s role in fighting prostate cancer.
Interpreting Cancer Treatment Statistics
Grasping cancer treatment stats requires looking at many factors. These include the cancer type, its stage, and the patient’s health. By understanding these, doctors and patients can choose the best treatments.
It’s also vital to recognize the data’s limits and possible biases. This way, we can use the stats to better care for patients.
Factors That Influence Chemotherapy Effectiveness
It’s key to know what affects how well chemotherapy works. Chemotherapy is a big part of fighting cancer. But, it doesn’t work the same for everyone.
Cancer Type and Stage at Diagnosis
The type and stage of cancer matter a lot. Different cancers react differently to treatment. For example, some blood cancers and lymphomas do well with chemotherapy. But, some solid tumors might not respond as well.
Cancer stage is also very important. Early cancers are usually easier to treat and have better results with chemotherapy. This is not as true for cancers that are more advanced.
Individual Patient Factors
Things like overall health, age, and other health issues can change how well chemotherapy works. People who are healthier and have fewer health problems usually do better with chemotherapy.
- Age can affect how well someone can handle chemotherapy, with older people facing more challenges.
- Having other health issues can make it harder for the body to get better after chemotherapy.
Genetic and Molecular Markers
Genetic and molecular markers are getting more attention in predicting how well chemotherapy will work. Some genetic changes can make cancer cells more or less likely to respond to certain treatments.
Personalized medicine is making chemotherapy more effective. It uses genetic and molecular tests to create treatments that fit each patient’s cancer.
Knowing these factors helps doctors predict who will benefit most from chemotherapy. They can then make treatment plans that are more likely to work.
Collateral Damage: How Chemotherapy Affects Healthy Cells
Chemotherapy targets fast-growing cancer cells but also harms healthy cells that grow quickly. This damage causes side effects that can greatly affect a patient’s life during and after treatment.
Impact on Bone Marrow and Blood Cells
The bone marrow is key because it makes blood cells. But, because it has fast-growing cells, chemotherapy can lower blood cell counts. This can lead to anemia, more infections, and bleeding problems.
| Condition | Cause | Effect |
| Anemia | Reduced red blood cell production | Fatigue, weakness |
| Neutropenia | Low white blood cell count | Increased infection risk |
| Thrombocytopenia | Decreased platelet count | Bleeding, bruising |
Effects on Gastrointestinal Tract
The GI tract is also affected by chemotherapy. Its fast-growing cells make it vulnerable. Side effects include nausea, vomiting, diarrhea, and mucositis.
“Chemotherapy-induced nausea and vomiting are among the most distressing side effects for patients undergoing cancer treatment.”
NCCN Guidelines for Antiemetics
Hair Follicles and Other Rapidly Dividing Tissues
Hair loss is a common side effect of chemotherapy. It affects hair follicles, where cells grow fast. Other tissues, like the mouth lining and reproductive system, can also be impacted.
It’s important to understand how chemotherapy affects healthy cells. This knowledge helps manage side effects and improve patient outcomes. By recognizing the damage, healthcare providers can find ways to lessen these effects. This improves the quality of life for patients going through cancer treatment.
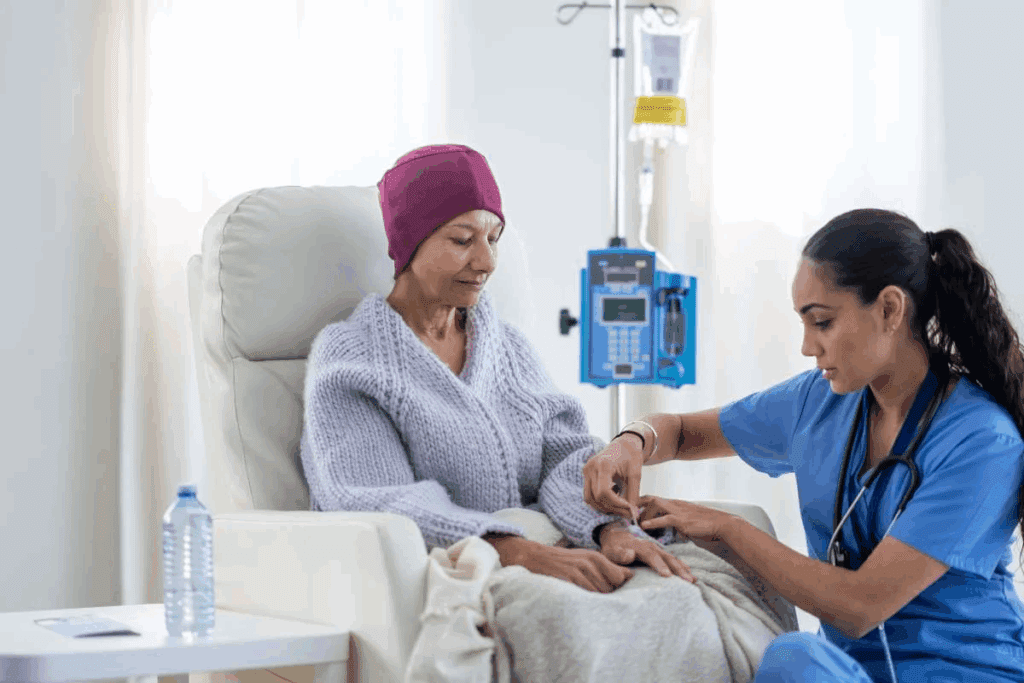
Managing and Mitigating Chemotherapy Side Effects
Managing chemotherapy side effects is vital for better patient outcomes and quality of life. Chemotherapy is a key part of cancer treatment but can have tough side effects. We will look at ways to manage these side effects to improve care.
Common Side Effects and Their Management
Chemotherapy side effects vary among patients, but common ones include nausea, hair loss, and fatigue. It’s important to manage these side effects to keep patients comfortable and on track with treatment.
- Nausea and Vomiting: Antiemetic medications are often prescribed to prevent or reduce nausea and vomiting.
- Hair Loss: While not preventable, scalp cooling devices may help reduce hair loss in some patients.
- Fatigue: Rest, nutrition counseling, and gentle exercise can help manage fatigue.
Long-term Effects of Chemotherapy
Some chemotherapy side effects can last long after treatment ends. It’s important to understand these long-term effects for complete care.
- Cardiac Issues: Certain chemotherapy agents can lead to long-term cardiac problems.
- Secondary Cancers: There is a small risk of developing secondary cancers after chemotherapy.
- Neurological Effects: Some patients may experience neuropathy or cognitive changes.
Quality of Life Considerations
Keeping quality of life in mind is key in cancer care. By effectively managing side effects, we can help patients stay on their treatment path with less disruption to their daily lives.
Chemotherapy Resistance: When Cancer Cells Fight Back
Chemotherapy is a common treatment for many cancers. But, cancer cells can develop resistance, making treatment less effective. This resistance makes it hard to achieve the best results.
Mechanisms of Resistance Development
Cancer cells can resist chemotherapy in several ways. Genetic changes can make the drug less effective. Cancer cells also activate survival pathways to fight off chemotherapy.
Genetic mutations are key in developing resistance. These changes can happen naturally or because of chemotherapy. For example, mutations in the p53 gene can make cells less responsive to chemotherapy.
Overcoming Resistance Strategies
To beat resistance, we use different strategies. Combination therapies use multiple drugs to target cancer in various ways. Targeted therapies aim at specific genetic changes in cancer cells.
We’re also looking into new treatments. Nanotechnology-based drug delivery systems might help get drugs directly to cancer cells. This could help overcome some resistance.
Predicting and Monitoring Resistance
It’s important to predict and monitor resistance. Biomarkers help us know if a treatment will work. Liquid biopsies might help track resistance during treatment.
Understanding resistance and finding ways to overcome it is key. Research is ongoing to improve treatments. This will help us give better care to cancer patients.
Combination Therapies: Enhancing Chemotherapy Effectiveness
Using chemotherapy with other treatments is a key strategy to fight cancer better. It combines different ways to attack cancer cells. This makes treatments more effective, leading to better patient outcomes and longer lives.
Chemotherapy with Radiation
Chemotherapy paired with radiation therapy is a common method. It works well for some cancers that don’t respond to one treatment alone. This combo can kill more tumor cells, lower the chance of cancer coming back, and boost survival chances.
Benefits of combining chemotherapy with radiation include:
- Enhanced local control of tumors
- Potential for organ preservation
- Improved survival rates in certain cancer types
Chemotherapy with Surgery
Chemotherapy can be used before or after surgery. Before surgery, it makes tumors smaller. After, it kills any cancer cells left behind, lowering the chance of cancer coming back.
The advantages of combining chemotherapy with surgery include:
- Improved surgical outcomes due to tumor shrinkage
- Reduced risk of cancer recurrence
- Potential for less extensive surgery
Chemotherapy with Targeted Therapies
Chemotherapy paired with targeted therapies is a big step forward in cancer treatment. Targeted therapies aim at specific cancer growth points, adding to chemotherapy’s broad attack.
Key benefits of combining chemotherapy with targeted therapies:
- Enhanced specificity towards cancer cells
- Potential for reduced side effects compared to chemotherapy alone
- Improved treatment outcomes through a multi-faceted approach
By using these combination therapies, we can make chemotherapy more effective. This gives patients more detailed and tailored treatment plans.
Advances in Chemotherapy: Precision and Personalized Approaches
Recent breakthroughs in chemotherapy are changing cancer treatment. They offer more precise and personalized options. These changes are making treatments more effective and tailored to each patient’s needs.
Targeted Chemotherapy Agents
One big advance is the creation of targeted agents. Unlike old chemotherapy, these new drugs only hit cancer cells, not healthy ones. For example, drugs like trastuzumab (Herceptin) target HER2 protein in some breast cancers. This makes treatments better and cuts down on side effects.
Key benefits of targeted chemotherapy agents include:
- Improved efficacy by directly targeting cancer cells
- Reduced side effects compared to traditional chemotherapy
- Potential for better treatment outcomes in specific cancer types
Genetic Testing and Personalized Treatment Plans
Genetic testing is key in making personalized treatment plans. It looks at a patient’s genes and their cancer’s genes. This helps doctors find the best treatments. For instance, genetic tests can find BRCA1 and BRCA2 mutations linked to breast and ovarian cancers. People with these mutations might get special targeted therapies.
The integration of genetic testing into treatment planning allows for:
- More accurate diagnosis and prognosis
- Tailored treatment plans based on genetic profiles
- Potential for preventive measures in high-risk individuals
Nanotechnology and Drug Delivery Innovations
Nanotechnology is making drug delivery systems better for chemotherapy. It uses nanoparticles to make drugs more stable and targeted. This could make chemotherapy more effective and reduce side effects.
Innovations in drug delivery include:
- Nanoparticle-based delivery systems
- Thermosensitive liposomes that release drugs in response to heat
- Implantable devices that deliver chemotherapy directly to tumor sites
As we keep improving, the future of chemotherapy looks bright. We’re heading towards even more effective and personalized treatments.
The Future of Cancer Cell Destruction: Beyond Traditional Chemotherapy
New ways to fight cancer are being discovered. Immunotherapy and other treatments are changing how we treat cancer. This brings hope to people all over the world.
Immunotherapy Approaches
Immunotherapy uses the body’s immune system to fight cancer. It’s different from traditional chemotherapy, which targets fast-growing cells. Immunotherapy boosts the immune system to attack cancer cells.
There are many types of immunotherapy being studied. These include:
- CAR-T cell therapy, which changes a patient’s T cells to attack cancer cells.
- Checkpoint inhibitors, which help the immune system fight cancer cells better.
- Cancer vaccines, which help the immune system recognize and fight cancer cells.
Emerging Non-Chemotherapy Treatments
New treatments are being explored, like targeted therapies and oncolytic virus therapy. These treatments aim to kill cancer cells while protecting healthy tissues.
Nanotechnology is also being researched. It involves using nanoparticles to deliver drugs directly to cancer cells. This could make treatments more effective and reduce side effects.
Combining Old and New Approaches
New treatments are being combined with traditional chemotherapy. This creates personalized treatment plans for patients. It aims to offer the best results possible.
For example, mixing immunotherapy with chemotherapy can improve treatment results. This combination helps overcome chemotherapy’s limitations, like resistance and side effects.
As we look to the future, combining new and old treatments will continue to evolve. This brings new hope to cancer patients everywhere.
Conclusion: Balancing the Benefits and Limitations of Chemotherapy
We’ve looked into how chemotherapy fights cancer, its success in different cancers, and what makes it work. It’s a key treatment for many cancers, killing fast-growing cancer cells and helping patients get better.
But, we know chemotherapy isn’t perfect. It can harm healthy cells too, causing side effects that make life hard for patients. It’s important to manage these side effects and prevent long-term damage.
Every patient is different, so chemotherapy must be tailored to each person. New treatments like targeted therapies and precision medicine are making chemotherapy better. They help fight cancer more effectively and reduce side effects.
As we keep improving cancer treatment, it’s vital to know both the good and bad of chemotherapy. Mixing chemotherapy with other treatments like immunotherapy can make care better. This way, we can help patients live better lives.
FAQ
What is chemotherapy and how does it work?
Chemotherapy is a treatment for cancer that uses drugs. These drugs target cells that grow and multiply quickly. This helps kill cancer cells.
How effective is chemotherapy in killing cancer cells?
Chemotherapy is very good at killing cancer cells. It works best in blood cancers like leukemia and lymphoma. It can also help improve survival rates for many cancers.
Does chemotherapy kill healthy cells?
Yes, chemotherapy can harm healthy cells too. This is because it targets cells that divide quickly. This can cause side effects in areas like the bone marrow and hair follicles.
What factors influence the effectiveness of chemotherapy?
Several things affect how well chemotherapy works. These include the type and stage of cancer, the patient’s health, and genetic markers.
Can cancer cells develop resistance to chemotherapy?
Yes, cancer cells can become resistant to chemotherapy. But, using combination therapies and targeted agents can help fight this resistance.
How can chemotherapy side effects be managed?
There are many ways to manage side effects from chemotherapy. This includes using medications, making lifestyle changes, and getting supportive care. These steps can help improve a patient’s quality of life during treatment.
What are the advances in chemotherapy?
Chemotherapy is getting better thanks to new advances. These include targeted agents, genetic testing, and better ways to deliver drugs. These improvements make treatment more precise and tailored to each patient.
Is chemotherapy the only treatment option for cancer?
No, chemotherapy is often used with other treatments like surgery and radiation. New approaches like immunotherapy are also changing how we treat cancer.
How does chemotherapy work with other treatments?
Chemotherapy can be used alongside other treatments to make them more effective. This combination can improve patient outcomes and treatment success.
What is the future of cancer treatment beyond traditional chemotherapy?
The future of cancer treatment looks promising. New approaches like immunotherapy and targeted therapies are emerging. These offer hope for better treatment outcomes and improved patient care.
References
Government Health Resource. (2025). How Effective Is Chemotherapy at Killing Cancer Cells. Retrieved from https://ashpublications.org/blood/article/89/6/1845/139072/Apoptosis-and-the-Dilemma-of-Cancer-Chemotherapy)





