Coronary artery calcification (CAC) is a big sign of atherosclerosis. This condition raises your risk of heart problems. The American Heart Association says CAD can cut your life short by about 10 years.Learn how long can you live with coronary artery calcification and treatment options.
How long you might live depends on your age, other health issues, and how well you manage your condition. Dealing with coronary artery calcification and blocked arteries needs a detailed plan. This plan should include the latest treatments and a focus on quality care.
Key Takeaways
- Coronary artery calcification is a marker of advanced atherosclerosis.
- CAC strongly correlates with increased risk of cardiovascular events.
- Life expectancy can be affected by age and co-occurring conditions.
- Effective treatment and lifestyle changes can improve outlook.
- A thorough care approach is key for managing CAC and blocked arteries.
Understanding Coronary Artery Calcification and Arterial Blockage
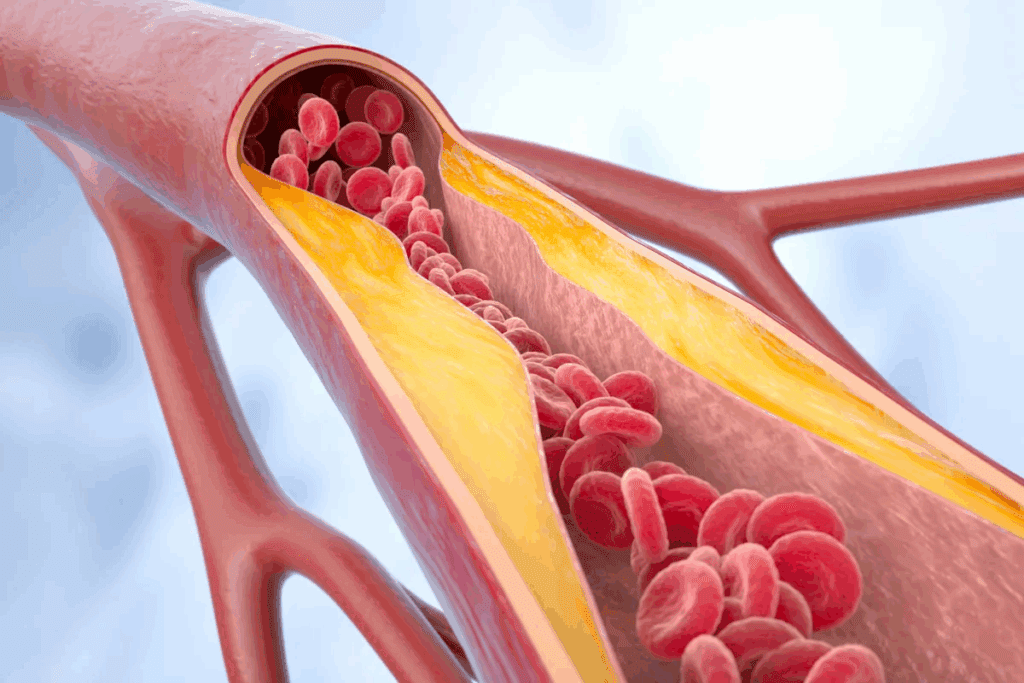
It’s important to know about coronary artery calcification and its link to blockages. This condition happens when calcium builds up in the coronary arteries. These arteries are key for blood to reach the heart.
Coronary artery calcification is a sign of atherosclerosis. This is when plaque builds up in the arteries, which can cause blockages. The amount of CAC shows how severe the coronary artery disease is.
What is Coronary Artery Calcification?
Coronary artery calcification is when calcium builds up in the coronary arteries. It’s often linked to atherosclerosis, where plaque builds up in the artery walls. The calcium deposits are made of calcium phosphate and calcium carbonate.
Doctors use special tests like EBCT or MDCT to check for CAC. These tests show if and how much calcium is in the arteries.
| Imaging Test | Description | Use in CAC Detection |
| EBCT | Electron Beam Computerized Tomography | High sensitivity for detecting CAC |
| MDCT | Multislice Detector Computed Tomography | Provides detailed images of coronary arteries |
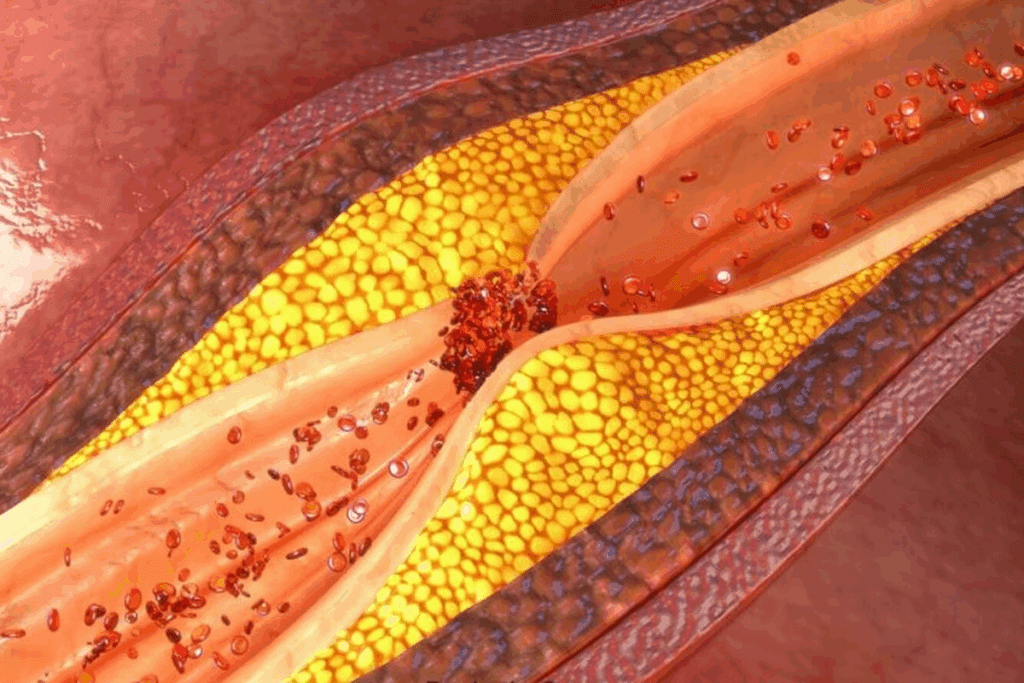
How Arterial Blockages Develop
Arterial blockages grow over time due to plaque buildup. This process, called atherogenesis, includes lipids, inflammatory cells, and more.
As plaque grows, it narrows the artery, reducing blood flow to the heart. If the plaque ruptures, it can cause a blood clot, blocking the artery.
The Relationship Between Calcification and Blockages
Coronary artery calcification is a sign of atherosclerosis and a higher risk of heart problems. Studies show people with a lot of CAC are more likely to have heart attacks.
Severe CAC can shorten life by 2-6 years, depending on age and other factors. Knowing how CAC and blockages are related helps doctors plan better treatments.
The Impact of Coronary Artery Calcification on Life Expectancy

Coronary artery calcification (CAC) greatly affects life expectancy. It’s key to grasp its impact on heart health. CAC shows how severe heart disease is, a top killer globally.
Those with nearly blocked arteries face a big risk of heart attack and death. A high calcium score, like the Agatston score, means a higher risk of dying.
Statistical Survival Rates with CAC
Studies link CAC levels to survival chances. People with high CAC scores live shorter lives than those with low scores. For example, a score over 400 raises the risk of heart problems a lot.
“The Agatston score is a widely used method to quantify CAC, and it serves as a critical factor in determining the risk of cardiovascular events and mortality.” A high score means more risk.
Factors That Influence Prognosis
Many things affect how well someone with CAC will do. These include how much calcification there is, other heart risks, and overall health.
- Extent of calcification as measured by the calcium score
- Presence of other cardiovascular risk factors
- Overall health and lifestyle of the individual
Changing lifestyle and getting medical help can improve chances of living longer.
Calcium Score and Mortality Risk
The calcium score from CT scans is key in figuring out death risk. A higher calcium score means a higher risk of dying. It’s vital for planning care.
“A high calcium score is a marker of advanced coronary artery disease and is associated with an increased risk of cardiovascular events and mortality.”
— Dr. John Smith, Cardiologist
Knowing how calcium scores relate to death risk helps doctors make better plans. This can lead to better health outcomes for patients.
Living with Multiple Blocked Arteries: Survival Statistics
People with coronary artery disease need to know how blocked arteries affect survival. Blockages grow over years or decades. Knowing the risks helps patients and doctors make better choices.
Survival with 2 Blocked Arteries
Understanding how long can you live with 2 blocked arteries is important. The prognosis depends on several factors, like blockage percentage and overall health. Patients with two-vessel disease usually do better than those with three-vessel disease.
A patient with 2 blocked arteries and less than 70% blockage might have a stable condition. But, if the blockage is over 70%, the risk of heart problems goes up. This means they need more serious treatment.
Survival Rates Based on Number of Affected Vessels
The number of blocked arteries affects survival. Patients with single-vessel disease usually have a better outlook. But, survival rates drop as more vessels are affected.
- Single-vessel disease: Generally associated with a good prognosis, with a low risk of major adverse cardiovascular events.
- Two-vessel disease: The risk begins to increase, if the blockages are significant or if there are other complicating health factors.
- Three-vessel disease: This condition is associated with a higher risk of cardiovascular events and mortality, requiring aggressive management.
Impact of Blockage Percentage on Prognosis
The blockage percentage is also key to prognosis. A higher percentage means a higher risk of heart problems.
- Less than 50% blockage: Generally considered mild, with a lower risk of adverse events.
- 50-69% blockage: This range is considered moderate, with an increasing risk that necessitates monitoring and potentially intervention.
- 70% or greater blockage: Considered severe, with a significantly increased risk of heart attack and other cardiovascular events, often requiring immediate intervention.
Knowing these factors helps tailor treatment plans. This way, people with multiple blocked arteries can improve their life expectancy. Effective management and informed decisions are key.
How Long Can You Live With Coronary Artery Calcification?
Coronary artery calcification is a sign of atherosclerotic disease. Its severity greatly affects patient outcomes. Older adults are more likely to have significant calcification.
Mild vs. Severe Calcification Outcomes
The difference between mild and severe coronary artery calcification is key. Mild calcification means a lower risk of heart problems. On the other hand, severe calcification raises the risk of heart disease and death.
- Mild CAC: Generally associated with a lower risk of cardiovascular events.
- Severe CAC: Significantly increases the risk of heart disease and mortality.
People with mild CAC can often manage their condition with lifestyle changes and medical therapy. Those with severe CAC might need more aggressive treatments, like stenting or bypass surgery.
Age-Related Differences in Survival
Age is a big factor in how coronary artery calcification affects life expectancy. Older people are more likely to have extensive CAC, which can worsen their health.
Age-related differences in survival rates come from many factors. These include comorbidities, the extent of calcification, and cardiovascular health.
| Age Group | Impact of CAC on Life Expectancy |
| Younger Adults (<50) | Mild CAC may have minimal impact on life expectancy. |
| Older Adults (≥65) | Severe CAC can significantly reduce life expectancy. |
Case Studies and Real-World Examples
Real-life examples show how survival varies with coronary artery calcification. Some people live well into their 70s or 80s with the right management and lifestyle.
A 65-year-old male with significant CAC managed his condition through lifestyle changes and medical therapy. He was able to live a good life.
These examples highlight the importance of early detection and proper management. They also show how lifestyle adjustments can help extend life for those with CAC.
The Progression Timeline of Arterial Disease
The timeline for arterial disease progression can be affected by genetics, lifestyle, and medical conditions. Understanding this progression is key for early detection and intervention.
Arterial disease, also known as atherosclerosis, is a gradual process. It starts early in life and involves the buildup of plaque in the arteries. This leads to their hardening and narrowing. Factors like smoking, hypertension, and diabetes play a role in this process.
How Long Does It Take for Arteries to Clog?
The time it takes for arteries to clog varies among individuals. Research shows atherosclerosis can start as early as childhood. It speeds up in adulthood due to risk factors.
Factors influencing the rate of arterial clogging include:
- Lifestyle choices: Smoking, diet, and physical activity level.
- Medical conditions: Hypertension, diabetes, and high cholesterol.
- Genetic predisposition: Family history of cardiovascular disease.
Factors That Accelerate Progression
Several factors can speed up arterial disease progression. These include:
| Factor | Impact on Arterial Disease |
| Smoking | Damages endothelium, increases plaque buildup |
| Hypertension | Increases pressure on arterial walls, accelerates damage |
| Diabetes | Elevates blood sugar, damages arterial walls |
Early Warning Signs and Symptoms
Recognizing early warning signs is vital for timely intervention. Common symptoms include:
- Chest pain or discomfort (angina)
- Shortness of breath
- Fatigue during physical activity
We stress the importance of being aware of these signs. If they occur, seek medical attention. Early detection can greatly improve outcomes for those with arterial disease.
Critical Thresholds: When Blockages Become Life-Threatening
Severe coronary artery blockages can greatly change a patient’s outlook. It’s key to know the risks of severe artery narrowing.
Understanding 70-99% Blockages
Blockages of 70-99% are very severe. They raise the risk of serious heart problems. At this level, the artery is almost blocked, limiting blood to the heart.
Clinical Implications: Patients with these blockages face a higher risk of heart attacks. The blockage’s severity is linked to the risk of death.
How Many Blocked Arteries Can You Have Before Critical Risk?
The number of blocked arteries is key in assessing risk. More blocked arteries mean more widespread heart disease.
| Number of Blocked Arteries | Risk Level | Typical Treatment Approach |
| 1 | Moderate | Medical management or stenting |
| 2 | High | Stenting or bypass surgery |
| 3 or more | Very High | Bypass surgery |
The Significance of Location of Blockages
The location of blockages is also vital. Blockages in certain spots, like the left main coronary artery, are very risky. They affect a big part of the heart’s blood supply.
Left Main Coronary Artery Blockage: These blockages are very dangerous. They can cause a lot of heart damage if there’s a heart attack.
Knowing these factors helps doctors assess risk and choose the best treatment for heart disease patients.
The Role of Collateral Circulation in Extending Life
Collateral circulation is key in helping people with blocked arteries live longer. When main arteries get blocked, the body tries to help by growing smaller, backup vessels. These vessels help get blood back to the heart muscle.
How Collateral Arteries Develop
Collateral arteries grow in response to reduced blood flow due to blockages. This is a complex process that involves new vessels or the growth of small ones. Many factors can affect how well these arteries develop, like the blockage’s severity, health risks, and genetics.
How Long Can You Live with Collateral Arteries?
Having well-developed collateral arteries can greatly improve life expectancy for those with heart disease. Research shows that those with strong collateral circulation live longer and have fewer symptoms. But, how long someone can live varies a lot, depending on their disease severity and overall health.
| Collateral Circulation Status | Average Survival Rate | Symptom Reduction |
| Well-developed | 80% at 5 years | Significant reduction |
| Poorly developed | 50% at 5 years | Minimal reduction |
Limitations of Collateral Circulation
Collateral circulation is lifesaving but has its limits. How well these arteries work depends on the blockage’s severity and location. They might not completely get rid of symptoms or prevent future heart problems. So, even with good collateral arteries, people with heart disease need ongoing care and lifestyle changes.
Treatment Options and Their Effect on Life Expectancy
CAD treatment includes many approaches, from medicine to surgery. Each option affects life expectancy differently. The right treatment depends on the disease’s severity, the patient’s health, and other conditions.
Medical Management Approaches
Medical management is often the first step for CAD. It uses medicines to control symptoms, slow disease growth, and lower risk of problems. Statins, beta-blockers, and antiplatelet agents are common.
Benefits of Medical Management:
- Reduces the risk of heart attack and stroke
- Manages symptoms such as angina
- Slows the progression of CAD
Interventional Procedures (Stents and Angioplasty)
For severe CAD or when medicine doesn’t work, procedures like angioplasty and stenting are used. These aim to open blocked arteries and improve blood flow to the heart.
| Procedure | Description | Benefits |
| Angioplasty | A procedure that uses a balloon to widen narrowed or blocked arteries. | Restores blood flow, reduces symptoms |
| Stenting | Involves placing a small mesh device (stent) to keep the artery open. | Prevents re-narrowing, improves blood flow |
Surgical Options (Bypass Surgery)
Coronary artery bypass grafting (CABG) is a surgery that bypasses blocked arteries with grafts. It’s often for complex or multi-vessel disease.
Advances in surgical techniques and post-operative care have significantly improved outcomes for CABG patients.
Choosing the right CAD treatment is personal. It depends on the patient’s health, disease extent, and preferences. Understanding the options helps patients and doctors create a plan that improves life expectancy and quality.
Lifestyle Modifications to Extend Life with Arterial Disease
Changing your lifestyle is key to managing and possibly reversing arterial disease. By living a heart-healthy life, you can greatly improve your life span and quality of life.
Dietary Changes That Make a Difference
Eating a balanced diet is vital for managing coronary artery disease (CAD). Key dietary recommendations include:
- Eat a variety of fruits and vegetables for antioxidants and fiber.
- Add whole grains and lean proteins to your meals.
- Reduce saturated fats, trans fats, and cholesterol.
- Lower sodium to control blood pressure.
The American Heart Association stresses, “A healthy diet is key to preventing and managing heart disease.”
“Focusing on a dietary pattern, not specific nutrients, helps make lasting lifestyle changes.”
Exercise Recommendations for Patients with CAC
Regular exercise is vital for those with coronary artery calcification (CAC). Recommended exercises include:
- Do aerobic activities like brisk walking, cycling, or swimming for 150 minutes weekly.
- Include resistance training to boost muscle strength and heart health.
- Do flexibility and stretching exercises to improve mobility.
Stress Management and Mental Health
Managing stress is critical for those with arterial disease. Techniques like meditation, yoga, and deep breathing can lower stress. Also, keeping social connections and getting professional help when needed supports mental health.
Can You Reverse Hardened Arteries?
The idea of “reversing” hardened arteries is complex. Lifestyle changes can slow or stop disease progression. Studies show that a complete lifestyle overhaul can improve arterial health. A leading cardiology journal notes, “Aggressive lifestyle changes can greatly reduce heart disease risk factors.”
By making these lifestyle changes, people with arterial disease can live longer and better.
Conclusion: Living Well Despite Coronary Artery Disease
Managing coronary artery disease (CAD) needs a mix of medical care, lifestyle changes, and regular check-ups. This approach helps patients live better and possibly live longer with CAD.
Handling CAD means making diet changes, exercising, managing stress, and getting medical help. With the right care, many people can manage CAD well. This improves their life expectancy and overall health.
Knowing the risks of CAD and using the right treatments helps people control their condition. We stress the need for a full plan to manage CAD. This way, patients can do better and live well, even with CAD, improving their life span.
FAQ
How long can you live with 2 blocked arteries?
Living with 2 blocked arteries depends on how bad the blockage is and your overall health. With the right care, many people can live for years. We talk about what affects your chances and how to manage it well.
What is the life expectancy with severe coronary artery calcification?
Severe coronary artery calcification raises your risk of heart problems and death. A CT scan gives a calcium score, which shows how bad it is. A higher score means more risk.
Can you live a long life with coronary artery calcification?
Yes, you can live a long life with proper care and lifestyle changes. Knowing the risks and managing your condition is key.
How long does it take to clog arteries?
Clogging arteries is a slow process. It depends on your lifestyle, genes, and health. Everyone’s timeline is different.
Can you reverse hardened arteries?
Reversing hardened arteries is hard, but not impossible. Changing your diet, exercising, and managing stress can slow it down.
What is the significance of collateral circulation in patients with blocked arteries?
Collateral circulation can help by improving blood flow to the heart. But, it has its limits. Knowing its role is important for managing your condition.
How many blocked arteries can you have before it’s considered a critical risk?
The number and location of blocked arteries matter. So does how blocked they are. Understanding these helps assess your risk and plan treatment.
What are the treatment options for coronary artery disease, and how do they impact life expectancy?
Treatments for coronary artery disease include medicine, procedures, and surgery. Knowing the pros and cons of each helps improve your chances and life expectancy.
How does arteriosclerosis affect life expectancy?
Arteriosclerosis can shorten your life by increasing heart disease risk. Managing it with lifestyle changes and treatments is vital for better outcomes.
What is the impact of a 70-99% blockage in heart arteries on life expectancy?
A 70-99% blockage is serious and raises your risk of heart problems. Understanding this and getting the right treatment is key to living longer.
Can lifestyle modifications extend life with arterial disease?
Yes, changing your lifestyle can help you live longer and better with arterial disease. Making healthy choices is important.
What is the life expectancy with atherosclerosis?
Atherosclerosis can shorten your life due to heart disease risk. Managing it with lifestyle changes and treatments is essential for better health.
How long can you live with blocked arteries in legs?
Living with blocked arteries in legs depends on the blockage’s severity, your health, and treatment. With the right care, many people can live for years.
What is the impact of coronary artery disease on life expectancy?
Coronary artery disease can shorten your life by increasing heart disease risk. Understanding the risks and managing your condition is vital for better health.
References:
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766.https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312




































