Heart stents are designed to stay in your body permanently. However, their performance over time depends greatly on your overall health and lifestyle. Many patients ask, “how long do stents last in heart?” — and the answer can vary.
At Liv Hospital, we understand how important it is to keep your stent functioning properly. Our expert team provides the best care, monitoring, and guidance to ensure your heart stays healthy for years to come.
The lifespan of heart stents depends on several factors, including the type of stent, medical condition, and lifestyle habits. Knowing how long stents last in heart helps patients take proactive steps toward better long-term heart health.
Heart stents are key for those with coronary artery disease. They offer a vital lifeline to prevent heart attacks. These small, mesh-like tubes keep arteries open, ensuring blood flows well to the heart.
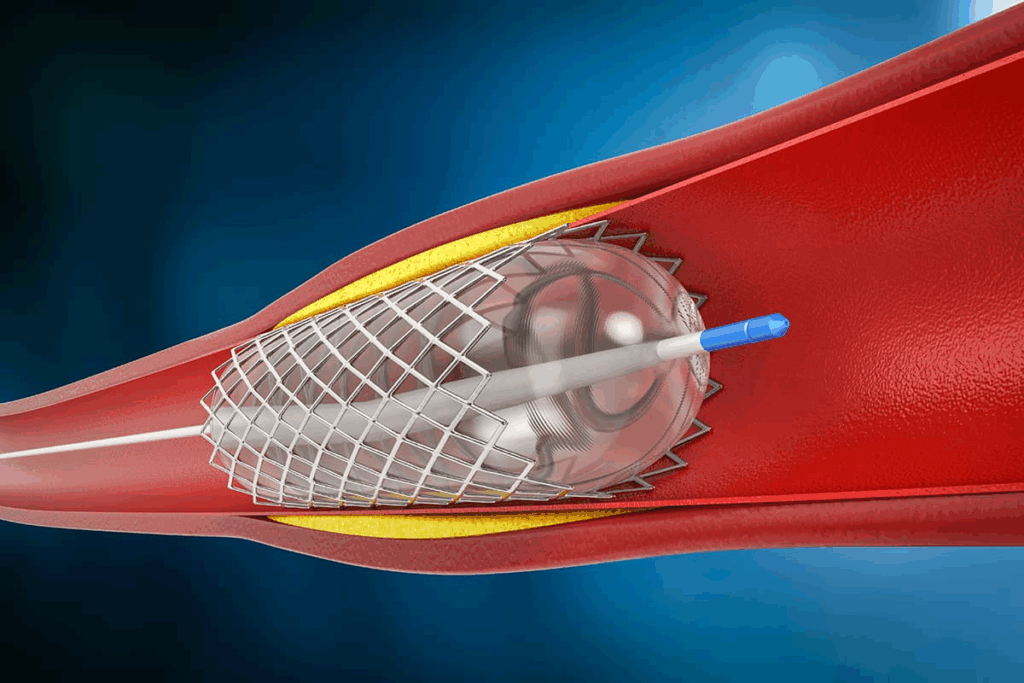
Heart stents, or coronary stents, are tiny, expandable metal mesh tubes. They treat narrowed or blocked coronary arteries, known as coronary artery disease. By keeping arteries open, stents improve blood flow to the heart muscle. This reduces symptoms like chest pain and shortness of breath.
The stent placement process is called percutaneous coronary intervention (PCI). A thin, flexible tube called a catheter is inserted into an artery in the leg or arm. It’s guided to the blocked coronary artery.
Next, a balloon on the catheter inflates to widen the artery. The stent expands to keep the artery open. Over time, the artery walls heal around the stent, securing it in place.
Stents are often used for coronary artery disease. This occurs when coronary arteries narrow or block due to plaque buildup. This can cause angina, heart attacks, and serious heart issues.
Stents may also help those who have had heart attacks or other heart diseases. Understanding heart stents and their role in managing heart disease is important. It helps patients see how these devices improve their quality of life.
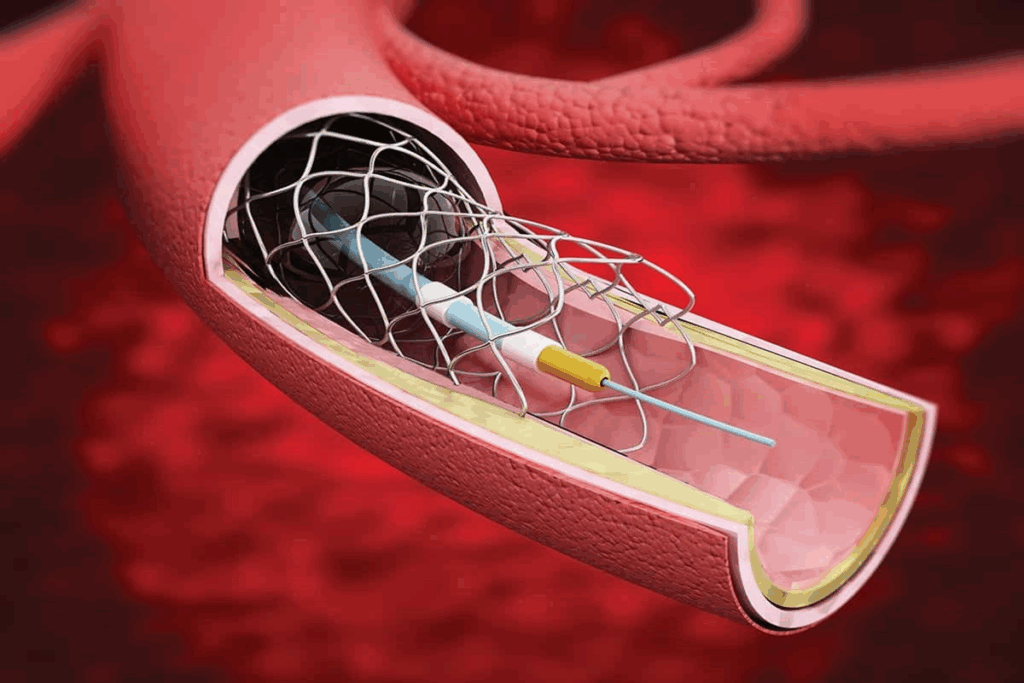
There are many types of heart stents, each with its own benefits. They are made to help with different parts of coronary artery disease. The right stent depends on the patient’s health, how bad the blockage is, and if they can follow medication instructions.
Bare-metal stents are made from metals like stainless steel. They help keep the artery open. These stents are good for patients at low risk of artery narrowing or who can’t use drug-eluting stents.
Key Features of Bare-Metal Stents:
Drug-eluting stents have a coating that slowly releases medicine. This helps prevent the artery from narrowing again. They are popular because they work well in preventing artery narrowing.
Advantages of Drug-Eluting Stents:
Bioresorbable vascular scaffolds are new stents that dissolve over time. They aim to reduce long-term problems with permanent stents.
Benefits of Bioresorbable Vascular Scaffolds:
The materials in heart stents are key to their success and how long they last. Things like the metal type, stent thickness, and drug coatings matter. These factors affect how well the stent works and how long it lasts.
Knowing how long heart stents last is key for both patients and doctors. The stent’s life span varies based on its type and the patient’s lifestyle.
Bare-metal stents (BMS) are made of metal mesh and last long. But, they are more likely to cause restenosis than drug-eluting stents. BMS can last 10 to 15 years or more. Yet, the risk of restenosis is highest in the first year.
Drug-eluting stents (DES) release medicine to prevent cell growth, lowering restenosis risk. They are the top choice for many because of their better results. DES can last as long as BMS, with some studies showing they can be effective for 10 years or more.
Bioresorbable vascular scaffolds (BVS) dissolve over time, usually in 2 to 3 years after being put in. They aim to improve outcomes by leaving no permanent implant. But, their use is limited due to concerns about thrombosis and restenosis.
Studies have given us insights into heart stent longevity. A detailed look at stent lifespan is shown in the table below:
| Stent Type | Average Lifespan | Restenosis Risk |
| Bare-Metal Stents | 10-15 years | Higher |
| Drug-Eluting Stents | 10+ years | Lower |
| Bioresorbable Stents | 2-3 years (dissolves) | Variable |
The data shows that while BMS last longer physically, DES offer better results due to lower restenosis risk. BVS, though limited, show promise in treating coronary artery disease.
It’s clear that patient lifestyle and sticking to medication are key to stent longevity. By understanding these factors and picking the right stent, patients can extend their stent’s life.
The journey of heart stent technology has been incredible. It has changed how we treat coronary artery disease. We’ve seen big steps forward in design, materials, and how they work, making care better for patients.
The first heart stents came out in the late 1980s. They were bare-metal stents (BMS). They were a big leap from just balloon angioplasty, but they had downsides. They could cause restenosis because the body reacts to the metal.
The early 2000s brought drug-eluting stents (DES). These stents had medicine that cut down restenosis risk. Then, third-generation stents came with better drug delivery and materials that were kinder to the body.
Now, stent tech keeps getting better. We have bioresorbable vascular scaffolds (BVS) that dissolve over time. This could mean fewer long-term problems. Also, new materials make stents last longer and work better with the body.
Looking to the future, stent tech will keep getting better. We’ll see nanotechnology and personalized medicine in stents. These changes will make stents work even better, help patients more, and maybe let us use stents in new ways.
It’s important to know what affects how long a heart stent lasts. This knowledge helps both patients and doctors. The lifespan of a stent depends on several things. These include the patient’s health, lifestyle, and the procedure itself.
How long a stent lasts can be influenced by the patient’s health. Age, overall health, diabetes, and kidney function are key factors.
Our lifestyle choices can also affect how long a stent lasts. Stopping smoking, eating well, and exercising are important. These habits can help or hurt the stent’s performance.
For example, smoking can make atherosclerosis worse, which can shorten the stent’s life. On the other hand, a healthy diet and regular exercise can help keep the heart healthy and the stent working better.
The way the stent is placed also matters a lot. The type of stent, how well it’s placed, and handling any problems during the procedure are all important.
| Procedural Factor | Impact on Stent Longevity |
| Type of Stent | Drug-eluting stents usually work better than bare-metal stents in preventing restenosis. |
| Precision of Stent Placement | Placing the stent accurately can lower the risk of problems like stent thrombosis and restenosis. |
| Management of Complications | Handling any problems during the procedure well can improve how long the stent lasts. |
In summary, the life of a heart stent depends on many things. These include the patient’s health, lifestyle, and the procedure. Understanding and managing these factors can help make the stent work better and improve patient outcomes.
Heart stents save lives but come with risks. Certain issues can make them last shorter. Knowing these risks helps both patients and doctors.
Restenosis is when arteries narrow again after a stent is placed. The risk depends on the stent type, with bare-metal stents more likely to fail than drug-eluting ones. Diabetes and small vessels can also play a part.
Drug-eluting stents lower restenosis risk. Yet, it can happen. This shows the need for ongoing care and checks.
Stent thrombosis is a serious issue where a clot forms in the stent. This risk is higher in the first few months if antiplatelet therapy stops too soon. Risks include stent issues and not taking medication as advised.
“The occurrence of stent thrombosis is a medical emergency requiring immediate attention.”
Stent fracture is rare but serious. It can cause restenosis and thrombosis. High mobility or flexion areas increase fracture risk. Stent displacement can happen during or after the procedure.
Inflammation to the stent can lead to restenosis. Stent material biocompatibility is key to avoiding this. New stent designs aim to reduce inflammation with better materials and coatings.
Understanding these complications helps doctors manage care better. Patients can also make informed choices about their treatment and follow-up.
Medications are key to keeping heart stents working well. They help the stent last longer and keep the heart healthy. After a stent is placed, doctors give patients a set of medicines to prevent problems and help the stent work right.
Antiplatelet therapy is very important after a stent is put in. This treatment stops platelets in the blood from clumping around the stent. Doctors often prescribe aspirin and P2Y12 inhibitors like clopidogrel for this. These drugs help avoid stent thrombosis, a serious condition.
It’s vital for patients to stick to their antiplatelet therapy. Changing or skipping doses can raise the risk of stent problems.
How long a patient needs to take antiplatelet therapy depends on several things. This includes the type of stent and the patient’s risk level. Usually, those with drug-eluting stents need to take these medicines for at least 12 months. Patients with bare-metal stents might not need them for as long.
Patients should talk to their doctors about their specific medication plan. This helps understand how long they’ll need to take the medicines and if any changes are needed.
Medication adherence is very important for the success of heart stents. Taking medicines as prescribed can lead to better outcomes. This includes lower risks of restenosis and stent thrombosis.
Antiplatelet therapy is usually safe, but some people might have side effects. Common issues include more bruising, bleeding gums, or stomach problems. In rare cases, serious bleeding can happen.
We suggest patients work closely with their healthcare team to handle side effects. This might mean changing the dosage or switching to different medicines. Always talk to a doctor before making any changes to your medication.
Living a heart-healthy lifestyle is key for stent patients. It helps keep stents working well for longer. Making smart choices can greatly boost your heart health and stent performance.
Eating right is essential for stent patients. Focus on nutrient-rich foods like fruits, veggies, whole grains, lean proteins, and healthy fats. Try to cut down on saturated fats, sodium, and added sugars.
Here are some diet tips:
Staying active is key for heart health and stent function. Aim for moderate-intensity exercises like brisk walking, cycling, or swimming for 150 minutes weekly. Adding strength training twice a week is also good.
Always talk to your doctor before starting any new exercise. They’ll help pick the best activities for you.
Too much stress can harm your heart and stent. Try stress-reducing techniques like meditation, deep breathing, or yoga. Enjoying hobbies and activities that make you happy can also help.
Some habits can hurt your stent’s performance. Avoid smoking and excessive alcohol use. Keeping a healthy weight and managing diabetes and high blood pressure are also important.
For more tips on living well after cardiac procedures, check out lifestyle changes after angioplasty.
After a stent is placed, it’s important to keep an eye on it. This helps make sure it’s working right and catches any problems early. We know this ongoing care is key for your heart’s health.
Having a set schedule for follow-ups is very important. Here’s what we usually suggest:
These visits help us keep track of the stent and make any changes to your treatment plan.
To check how the stent is working and your heart’s health, we use different tests. These include:
It’s important for patients to know the signs of possible stent problems. These include:
If you notice any of these symptoms, get medical help right away. Catching and treating problems early can make a big difference.
By sticking to your follow-up schedule and watching for these signs, you can work with your healthcare team. This helps ensure your heart stent works well for a long time.
Understanding how to keep heart stents working well is key. We’ve talked about the different types of stents and what makes them last longer. This knowledge helps people with heart stents live better, with healthier hearts and overall well-being.
Managing heart stents means sticking to medication, making healthy lifestyle choices, and seeing your doctor regularly. Taking your medicines as told, staying active, and eating right helps your stents work well for a long time. For more tips on life after getting a stent, check out Continental Hospitals’ guide on heart care after stent.
With the right care, most people can get back to their usual activities. They can enjoy life more, with less chest pain and better breathing. By focusing on heart health and following their doctor’s advice, people with heart stents can stay well and feel confident.
Heart stent lifespan varies. It depends on the stent type, patient health, and lifestyle. Bare-metal stents can last up to 15 years or more. Drug-eluting stents often last beyond 15 years.
Several factors impact stent longevity. These include patient health, lifestyle, and the stent placement procedure. Diet, exercise, and avoiding harmful habits are key.
Yes, a healthy lifestyle can help a heart stent last longer. Eating well, exercising, managing stress, and not smoking are important.
Complications like restenosis, stent thrombosis, fracture, and inflammation can shorten stent life. These issues can affect how long a stent lasts.
Taking medication as prescribed is very important after a stent is placed. Antiplatelet therapy prevents clots. Following the medication plan helps the stent work better and last longer.
Follow-up appointments after stent placement vary. But, regular check-ups with your doctor are needed. They help monitor the stent and your heart health.
Tests like angiography, stress tests, and imaging (echocardiography or cardiac MRI) are used. They help check how well a stent is working.
Yes, signs like chest pain, shortness of breath, or cardiac distress can indicate stent problems. If you notice these symptoms, seek medical help right away.
Yes, the type of stent affects its lifespan. Different stents, like bare-metal, drug-eluting, or bioresorbable, have different durability and performance.
Heart stent technology has greatly improved. From bare-metal stents to drug-eluting and bioresorbable stents, advancements have increased stent longevity and performance.
Bioresorbable vascular scaffolds dissolve over time, usually within 2 to 3 years. The exact timeline can vary based on patient factors and the specific device used.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us