Cancer treatment often involves chemotherapy cycles. But, the number of cycles can vary a lot from one patient to another. A recent study found that the average number of chemotherapy cycles differs based on the type and stage of cancer.
For many patients, the question of how many rounds of chemotherapy are needed is a big concern. The answer depends on several factors. These include the chemo regimen and standard chemo protocols set by healthcare providers.
We know that undergoing chemotherapy can be tough. Knowing what to expect is key. The number of chemotherapy rounds is based on the patient’s response and the specific cancer diagnosis.
Key Takeaways
- Chemotherapy cycles vary based on cancer type and stage.
- The number of chemotherapy rounds is determined by the patient’s response and diagnosis.
- Standard chemo protocols guide treatment decisions.
- Understanding the chemo regimen is essential for patient care.
- Chemotherapy treatment plans are tailored to individual needs.
Understanding Chemotherapy Basics
Chemotherapy is a treatment that fights cancer all over the body. It uses drugs to kill or slow down cancer cells. This method is key in treating cancer that has spread or is likely to spread.
What is Chemotherapy?
Chemotherapy is a cancer treatment that uses drugs. It’s a systemic treatment that affects the whole body. This makes it very effective against cancer that has spread or is at high risk of spreading.
How Chemotherapy Works to Fight Cancer
Chemotherapy uses drugs to target and kill cancer cells. These drugs can be given in various ways, based on the cancer type and treatment plan. The goal is to stop cancer cells from growing and dividing, leading to their death. It can be used alone or with other treatments like surgery and radiation.
Different Types of Chemotherapy Delivery Methods
Chemotherapy can be given in different ways, including:
| Delivery Method | Description |
| Intravenous (IV) Chemotherapy | Given directly into a vein, IV chemotherapy delivers high doses quickly. |
| Oral Chemotherapy | Taken as pills or liquids, oral chemotherapy is easy to take at home. |
| Topical Chemotherapy | Applied to the skin, it’s used for some skin cancers or pre-cancerous conditions. |
Understanding these basics is key for patients to make informed choices. Knowing how chemotherapy works and the different ways it can be given helps patients prepare for their treatment.
How Many Rounds of Chemo Is Normal?
Knowing how many chemotherapy cycles you’ll need is key for patients. The number can change a lot. It depends on the cancer type, stage, and your health.
Average Number of Chemotherapy Cycles
Most people get between 3 to 6 cycles of chemo. But, it really depends on your cancer and treatment goals. For example, early-stage cancer might need fewer cycles, while advanced cancer might need more.
Barbara Jeffery, a breast cancer patient, had many rounds of chemo. Her story shows how treatment plans can vary. It’s all about what’s best for you.
Chemotherapy is not a one-size-fits-all treatment. It’s made just for you.
Factors That Determine Treatment Length
Several things can affect how long chemo lasts. These include:
- The type and stage of cancer
- Your overall health and how well you can handle treatment
- The specific chemo regimen used
- How well the cancer responds to treatment
These factors can really change how many cycles you need. For example, aggressive cancers might need more treatment. But, slower-growing tumors might need fewer cycles.
Why Treatment Plans Vary Between Patients
Every patient’s treatment plan is different. This is because each person’s cancer and health are unique. Doctors say, “one size does not fit all when it comes to chemotherapy.”
“The key to successful chemotherapy is tailoring the treatment to the individual patient’s needs and response to therapy.” –
Oncologist’s statement
Understanding these factors helps patients prepare for chemo. It also helps them talk better with their doctors.
What Constitutes a Chemotherapy Cycle?
To fully understand chemotherapy, it’s key to know what a cycle is. A chemotherapy cycle is the time between starting treatment and starting the next round.
Defining a Chemotherapy Cycle
A cycle includes giving chemotherapy drugs and then a break. This break lets the body heal from the treatment. The cycle’s length changes based on the cancer type, drugs, and the patient’s health.
What is a 21-Day Chemo Cycle?
A 21-day chemo cycle, or 3-week cycle chemotherapy, is common in cancer treatment. It starts with chemotherapy on the first day, then 20 days of rest. This cycle repeats as needed.
Other Common Cycle Patterns
While the 21-day cycle is common, others exist. For example, some use a 14-day or 28-day cycle. The cycle length depends on the treatment plan and how well the patient responds.
Knowing these cycles helps patients get ready for treatment and set realistic expectations. Different cycles let doctors customize treatment for each patient. This approach makes chemotherapy more effective and reduces side effects.
Duration of Chemotherapy Sessions
The time a chemotherapy session lasts can change a lot. It depends on the type of treatment, the patient’s health, and the cancer type. Knowing these details helps patients get ready for their treatment.
How long is a typical chemo session?
Chemotherapy sessions can last from 30 minutes to several hours. Most sessions are between 1 to 3 hours. But, it can vary a lot.
Some drugs are given quickly, while others need more time. A study in the Journal of Clinical Oncology found the average session is about 2 hours. But, this can change based on the treatment and how the patient responds.
| Chemotherapy Type | Average Session Duration |
| Intravenous Chemotherapy | 1-3 hours |
| Oral Chemotherapy | Minimal (self-administered) |
| Intraperitoneal Chemotherapy | 2-4 hours |
Factors affecting session length
Many things can make a chemotherapy session longer or shorter. These include:
- The type and dose of chemotherapy drugs
- The method of administration (e.g., IV, oral, or intraperitoneal)
- The patient’s overall health and response to treatment
- Any necessary pre-medications or hydration
Dr. Smith, an oncologist, said, “The treatment plan’s complexity and the patient’s needs greatly affect session length.”
Preparation and recovery time
Patients need to think about the time for getting ready and recovering. Getting ready might include:
- Pre-medication to prevent side effects
- Insertion of an IV line or other access device
- Initial assessment and vitals check
Recovery time varies. But, patients are watched closely after treatment to make sure they’re okay. A patient said, “Recovery time is just as important as the treatment itself. It helps your body adjust.”
“Chemotherapy is a journey, not just a treatment. Understanding what to expect can make a significant difference in how you navigate it.” –
A cancer survivor
By knowing what affects chemotherapy session length, patients can prepare better. This helps them plan for their treatment.
Chemotherapy Treatment Schedules
It’s important for patients to know about chemotherapy treatment schedules. These plans are made just for them, based on their cancer type and needs.
How Often is Chemotherapy Administered?
Chemotherapy schedules vary a lot. They depend on the cancer type, the drugs used, and the treatment goals. Here are some common schedules:
- Weekly chemotherapy: This is for some cancers like leukemia or lymphoma.
- Every 2-3 weeks: This is common for many treatments, giving time to recover.
- Continuous infusion: Treatments given over days or weeks.
The treatment plan decides how often chemotherapy is given. It aims to be effective while managing side effects.
Rest Periods Between Treatments
Rest periods between treatments help the body recover. They let the body:
- Rebuild healthy cells damaged by treatment.
- Gain strength and energy.
- Lower the risk of infection and other problems.
The length of these rest periods can change. It depends on the treatment and the patient’s health.
Adjusting Schedules Based on Patient Response
Chemotherapy plans are not the same for everyone. They change based on how well the treatment works and how the patient feels. Adjustments might be made for:
| Factor | Adjustment |
| Severe side effects | Delaying treatment or reducing dosage |
| Poor response to treatment | Changing the chemotherapy regimen or adding other treatments |
| Patient’s overall health | Adjusting the treatment schedule to accommodate recovery or managing comorbidities |
By watching how patients respond and adjusting plans, doctors can make chemotherapy work better. They aim to keep the treatment effective while improving the patient’s life quality.
Total Duration of Chemotherapy Treatment
Knowing how long chemotherapy lasts is key for patients. The time it takes can change a lot. It depends on the cancer type, stage, patient’s health, and treatment goals.
How Long Does a Complete Course of Chemotherapy Last?
Chemotherapy can last from a few months to several years. The exact time depends on the cancer type, stage, and how well the treatment works.
For example, early-stage breast cancer might need 3 to 6 months of treatment. But, advanced cancer or certain lymphomas could need a year or more.
Short-term vs. Long-term Treatment Plans
Chemotherapy plans can be short or long. Short plans last a few months and are for early cancers or to shrink tumors before surgery.
Long plans can last a year or more. They’re for more advanced cancers or those harder to treat.
| Treatment Plan | Duration | Typical Use |
| Short-term | 3-6 months | Early-stage cancers, preoperative treatment |
| Long-term | 1 year or more | Advanced cancers, difficult-to-treat cancers |
Maintenance Chemotherapy
Maintenance chemotherapy is ongoing after the first intense treatment. It aims to stop cancer from coming back and keep it in remission.
This treatment is common for cancers like leukemia or lymphoma. It can go on for months to years.
Key aspects of maintenance chemotherapy include:
- Lower doses of chemotherapy drugs
- Less frequent treatment sessions
- Ongoing monitoring of patient response and side effects
Understanding chemotherapy duration helps patients prepare. It lets them make informed decisions about their care.
Chemotherapy Protocols for Different Cancer Types
The type and stage of cancer are key in choosing the right chemotherapy. Each cancer type reacts differently to treatments. We’ll look at how chemotherapy works for breast, lung, colorectal, lymphoma, and leukemia cancers.
Breast Cancer Chemotherapy Regimens
Breast cancer treatments change based on the cancer’s stage and characteristics. Drugs like anthracyclines, taxanes, and cyclophosphamide are common. For example, the AC-T regimen is often used for early-stage breast cancer.
A breast cancer survivor said, “My chemotherapy journey was tough, but knowing the plan helped me deal with side effects.”
“The key to successful treatment is tailoring the chemotherapy regimen to the individual patient’s needs,” – A medical oncologist.
Lung Cancer Treatment Protocols
Lung cancer treatments vary based on the type and stage. Non-small cell lung cancer often gets platinum-based doublets like cisplatin and pemetrexed. Small cell lung cancer is usually treated with etoposide and platinum-based drugs.
| Lung Cancer Type | Common Chemotherapy Regimens |
| Non-Small Cell Lung Cancer | Cisplatin + Pemetrexed, Carboplatin + Paclitaxel |
| Small Cell Lung Cancer | Etoposide + Cisplatin, Etoposide + Carboplatin |
Colorectal Cancer Chemotherapy
Colorectal cancer treatments often include 5-fluorouracil (5-FU), oxaliplatin, and irinotecan. FOLFOX is a common choice for stage III colon cancer. For metastatic colorectal cancer, FOLFIRI is often used.
Lymphoma and Leukemia Treatment Plans
Lymphoma and leukemia treatments are very specific. For aggressive lymphomas, R-CHOP is a standard treatment. Leukemia treatments vary, with acute leukemia needing intensive chemotherapy.
Knowing these chemotherapy protocols is key for patients and doctors. Tailoring treatments to each cancer type can improve outcomes and quality of life.
Oral Chemotherapy vs. Intravenous Treatment
Patients often face a big decision: oral chemotherapy or intravenous treatment. Each has its own pros and cons. Knowing these differences helps patients make a smart choice.
Comparing Pill-Based and IV Chemotherapy
Oral chemotherapy means taking pills or liquids at home. This makes it easier to avoid hospital visits. But, it’s key to follow the treatment plan closely.
Intravenous chemotherapy is given through a vein. It’s used for aggressive cancers and is given in a clinic. This way, doctors can watch how the patient is doing and handle side effects quickly.
Side Effects of Chemotherapy Pills
Oral chemotherapy side effects depend on the drug and the patient. Common issues include nausea, tiredness, and hair loss. Patients taking pills at home must tell their doctor about any side effects right away.
- Nausea and vomiting
- Fatigue and weakness
- Hair loss
- Increased risk of infection
Duration Differences Between Delivery Methods
Chemotherapy treatment time can vary a lot. Oral chemotherapy might last longer, sometimes into maintenance therapy. Intravenous chemotherapy is given in cycles with breaks in between to let the body rest.
It’s important for patients to understand these differences. Talking to their doctor about their treatment plan helps them get ready for what’s ahead.
Factors That May Alter the Number of Chemo Rounds
Many important factors can change how many chemotherapy rounds a patient gets. It’s key for patients to understand these factors. This helps them know what to expect during their cancer treatment.
Cancer Stage and Aggressiveness
The stage and how aggressive the cancer is greatly affect treatment. Advanced cancer often needs more treatment, leading to more chemotherapy cycles. For example, someone with stage III or IV cancer might need more rounds than someone with an earlier stage.
How aggressive the cancer is also matters. Tumors that grow fast or are high-grade might need a stronger chemotherapy plan. This could mean more treatment rounds.
Patient Health and Tolerance
A patient’s health and how well they can handle chemotherapy are very important. Those with health issues or severe side effects might need their treatment plans changed. This could mean fewer rounds of chemotherapy or a different schedule.
Managing side effects well is key for patients to handle chemotherapy and finish their treatment. Doctors keep a close eye on patients’ health. They adjust treatment plans to make sure it works without being too hard on the patient.
Treatment Response Assessment
How a patient reacts to chemotherapy is a big factor in how many rounds they’ll have. Doctors use tests and scans to check how well the treatment is working.
If a patient does well with chemotherapy, their treatment might be adjusted. This could mean finishing the planned rounds or stopping early if the cancer is gone or greatly reduced.
But if the cancer doesn’t respond well, the treatment plan could change. This might mean switching to a different chemotherapy or adding other treatments.
Why Doctors Typically Prescribe Six Rounds of Chemo
In many cancer treatment plans, six rounds of chemotherapy are usually recommended. But why is this the case? We’ll look into the science and research that back this standard. We’ll also explore when the number of cycles might change.
The Science Behind the Standard Six-Cycle Approach
The six-cycle chemotherapy regimen is based on a mix of clinical experience, research, and cancer biology. Chemotherapy is given in cycles, with treatment periods followed by recovery. This approach boosts treatment effectiveness while reducing harm to the patient.
Studies show that six cycles of chemotherapy can be effective for many cancers. The exact number of cycles depends on the cancer type, stage, and the patient’s health.
Research Supporting This Treatment Duration
Many clinical trials and studies have looked into the best number of chemotherapy cycles for different cancers. For example, research on breast cancer found that six cycles of certain chemotherapy regimens can be as effective as longer treatments in some cases.
| Cancer Type | Typical Chemotherapy Cycles | Research Findings |
| Breast Cancer | 4-6 cycles | Six cycles shown to be effective in many cases |
| Lung Cancer | 4-6 cycles | Variability in treatment duration based on stage and type |
| Colorectal Cancer | 6-12 cycles | Adjuvant chemotherapy often involves 6 months of treatment |
When Fewer or More Cycles May Be Recommended
While six cycles are standard for many chemotherapy regimens, the actual number can vary. Patients with more aggressive or advanced cancers may need more cycles. Those with earlier-stage cancers might need fewer.
How well a patient responds to treatment also affects the number of cycles. Regular assessments during treatment help doctors adjust the plan as needed. This ensures patients get the best care possible.
How Doctors Monitor Treatment Effectiveness
Checking how well chemotherapy works is key in planning a patient’s next steps. We use different tools to see if the treatment is effective. Then, we adjust the plan as needed.
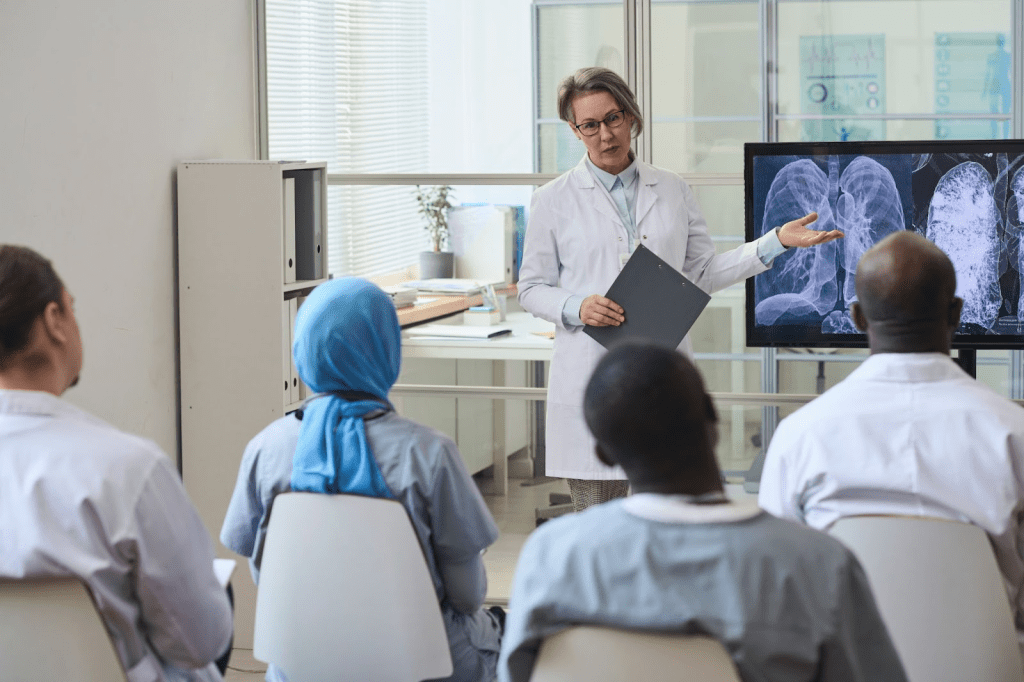
Imaging and Blood Tests During Treatment
During chemotherapy, we use imaging and blood tests to check how well the treatment is working. Tests like CT scans and MRI scans show us the tumor’s size and spread. These tests help us see if the cancer is responding to the treatment.
Blood tests give us information on the patient’s health and tumor markers. Tumor markers are substances found in the blood of some cancer patients. By watching these markers, we can see how well the treatment is working.
Adjusting Treatment Based on Results
The results from these tests help us change the treatment plan. If the cancer is responding well, we might keep the current plan. But if it’s not responding, we might try something different.
Barbara Jeffery’s case shows how treatment plans can change. Her doctors used tests to check her treatment’s effectiveness and made changes. This approach makes sure each patient gets the best care.
When to Consider Changing the Treatment Plan
We might change the treatment plan in several situations. If imaging shows the tumor isn’t shrinking or is growing, we might switch treatments. This could include trying targeted therapy or immunotherapy.
If a patient is having severe side effects, we might adjust the plan to reduce these effects. We aim to treat the cancer effectively while keeping the patient’s quality of life good.
“The key to successful cancer treatment is closely monitoring the patient’s response and being prepared to adjust the treatment plan as needed,” says A leading oncologist. “By using a combination of imaging tests and blood work, we can make informed decisions about the best course of treatment.”
By always checking how well the treatment is working and being ready to change the plan, we can give our patients the best care. This way, we’re always working towards the most effective treatment strategy.
Managing Side Effects Throughout Multiple Rounds
Managing side effects from chemotherapy is key for patients to finish their treatment. Side effects can range from nausea and tiredness to hair loss and nerve damage. Duane Hawkins, for example, dealt with nerve damage during his treatment.
Common Side Effects During Chemotherapy
Side effects from chemotherapy vary among patients. Some common ones include:
- Nausea and Vomiting: Often managed with anti-nausea medications.
- Fatigue: Persistent tiredness that can be alleviated with rest and appropriate exercise.
- Hair Loss: A common side effect, though not universal, which can be emotionally challenging.
- Neuropathy: Numbness or tingling in hands and feet, as seen in Duane Hawkins’ case.
How Side Effects May Change Over Treatment Course
As patients go through multiple rounds of chemotherapy, side effects can change. Some may see a decrease in side effects as their bodies adapt. Others may face new ones.
Nausea might be worse in the first cycles, while neuropathy could worsen later. It’s important to keep track of these changes to adjust care.
Supportive Care During Chemotherapy
Supportive care is essential in managing chemotherapy side effects. This includes:
- Medications: To alleviate specific side effects like nausea or pain.
- Nutritional Support: Ensuring patients receive adequate nutrients to maintain their strength.
- Emotional Support: Counseling or support groups to help cope with the psychological impact of treatment.
With thorough supportive care, we can greatly improve patients’ quality of life during chemotherapy. This helps them better tolerate and complete their treatment.
How Long Chemotherapy Stays in Your Body
Chemotherapy is a complex topic. It’s important to know how these drugs work in our bodies. They can stay with us for different times after treatment. Knowing how they leave our bodies is key for those going through it.
Drug Half-Life and Elimination
The drug half-life is key to understanding how long chemotherapy lasts in us. It’s the time it takes for a drug’s level in our blood to drop by half. Different drugs have different half-lives, from hours to days or weeks.
Our liver and kidneys mainly get rid of these drugs. They break them down and remove them from our body. But, how well they do this can change based on our age, health, and organ function.
Lingering Effects After Treatment Ends
Even when the drugs are gone, we might feel some lingering effects. These can include tiredness, changes in taste or smell, and nerve damage. How long these last can vary a lot.
Some drugs can cause side effects that last for a long time. These can be months or even years after treatment. Knowing about these effects helps doctors take better care of their patients.
Recovery Timeline Post-Chemotherapy
The recovery timeline after chemotherapy is different for everyone. Some people start feeling better in weeks, while others take months. The type of treatment, our health, and how well we recover all play a part.
While recovering, patients often need a special care plan. This includes advice on food, exercise, and doctor visits. Following this plan helps our bodies heal better and lowers the chance of lasting side effects.
When Additional Rounds of Chemotherapy May Be Needed
Deciding on more chemotherapy depends on how well the cancer responds to treatment. While most patients get a set number of cycles, some may need more or less. This varies based on their unique situation.
Recurrence Scenarios Requiring More Treatment
Cancer coming back is a main reason for more chemotherapy. When cancer returns, treatment can help control it. For example, Barbara Jeffery needed more treatment after her cancer came back.
The type and length of extra chemotherapy depend on the recurrence’s nature and the patient’s past treatments.
Recurrence can happen locally, regionally, or distantly. Local means it’s back in the same area. Regional means it’s in nearby lymph nodes or tissues. Distant means it’s spread to other parts of the body.
Maximum Lifetime Chemotherapy Limits
There’s a limit to how much chemotherapy a person can safely get. This limit is based on the drugs used and their long-term side effects. Some drugs, like anthracyclines, have a heart damage risk.
Doctors look at a patient’s past chemotherapy when deciding on more treatment. The goal is to weigh the benefits against the risks and side effects. When the safe dose is reached, other treatments might be considered.
Alternative Treatments When Standard Chemo Isn’t Enough
When standard chemotherapy stops working or reaches its limit, doctors look at other options. These can include targeted therapies, immunotherapies, or clinical trials for new treatments.
Targeted therapies target cancer cells or the environment that helps them grow. Immunotherapies boost the body’s defenses against cancer. These options offer hope for patients who can’t respond to standard chemotherapy.
In summary, more chemotherapy is needed based on cancer recurrence and the patient’s health. Understanding these factors and exploring other treatments helps healthcare providers tailor plans for better outcomes.
Newer Approaches to Chemotherapy Scheduling
Cancer research is leading to new ways to schedule chemotherapy. These methods aim to make treatments more effective and reduce side effects. We’ll look at dose-dense, metronomic, and personalized chemotherapy based on genetic testing.
Dose-Dense Chemotherapy
Dose-dense chemotherapy means giving chemotherapy more often, like every two weeks. It’s based on the idea that more frequent treatments can fight cancer cells better. Research has shown it can help patients live longer with certain cancers, like breast and lymphoma.
But, it can also lead to more side effects because the body doesn’t get as much time to recover. Careful patient monitoring is key to managing these side effects and adjusting the treatment plan.
Metronomic Chemotherapy
Metronomic chemotherapy involves giving low doses of chemotherapy continuously. It targets the blood vessels in tumors, slowing their growth. Clinical trials show it can help patients live longer with some cancers.
It’s also less toxic than traditional chemotherapy, making it a good option for those who can’t handle standard treatments well.
Personalized Treatment Based on Genetic Testing
Genetic testing has led to more personalized chemotherapy. It helps doctors choose the right chemotherapy based on a tumor’s genetic makeup. Targeted therapies can then be used, leading to better results with fewer side effects.
This personalized approach is a big step forward in cancer treatment. It offers better outcomes and less harm. As genetic testing gets better, so will this method.
Conclusion
Knowing how many rounds of chemotherapy you’ll need is key. It helps you get ready for your treatment. We’ve looked at how many cycles are typical, the different schedules, and what affects how long treatment lasts.
Every patient’s chemotherapy plan is unique. It depends on the cancer type, stage, and your health. Knowing this helps you understand your treatment better and make smart choices about your care.
Chemotherapy plans change based on how you respond. New ways to schedule treatments, like dose-dense and metronomic, are being tested. These could lead to better outcomes.
In short, chemotherapy is a detailed process that needs careful planning. We aim to give you all the info you need to handle your cancer treatment journey.
FAQ
How often is chemotherapy administered?
How many rounds of chemotherapy are normal?
Chemotherapy cycles can last from 3 to 6 rounds. This number changes based on the cancer type and treatment goals.
What is a chemotherapy cycle?
A chemotherapy cycle is the time between treatments. Most cycles are 21 days long.
How long does a chemotherapy session last?
Chemotherapy sessions can last from 30 minutes to hours. This depends on the treatment and the patient.
What is the difference between oral and intravenous chemotherapy?
Oral chemotherapy is taken as pills. Intravenous chemotherapy is given through a vein. They have different side effects and how long they last.
How do doctors determine the number of chemotherapy rounds?
Doctors look at the cancer stage, patient health, and how well the treatment works. These factors help decide how many rounds are needed.
Why do doctors typically prescribe six rounds of chemotherapy?
The six-cycle standard comes from research and experience. But, the exact number can change based on the patient.
How do doctors monitor treatment effectiveness during chemotherapy?
Doctors use imaging and blood tests to check how well the treatment is working. They adjust the plan as needed.
What are the common side effects of chemotherapy?
Side effects include nausea, fatigue, hair loss, and neuropathy. These can vary in how severe they are and how they affect the patient.
How long do chemotherapy drugs stay in the body?
Chemotherapy drugs stay in the body for different lengths of time. The drug half-life and how the body eliminates them affect recovery.
Can chemotherapy be used to treat cancer recurrence?
Yes, chemotherapy can treat cancer that comes back. The treatment plan is adjusted based on the patient and treatment goals.
What are some newer approaches to chemotherapy scheduling?
New methods include dose-dense and metronomic chemotherapy. They also use genetic testing for personalized treatment. These aim to improve results and reduce side effects.









