At Liv Hospital, we know patients worry about coronary artery disease. They often ask, how many stents a heart can hold. This question is complex and depends on the patient’s needs and artery shape
Understand how many stents can a heart hold, limits, benefits, and real-life cases..
Cardiac stents help open blocked arteries, improving blood flow. The number of stents needed varies with the disease’s severity. We talk about the flexible limits on heart stents, their benefits, and risks.
Deciding on multiple stents depends on the patient’s specific needs and situation. Our team of experts works closely with patients to find the best treatment.
Key Takeaways
- The number of stents a heart can hold is not fixed.
- Cardiac stents restore blood flow through blocked arteries.
- The decision to use multiple stents is based on individual patient needs.
- Our team works closely with patients to determine the best course of treatment.
- Benefits and risks are associated with multiple stents.
The Basics of Cardiac Stents and Their Purpose
Cardiac stents are small, mesh-like tubes that help keep arteries open. They are used to improve heart health. “The use of stents has revolutionized the treatment of coronary artery disease,” say cardiologists worldwide. These devices help restore blood flow to the heart, easing symptoms of heart disease.
What Are Cardiac Stents?
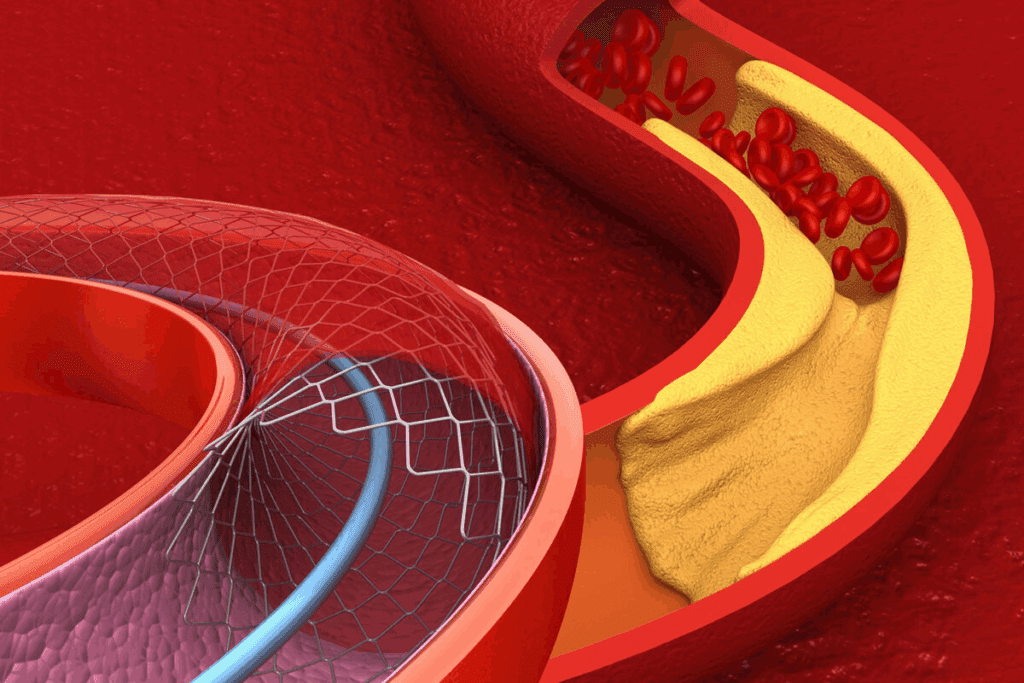
Cardiac stents are medical devices that keep arteries open. They are made from metal mesh and are put in the artery with a balloon catheter. Once in place, the stent expands to support the artery walls, ensuring blood can flow freely.
How Stents Work to Improve Blood Flow
Stents mechanically keep the artery open, improving blood flow to the heart muscle. This is key when coronary arteries are narrowed by plaque buildup (atherosclerosis). By restoring blood flow, stents reduce symptoms like chest pain (angina) and shortness of breath, improving life quality.
Key benefits of cardiac stents include:
- Minimally invasive procedure
- Quick recovery time
- Effective in reducing angina symptoms
Types of Cardiac Stents Available Today
There are mainly two types of cardiac stents: bare-metal stents and drug-eluting stents. Bare-metal stents are made of metal mesh and keep the artery open. Drug-eluting stents are coated with medication to prevent the artery from re-narrowing.
The choice between these stent types depends on various factors, including the patient’s medical history and the specific condition of their coronary arteries. Drug-eluting stents are often preferred when there’s a higher risk of the artery re-narrowing. They release medication that stops new tissue growth.
How Many Stents Can a Heart Hold: Medical Perspectives
The heart’s ability to hold stents varies from person to person. This depends on several clinical factors. Doctors look at these factors to decide the best treatment for each patient.
Is There a Medical Maximum?
There’s no strict limit on how many stents a heart can hold. But, doctors follow guidelines. They consider the disease’s severity, the patient’s health, and the arteries’ anatomy.
Clinical judgment is key in choosing the right number of stents. Diabetes, kidney disease, and the disease’s extent also play a role.
Factors That Determine Stent Capacity
Several factors affect a heart’s stent capacity:
- The disease’s extent and severity
- The patient’s age and health
- Presence of conditions like diabetes or high blood pressure
- The arteries’ size and shape
Doctors evaluate these factors to find the best treatment.
What Research Shows About Multiple Stent Placements
Research on multiple stents has given us important insights. It shows that while there are risks, many patients benefit from it when done right.
| Number of Stents | Common Indications | Potential Risks |
| 1-2 Stents | Single or double vessel disease with significant stenosis | In-stent restenosis, stent thrombosis |
| 3-4 Stents | Multi-vessel disease, complex lesions | Increased risk of complications, higher cost |
| 5 or More Stents | Extensive coronary artery disease, previous stent failure | Higher risk of long-term complications, careful monitoring required |
Having multiple stents can seem scary. But, thanks to new medical tech and strategies, many people with multiple stents live well. Our team creates personalized plans to meet each patient’s needs.
Anatomy of Coronary Arteries and Stent Placement
Coronary artery anatomy is key in stent placement. Stents help restore blood flow to the heart. The coronary arteries supply blood to the heart muscle.
Understanding Coronary Artery Structure
The coronary arteries branch off from the aorta, wrapping around the heart. They supply oxygen and nutrients. The main arteries are the left main and the right coronary artery, with smaller branches.
The arteries have three layers: the intima, media, and adventitia. Plaque buildup happens in the intima. Stents are placed here to keep the artery open.
Common Locations for Stent Placement
Stents are placed where plaque buildup is significant. This causes narrowing or blockage. Common areas include:
- The proximal segments of the major coronary arteries
- Bifurcation areas where branches divide
- Areas with significant plaque accumulation
These areas need precise stent placement. This is to restore blood flow and prevent complications.
How Arterial Anatomy Affects Stent Capacity
The anatomy of coronary arteries affects stent placement. The diameter of the artery, calcification, and vessel tortuosity matter. These factors determine how many stents can be placed.
Larger diameter arteries can handle longer or multiple stents. But tortuous vessels may limit stent placement due to risk. Knowing these factors is key for the best stenting strategy.
“The complexity of coronary artery anatomy necessitates a tailored approach to stent placement, taking into account individual patient characteristics to achieve the best outcomes.”
Healthcare providers tailor treatment plans based on each patient’s anatomy. This approach maximizes stent benefits while reducing risks.
How Many Stents Can Be Placed at One Time
Cardiac stenting can involve placing many stents at once. This is often needed when a patient has many blockages in their coronary arteries.
We will look into the details of this process. We will discuss the benefits and risks of placing many stents in one go.
The Process of Placing Multiple Stents
Putting in multiple stents is a precise and careful process. The cardiologist must carefully plan the placement of each stent. They use tools like angiography to see the arteries.
The first step is to put a catheter into the blocked artery. Then, a balloon is inflated to open it. After that, a stent is placed to keep it open. This is done for each blockage.
Recovery Differences Between Single and Multiple Stent Procedures
Recovery times can differ a lot between single and multiple stent patients. Patients with multiple stents usually need more time to recover. They might also have to stay in the hospital longer.
But, recovery is quick. Most people can get back to normal in just a few days to a week after the procedure.
Medical Considerations for Same-Day Multiple Stenting
There are many things to think about when considering same-day multiple stenting. The patient’s health, the blockages’ severity, and other medical conditions are all important.
Our team carefully looks at each patient’s needs. They make sure placing multiple stents is safe and effective for them.
2 Heart Stents: Common Scenarios and Outcomes
Using two heart stents is a common treatment for coronary artery disease. It has shown great success in improving patient outcomes. This method is often used for patients with multiple blockages or complex coronary disease.
Typical Cases Requiring Two Stents
Two stents are used when there are blockages in different parts of the coronary arteries. This is common in advanced coronary artery disease. A single stent may not be enough to ensure good blood flow to the heart.
Common scenarios include:
- Multiple blockages in different coronary arteries
- Complex lesions that require multiple stents for complete coverage
- Patients who have had previous stent placements and require additional intervention
Success Rates and Long-term Prognosis
The success rate for two stents is generally high. Most patients see a big improvement in their symptoms and quality of life. But, the long-term outcome depends on many factors.
| Outcome | Short-term | Long-term |
| Symptom Improvement | High | Moderate to High |
| Major Adverse Cardiac Events (MACE) | Low | Moderate |
| Survival Rate | High | High |
Patient Experiences with Two Stents
Patient experiences with two stents vary. It depends on their health and how well they respond to treatment. Many patients see a big drop in symptoms like angina and can do more daily activities.
“After receiving two stents, I noticed a dramatic improvement in my energy levels and was able to resume my normal activities without chest pain.” – Patient testimonial.
We know each patient’s journey is different. Outcomes can vary based on many factors. This includes other health conditions and how well the patient sticks to lifestyle changes and medication.
3 Stents in the Heart: When Triple Intervention Is Necessary
Using three stents in the heart is a choice made when coronary disease is severe. This approach is needed to ensure blood flow and prevent more heart problems. We will look at why triple stenting is used, the procedure, recovery, and success stories.
Medical Indications for Three Stents
Patients with severe blockages in different arteries or multiple lesions in one artery might need three stents. Doctors use tests like angiograms and stress tests to decide. These tests show how bad the disease is.
Placement Strategies for Triple Stenting
Placing three stents is a detailed process. Doctors use advanced imaging to guide the stents. They access the arteries through the wrist or groin and place the stents at the blockages.
Recovery and Lifestyle After Three Stent Procedures
After triple stenting, patients need to rest and then slowly get back to normal. They take medicine to prevent clots and manage symptoms. Changing diet, exercise, and quitting smoking are key for long-term health.
Real-Life Cases of Patients with 3 Stents
Many patients have had success with triple stenting. For example, a 55-year-old man with blockages got three stents at once. A year later, he felt much better, moving more and having fewer symptoms.
| Aspect | Pre-Procedure | Post-Procedure |
| Symptoms | Chest pain, shortness of breath | Significant reduction in symptoms |
| Activity Level | Limited mobility | Improved mobility and activity |
| Medication | Various medications for symptoms | Anti-clotting and symptom management medications |
4 Stents in Heart: Managing Complex Coronary Disease
Complex coronary artery disease might need four stents to improve blood flow. When there are many blockages, managing the condition gets harder. We’ll look at when four stents are needed, their risks and benefits, and how to manage them long-term.
Clinical Scenarios Requiring Four Stents
Patients with severe coronary artery disease often need more than one stent. Clinical scenarios that may necessitate four stents include:
- Multiple blockages in different coronary arteries
- Long lesions within a single artery
- Restenosis after previous stent placement
- Complex bifurcation lesions
Cardiologists must plan carefully to ensure the best results.
Risks and Benefits Assessment
Choosing to use four stents involves weighing risks and benefits. Benefits include improved blood flow and reduced symptoms. Risks include stent thrombosis, restenosis, and bleeding. The patient’s health, disease complexity, and success chances are key in this decision.
Long-term Management with Four Stents
Managing four stents long-term is essential. This includes:
- Adherence to dual antiplatelet therapy
- Regular follow-up appointments with their cardiologist
- Lifestyle modifications such as diet and exercise
- Monitoring for possible complications
| Management Strategy | Description | Benefits |
| Dual Antiplatelet Therapy | Medications to prevent clot formation | Reduces risk of stent thrombosis |
| Regular Follow-ups | Monitoring by cardiologist | Early detection of complications |
| Lifestyle Modifications | Diet, exercise, and smoking cessation | Improves overall cardiovascular health |
Patient Outcomes with 4 Heart Stents
Results for patients with four stents vary. This depends on their disease complexity and treatment adherence. With proper care, many see big improvements in their quality of life.
In conclusion, managing complex coronary disease with four stents is complex. It requires careful consideration of clinical scenarios, risks, and benefits, as well as long-term management strategies. Understanding these factors helps healthcare providers improve patient outcomes.
5 Stents in Heart: Pushing the Boundaries
Putting five stents in the heart is a big step in cardiology. It brings both challenges and chances for improvement. Though rare, some people need this many stents to deal with serious heart disease.
Case Studies of Patients with Five Stents
There are stories of people getting five stents in their heart. A study in the Journal of Cardiology showed these patients face more problems than those with fewer stents. Yet, with the right care, many live well.
A 65-year-old man with heart disease is a good example. He got five stents after many procedures. Despite the complexity, he recovered well and got back to his life.
Special Considerations for Extensive Stenting
Those with five stents need extra attention. Their situation needs a detailed plan. This plan must tackle the stents and the heart disease itself.
Important things to consider include:
- Watching for stent problems like blockages or narrowing
- Controlling risk factors like high blood pressure and diabetes
- Making lifestyle changes like eating better and exercising
- Adjusting medicines to keep the heart healthy
Quality of Life with Five Stents
Having five stents is tough, but many people live well with the right care. A study in the Journal of the American College of Cardiology showed big improvements in symptoms and how well people could move.
Here’s how five stents can improve life:
| Aspect of Life | Pre-Stenting | Post-Stenting |
| Physical Activity | Limited due to angina | Improved ability to perform daily activities |
| Symptoms | Frequent angina episodes | Significant reduction in angina frequency |
| Medication | Multiple medications for symptom management | Optimized medication regimen to prevent complications |
Medical Monitoring Requirements
Patients with five stents need regular check-ups. These visits help keep an eye on the stents and adjust treatments as needed. This close watch is key to managing their care.
In summary, managing five stents in the heart is complex. But, with the right care, patients can live well. Understanding the needs and monitoring them closely helps healthcare teams provide the best care.
Can You Have 6 Stents in Your Heart? Exploring Extreme Cases
It’s rare, but some people have gotten six or more stents. This raises big questions about how far cardiac stenting can go. Doctors only consider this option after thinking a lot about the patient’s health and the disease’s severity.
Documented Cases of Six or More Stents
There are cases where patients got six or more stents. These are usually people with very complex heart disease. Often, they’ve had many heart attacks or have disease in many parts of their heart.
A study in a top cardiology journal showed cases with six to ten stents. These extreme cases show that, with the right care, people can live well with many stents.
Medical Decision-Making in Complex Cases
Deciding on multiple stents is a big deal. Doctors have to think about a lot of things. They look at the immediate need for stents and the long-term effects of having many.
Important factors include:
- The extent and severity of coronary artery disease
- The patient’s overall health and other medical conditions
- The patient’s lifestyle and ability to follow care instructions
- The possibility of other treatments, like CABG
Alternative Approaches When Multiple Stents Aren’t Ideal
In some cases, other treatments might be better than many stents. For complex heart disease, CABG might be a better choice than stenting.
Other options include:
- Improving medical treatment to manage symptoms and slow disease
- Making lifestyle changes, like diet and exercise
- Trying new technologies, like drug-coated balloons or bioabsorbable stents
Long-term Outcomes in Patients with Many Stents
Outcomes for patients with many stents vary. While there are risks, good care and follow-up can help a lot.
Important long-term care includes:
- Following antiplatelet therapy to prevent stent problems
- Regular check-ups with a cardiologist to watch stent health
- Making lifestyle changes to prevent more heart disease
Understanding the complexities of six or more stents helps us see the depth of heart care. It shows how important it is to tailor treatment plans to each person.
How Many Stents Can Be Placed in One Artery?
When thinking about stenting for coronary artery disease, a key question is: how many stents can go in one artery? The answer varies based on several technical and clinical factors.
Technical Limitations of Single-Artery Stenting
Putting multiple stents in one artery has big technical limits. Stent length and diameter are key in making decisions. Longer stents or stents that overlap can raise the chance of problems like in-stent restenosis or stent thrombosis.
We also look at the coronary artery’s shape and if it has calcium when deciding on multiple stent use.
Overlapping Stents: Benefits and Concerns
At times, we need to use overlapping stents for long or complex lesions. This method can work well but also has risks. It can fully cover the diseased area, possibly improving results. Yet, it might increase the risk of blood clots and restenosis because of the metal overlap.
A study in the Journal of the American College of Cardiology showed overlapping stents might lead to more heart problems than non-overlapping ones.
Case Examples of Multiple Stents in a Single Vessel
There are cases where putting multiple stents in one artery works well. For example, a patient with a long lesion in the left anterior descending artery might need two or more stents for full revascularization.
| Case | Number of Stents | Outcome |
| 1 | 2 | Successful revascularization with no complications at 1-year follow-up |
| 2 | 3 | Patient experienced in-stent restenosis requiring additional intervention |
| 3 | 1 | Optimal stent placement with good long-term results |
Risks Specific to Same-Artery Multiple Stenting
Putting multiple stents in the same artery has specific risks. These include a higher chance of stent thrombosis, restenosis, and possible complications during or after the procedure.
We balance these risks against the possible benefits when thinking about putting multiple stents in one artery. The choice depends on the patient’s health, the artery’s anatomy, and the nature of the lesions being treated.
Living with Multiple Heart Stents: Patient Experiences
Living with multiple heart stents changes your life in many ways. You have to adjust to new daily routines and ongoing medical care. With the right support, patients can live happy and fulfilling lives.
Daily Life and Activity Levels
Having multiple heart stents means making some lifestyle changes. But, most people can keep doing the things they love. Regular exercise and a balanced diet are key to keeping your heart healthy. Many patients feel better after the procedure.
For example, John, a 55-year-old, started hiking again after getting stents. “I was worried at first,” he said, “but my doctor said I could do my usual activities.”
Medication Requirements and Follow-up Care
Patients with multiple stents need to take medicines to prevent blood clots and manage heart health. Antiplatelet therapy is often used to stop stent blockages. It’s also important to see your doctor regularly to check on your stents and heart.
- Adherence to prescribed medication
- Regular check-ups with healthcare providers
- Monitoring for possible complications
Long-term Outcomes and Quality of Life
Long-term results for patients with multiple stents vary. But, many see a big improvement in their quality of life. The number of stents, where they are, and your overall health matter a lot.
A study in the Journal of the American College of Cardiology showed that with the right care, patients can do well long-term.
Psychological Aspects of Living with Multiple Stents
Having multiple heart stents can affect your mind, too. You might feel anxious or depressed. It’s important to get care that looks at your whole health. Support groups and counseling can help a lot.
“The emotional journey is just as important as the physical one. Support from family, friends, and healthcare professionals makes a big difference.”
— Dr. Jane Smith, Cardiologist
Understanding what patients go through with multiple heart stents helps us support them better. This way, we can help them improve their heart health and overall well-being.
Conclusion: Personalized Approach to Cardiac Stenting
Cardiac stenting is a procedure that’s tailored to each patient. We’ve looked at the basics of stents and their role. We’ve also explored the complexities of using more than one stent.
Every patient is different, and so is their treatment plan. Healthcare providers focus on what each patient needs. This way, they can create plans that improve health and quality of life.
Technology and medical practices in cardiac stenting have grown a lot. The number of stents needed varies. It depends on the disease’s severity and the patient’s health.
By tailoring cardiac stenting to each patient, we can offer better care. This leads to better health outcomes and happier patients.
FAQ
How many stents can a heart hold?
The number of stents a heart can hold varies. It depends on the patient’s needs and health. There’s no strict limit, but doctors decide based on disease severity and health.
What are the different types of cardiac stents available?
There are two main types of cardiac stents. Bare-metal stents are made of metal mesh. Drug-eluting stents release medication to prevent artery narrowing.
How many stents can be placed at one time?
The number of stents placed at once depends on the procedure’s complexity and the patient’s condition. Sometimes, multiple stents are placed in one go. Other times, procedures are done in stages.
What are the risks associated with having multiple stents?
Having multiple stents can increase the risk of bleeding and stent thrombosis. Restenosis is also a risk. But, the benefits of better blood flow and reduced symptoms often outweigh these risks for many.
Can you have 6 stents in your heart?
Yes, some patients have had 6 or more stents. This decision is made on a case-by-case basis. It depends on the patient’s needs and health.
How many stents can be placed in one artery?
The number of stents in one artery depends on the blockage’s length and complexity. Sometimes, multiple stents are used in one artery. This requires careful planning to minimize risks.
What is the recovery like after having multiple stents placed?
Recovery after multiple stent placement varies. It depends on the patient’s health and the procedure’s complexity. Patients are usually advised to rest for a few days and follow a medication regimen for healing.
How do multiple stents affect daily life and activity levels?
Many patients with multiple stents can lead active lives. They may need to make lifestyle changes like diet and exercise. Stress management is also important for heart health.
What are the long-term outcomes for patients with multiple stents?
Long-term outcomes for patients with multiple stents vary. They depend on health, medication adherence, and lifestyle changes. Regular follow-up care is key to monitor stent function and heart health.
Are there any psychological aspects to consider when living with multiple stents?
Yes, living with multiple stents can affect mental health. Anxiety and stress are common. Support from healthcare providers, family, and friends, along with stress management, can help patients cope.
References
Bicket, M. C., et al. (2013). Epidural injections for spinal pain: A systematic review and meta-analysis. Pain Physician, 16(5), E453-E470. https://pubmed.ncbi.nlm.nih.gov/24195874/





