Coronary artery disease affects millions globally. It often needs heart stents to improve blood flow. At Liv Hospital, we tackle this complex condition with care.
The number of stents varies by person. It depends on their body and overall health. Some people have several stents, but adding more is always decided carefully. Many patients ask, “how many stents can be placed in your heart?” — the answer depends on the severity of blockages, artery size, and how well the heart can handle additional stents safely.
We help our patients understand their options. We share the latest in cardiology. Our aim is to make the best choice for each patient, no matter how tough the case.
Key Takeaways
- The number of heart stents a person can have depends on individual factors, including anatomy and health.
- Patients with coronary artery disease may require multiple stents.
- The decision to place additional stents is made on a case-by-case basis.
- Personalized care is key in finding the best treatment.
- Cardiology keeps getting better, giving more options for treatment.
Understanding Heart Stents: Purpose and Function
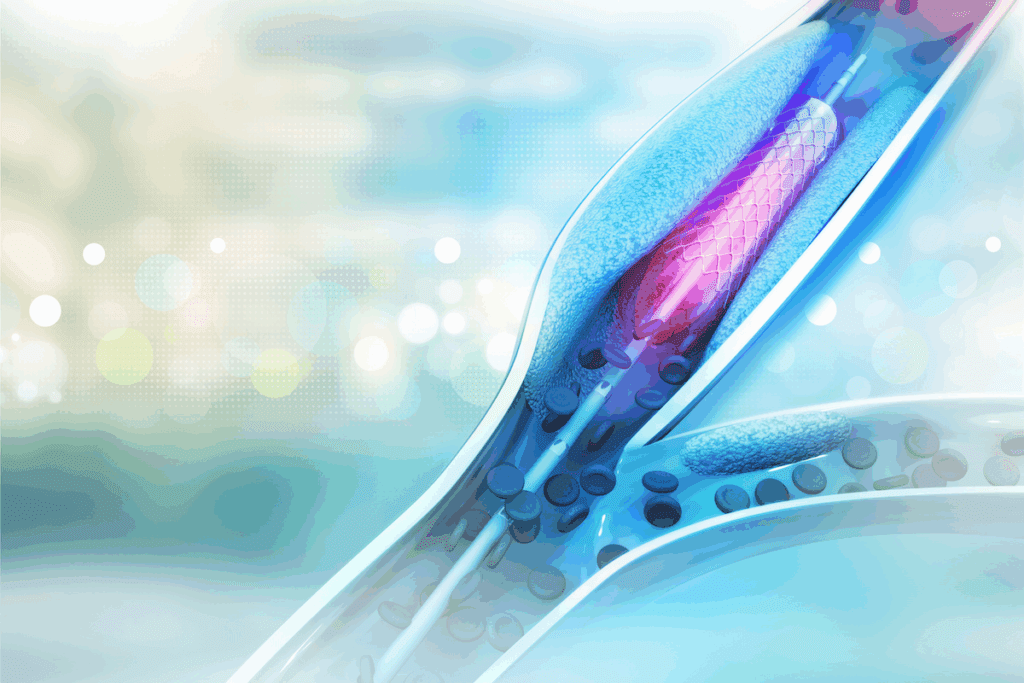
Keeping blood flowing to the heart is key, and coronary stents are vital for this. These small, mesh-like tubes keep arteries open. This ensures the heart gets the blood it needs.
What Are Coronary Stents and How Do They Work?
Coronary stents are used in angioplasty to open blocked arteries. A catheter is inserted, and a balloon is inflated to widen the artery. Then, a stent is placed to keep it open, improving blood flow.
The process involves several key steps:
- Insertion of a catheter into the blocked artery
- Inflation of a balloon to widen the artery
- Placement of a stent to keep the artery open
A study in the Journal of the American College of Cardiology found that stents are key in treating coronary artery disease. They significantly improve patient outcomes.
“The introduction of coronary stents has revolutionized the treatment of coronary artery disease, providing a safe and effective means of restoring blood flow to the heart.”
Types of Heart Stents Available Today
There are many types of heart stents, each with its own benefits. The main types include:
| Type of Stent | Description | Benefits |
| Bare-metal stents | Made of metal mesh | Simple design, less expensive |
| Drug-eluting stents | Coated with medication to prevent re-narrowing | Reduced risk of artery re-narrowing |
| Bioresorbable stents | Made of materials that dissolve over time | Potential for improved long-term outcomes |
Each stent type has its own benefits. Our medical team will choose the best one for you based on your condition.
How Many Stents Can Be Placed in Your Heart?
It’s important for doctors and patients to know about heart stent placement limits. The number of stents in a heart can vary a lot. This depends on many medical factors.
Is There a Maximum Limit to Heart Stent Placement?
There’s no fixed number of stents for everyone. But, in some cases, many stents can be safely put in. The choice depends on how bad the heart disease is and the patient’s health.
Important things to think about include:
- The size and location of blockages in the heart’s arteries
- The patient’s heart health
- Any other health issues that might affect the procedure or recovery
Single Procedure vs. Multiple Procedures
Choosing between one or many stent placements depends on several things. These include how complex the blockages are and the patient’s risk level.
Single procedure: This is often chosen for simple blockages in one area.
Multiple procedures: Needed for those with many blockages or complex heart disease.
Medical Considerations for Multiple Stent Placement
Several medical factors are important for placing many stents. These include:
- The shape and size of the heart’s arteries
- The severity of heart disease
- The patient’s overall health and risk for complications
Our medical team looks at these factors to decide the best plan for each patient. Sometimes, a heart may need 3 stents or more. This is to ensure blood flows well and to lower the risk of future heart issues.
Factors That Determine Stent Quantity in Coronary Arteries
Many factors decide how many stents a patient can get in their coronary arteries. Doctors look at the patient’s health, the shape, and how sick they are. This helps them choose the right treatment.
Anatomical Considerations and Vessel Structure
The shape and size of the coronary arteries matter a lot. How straight or curved they are, and if they have calcification, can affect stent placement.
Key anatomical considerations include:
- Vessel diameter and its suitability for stent placement
- Presence of calcification or thrombus
- Tortuosity or angulation of the coronary arteries
Extent and Location of Coronary Artery Disease
The size and where the disease is in the arteries also matter. People with disease in more than one artery might need more stents.
As noted by a leading cardiologist:
“The complexity and extent of coronary artery disease play a significant role in determining the number of stents required. A thorough assessment is critical for a good treatment plan.”
| Disease Extent | Typical Stent Requirement | Clinical Considerations |
| Single-vessel disease | 1-2 stents | Focus on treating the specific blockage |
| Multi-vessel disease | Multiple stents (3 or more) | Comprehensive assessment required; may involve staged procedures |
Overall Health and Risk Assessment
A patient’s health and risk factors, like diabetes and high blood pressure, are important. Doctors assess these to decide on the right number of stents.
They look at the patient’s age, other health issues, and medicines. This helps make a treatment plan that fits the patient’s needs.
Typical Scenarios: From 2 Heart Stents to Multiple Placements
Stents are key in treating blocked coronary arteries. The number of stents needed varies. This depends on the disease’s severity and the patient’s health.
Single-Stent Procedures: The Most Common Scenario
Often, just one stent is needed to clear a blockage. Single-stent procedures are the most common. They work well for patients with a single big blockage. These procedures usually have a high success rate and help patients recover quickly.
Two to Three Stents in Heart: Managing Multiple Blockages
Patients with many blockages might need two or three stents. Handling multiple blockages is complex. Cardiologists must plan carefully and execute precisely. We closely monitor patients and adjust treatment plans as needed.
Statistical Overview of Stent Placement Numbers
While single-stent procedures are common, many patients get multiple stents. About 20-30% of patients getting PCI get multiple stents. We keep up with the latest stats to give our patients the best care.
Knowing these scenarios helps us create treatment plans that fit each patient. This ensures the best outcomes for those with coronary artery disease.
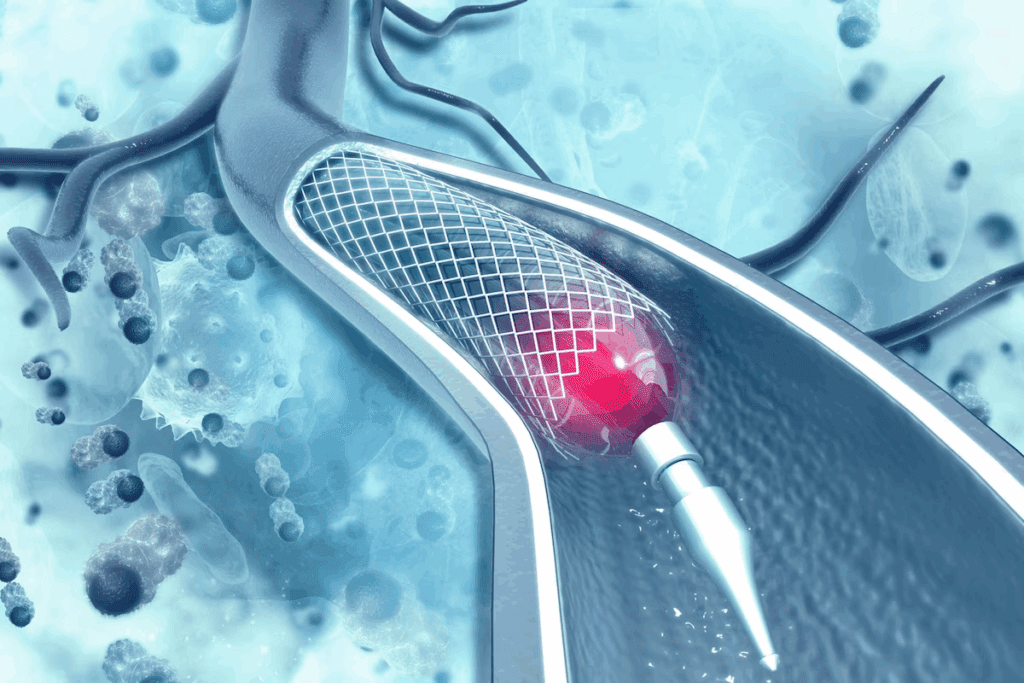
Multiple Stent Placement in a Single Artery
Putting multiple stents in one artery is a good option for people with complex heart disease. It’s a way to fix many blockages in one go. This helps get more blood to the heart.
How Many Stents Can Be Placed in One Artery?
The number of stents in one artery varies. It depends on the blockage’s length and complexity, and the patient’s health. Studies show it’s safe to put more than one stent in some cases.
A study in the Journal of the American College of Cardiology found that many patients get more than one stent. This is common practice.
“The safety and efficacy of multiple stent placement have been demonstrated in numerous studies, with outcomes comparable to those of single-stent procedures.”
| Factors Influencing Multiple Stent Placement | Description | Clinical Considerations |
| Blockage Length and Complexity | Longer or more complex blockages may require multiple stents. | Careful planning is necessary to ensure proper stent sizing and placement. |
| Artery Size and Structure | The size and tapering of the artery can affect stent placement. | Precise measurements are critical for the right stent size. |
| Patient’s Overall Health | Patients with comorbidities may need special treatment plans. | A full health check is key to finding the best treatment. |
Overlapping Stents: Benefits and Risks
Overlapping stents are used for long or complex blockages. They can be effective but also carry risks, like stent thrombosis.
Benefits of Overlapping Stents:
- They cover long or complex blockages fully.
- They can lead to better outcomes for multiple lesions.
Risks Associated with Overlapping Stents:
- They increase the risk of stent thrombosis.
- They might lead to higher rates of restenosis.
Procedural Limitations During a Single Session
While it’s possible to put multiple stents in one session, there are limits. Risks include contrast-induced nephropathy, radiation exposure, and procedural complications.
To reduce these risks, doctors plan carefully. They balance the need for full revascularization with the risks of long procedures.
Case Studies: From 3 Stents in the Heart to Complex Cases
Case studies on patients with many heart stents offer valuable insights. They show the challenges and successes in treating those with multiple stents. These real-life examples help us understand better.
Living with 3-4 Heart Stents: Patient Experiences
Patients with 3-4 heart stents face unique challenges. They need careful management, including sticking to their medication and making lifestyle changes. For example, a 55-year-old man with four stents reported a better quality of life after a year.
“I’m grateful for the second chance I’ve been given,” he said. “My cardiologist and I work together to monitor my condition closely, ensuring that I’m on the right track.”
5 Stents in Heart: Managing Complex Coronary Disease
Managing patients with 5 stents in their hearts needs a team effort. We look at the disease’s extent, the heart’s function, and any other health issues. A 65-year-old woman with five stents had a treatment plan that included medication, lifestyle changes, and regular check-ups.
Our team worked closely with her to adjust her treatment plan as needed, ensuring that she received the best care. “The key to managing complex coronary disease is a collaborative approach between the patient, cardiologist, and other healthcare professionals,” we emphasize.
Exceptional Cases: Patients with 6+ Stents in Their Heart
In some cases, patients have had six or more stents placed. These cases are often due to severe and complex coronary artery disease. We remember a patient who had seven stents over several years. Despite his complex condition, he has a good quality of life thanks to careful health management.
Such cases highlight the need for personalized care and ongoing research into treating complex coronary disease.
When Multiple Stents May Not Be Ideal: Alternative Approaches
For some patients, there are better options than multiple stents. Stenting is a common treatment for heart disease. But sometimes other methods work better.
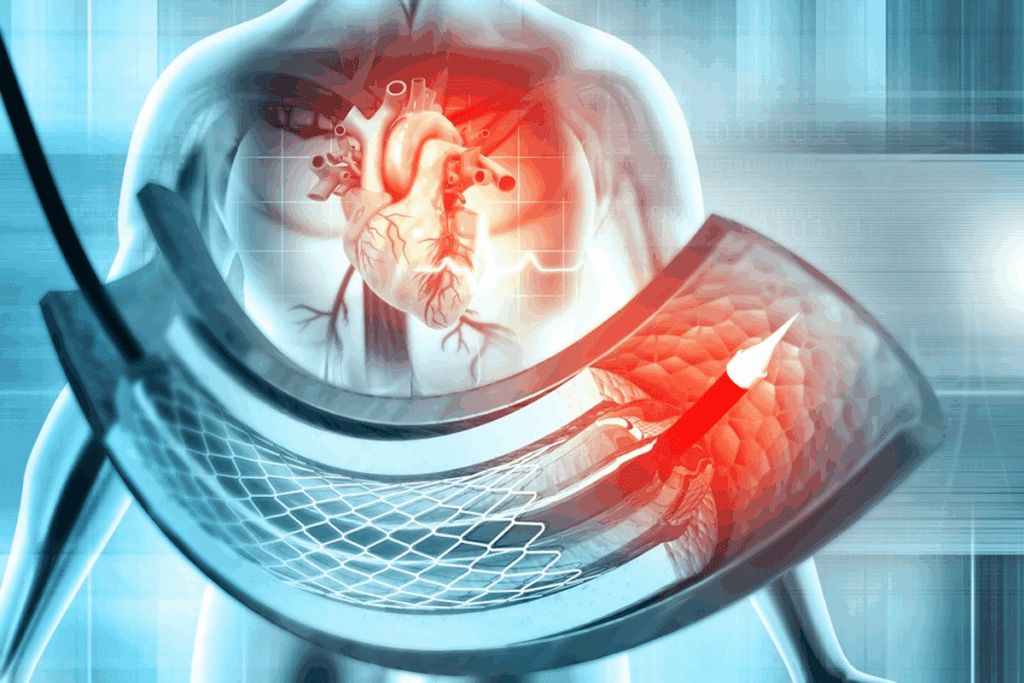
Coronary Artery Bypass Grafting vs. Multiple Stenting
Coronary artery bypass grafting (CABG) is a surgery that bypasses blocked arteries. It’s often used for complex cases, like those with diabetes or heart damage.
Choosing between CABG and stenting depends on several factors:
| Procedure | CABG | Multiple Stenting |
| Invasiveness | More invasive, requiring open-heart surgery | Less invasive, using minimally invasive catheter techniques |
| Recovery Time | Typically longer recovery period | Generally shorter recovery period |
| Long-term Outcomes | May offer more durable long-term results for complex cases | Effective for many patients, but may require repeat procedures |
Hybrid Procedures: Combining Stents with Other Treatments
Hybrid procedures mix different treatments for better results. This might include stents with CABG or other surgeries.
Hybrid methods have many benefits:
- Reduced risk of complications
- Improved long-term outcomes
- Tailored treatment plans to address individual patient needs
Medical Management Alternatives
Medical management is another option for some. It focuses on medication, lifestyle changes, and monitoring to manage symptoms and slow the disease.
Medical management includes:
- Aggressive risk factor modification (e.g., blood pressure and cholesterol control)
- Antiplatelet and anticoagulant therapy
- Lifestyle changes, such as diet, exercise, and smoking cessation
Healthcare providers can tailor treatments to meet each patient’s needs. This ensures the best care for everyone.
Living with Multiple Heart Stents: Recovery and Long-Term Care
The journey doesn’t end with the placement of multiple heart stents. It extends into a period of recovery and long-term care. Understanding the requirements and recommendations is key to optimal health outcomes.
Medication Requirements After Multiple Stent Placement
After getting multiple heart stents, patients need to take certain medications. These help manage their condition well. The medications may include:
- Antiplatelet therapy to prevent clot formation
- Statins to lower cholesterol levels
- Beta-blockers to reduce heart rate and blood pressure
- ACE inhibitors or ARBs to manage blood pressure
It’s important to take these medications as directed. This helps prevent complications and keeps the stents working right.
Activity Restrictions and Recommendations
After getting multiple stents, patients need to follow certain activity restrictions. These help with recovery and reduce risks. Some examples include:
| Activity | Recommendation |
| Exercise | Start with light exercises and gradually increase activity |
| Lifting | Avoid heavy lifting for a while, as advised by your doctor |
| Driving | Don’t drive for a bit if you were sedated during the procedure |
Following these guidelines helps ensure a smooth recovery. It also helps avoid complications.
Long-Term Prognosis and Follow-up Care
The long-term outlook for patients with multiple heart stents depends on several factors. These include overall health, the extent of coronary artery disease, and treatment adherence. Regular follow-up care is key for monitoring stent function and managing any issues.
It’s important to keep up with follow-up appointments with your healthcare provider. This ensures the best possible outcomes. By doing so, patients can live active and fulfilling lives even with multiple heart stents.
Conclusion: Personalized Approach to Heart Stent Placement
Every patient is different, needing a treatment plan that fits them perfectly. The number of stents needed in the heart changes a lot from person to person. This depends on how much heart disease they have and their overall health.
We’ve looked at the different parts of heart stent placement. This includes what coronary stents do and how many are needed. A plan that’s made just for you is key to getting the best treatment.
It’s important to talk to a doctor before getting heart stents. They can look at your situation and medical history. This way, you get a treatment plan that’s just right for you, making sure you’re safe and get the best results.
FAQ
How many stents can be placed in the heart?
The number of stents in the heart varies. It depends on the disease’s extent and the person’s health. Doctors decide based on the disease’s complexity and the patient’s condition.
Is there a maximum limit to heart stent placement?
There’s no fixed limit for heart stent placement. The decision to use multiple stents depends on several factors. These include the disease’s extent, the person’s health, and the artery’s anatomy.
How many stents can be placed in one artery?
The number of stents in one artery varies. It depends on the blockage’s length and complexity. Sometimes, more than one stent is needed to ensure blood flow.
What are the risks of having multiple stents in the heart?
Multiple stents can increase risks like bleeding and clotting. But the benefits often outweigh the risks, mainly for those with complex ddiseases
Can you have 6 stents in your heart?
Yes, some people might have 6 or more stents. This depends on the disease’s severity. Each case is unique, and doctors decide based on the patient’s needs.
How many stents can a person have in their heart?
The number of stents varies greatly. There’s no strict limit. The decision depends on the disease’s extent, the person’s health, and the artery’s anatomy.
What are the alternatives to multiple stent placements?
Alternatives include bypass grafting, hybrid procedures, and medical management. The best option depends on the patient’s condition and is decided with a healthcare provider.
How do I manage life with multiple heart stents?
Managing life with multiple stents requires careful attention. This includes the following medication, lifestyle, and follow-up care. Patients should work closely with their healthcare provider to manage their condition.
What are the long-term implications of having multiple stents?
The long-term implications vary. They depend on the condition, overall health, and treatment adherence. Regular follow-up care is key to monitoring and adjusting as needed.
Can I have multiple stents placed at the same time?
Yes, multiple stents can be placed at once. But the decision depends on the disease’s complexity and the patient’s condition.
References
- Suh, J., et al. (2010). The Relationship and Threshold of Stent Length With Mortality: A Multicenter Registry Study. American Journal of Cardiology, 106(12), 1767-1773. https://www.sciencedirect.com/science/article/pii/S1936879810001408