Knowing when a stent or bypass surgery is needed is key for both patients and doctors. At Liv Hospital, we focus on you, with top-notch care and the latest treatments. We make sure you get the best care tailored just for you.
A blockage of 70 percent or greater usually means a stent is needed. This is true if you have chest pain or if your heart isn’t getting enough blood. We’ll look at how serious the blockage is, your symptoms, and other personal factors to decide.
Our team uses the newest technology and methods to find and fix artery blockages. We aim for the best results for our patients. Many people ask, “how much blockage before stent?” — generally, a stent is considered when an artery is narrowed by 70% or more, especially if it causes chest pain or other heart-related symptoms.
Key Takeaways
- A blockage of 70 percent or greater is generally considered the threshold for stent placement.
- Symptoms like chest pain or evidence of reduced blood flow to the heart influence the decision to place a stent.
- Individual patient factors are also considered when determining the need for a stent or bypass surgery.
- Liv Hospital prioritizes patient-centered care with the highest standards of medical excellence.
- Our medical team uses the latest technology and techniques to diagnose and treat artery blockage.
Understanding Coronary Artery Disease and Blockages
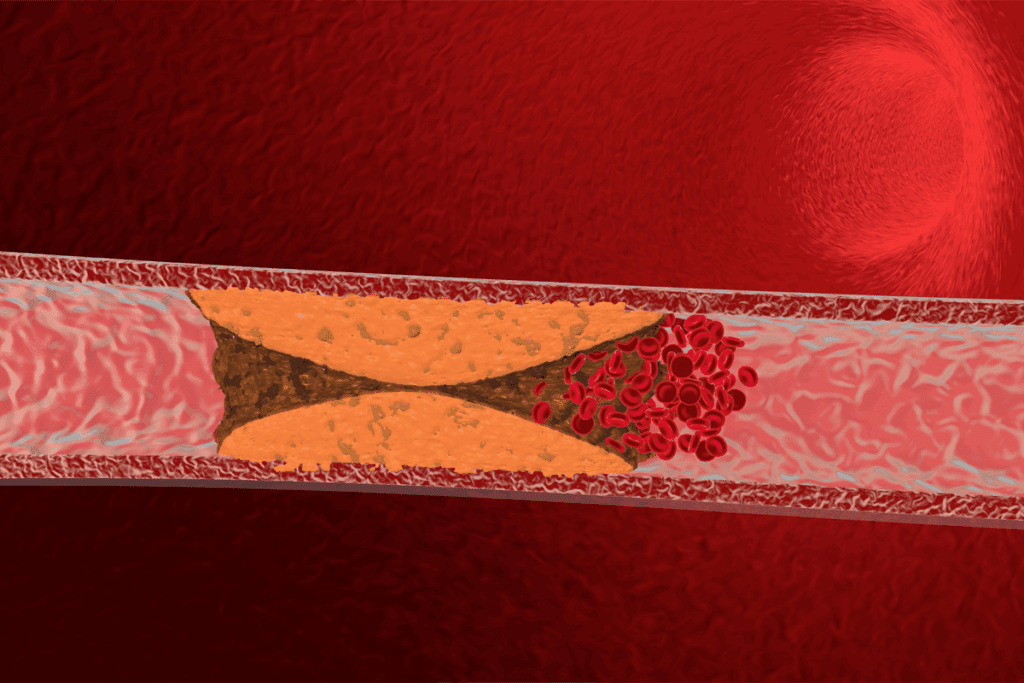
Coronary artery disease happens when the heart’s blood supply gets cut off. This is due to plaque buildup in the coronary arteries. The plaque is made of fat, cholesterol, and calcium.
How Arterial Blockages Form
A blockage in the heart occurs when plaque builds up in the arteries. This narrows them and cuts down blood flow to the heart. “Damage to the artery’s inner layer, often from smoking, high blood pressure, or high cholesterol, starts the process,” a top cardiologist explains.
Over time, this damage leads to plaque buildup. The artery then becomes less flexible and more likely to rupture. A significant blockage can reduce blood flow to the heart muscle, causing chest pain or a heart attack.
Measuring Blockage Percentage
The blockage percentage shows how much the artery is narrowed. It’s key in figuring out how severe the disease is and what treatment is needed. For example, a 50% blockage means half of the artery’s diameter is blocked by plaque.
Doctors use tests like angiograms to measure blockage percentage. An angiogram shows detailed images of the arteries. This lets doctors see the blockages and judge their severity.
Knowing how blockages form and how they’re measured helps patients understand their condition. It also guides treatment choices. We stress the role of these tests in making treatment plans.
The Significance of Blockage Percentages
The percentage of blockage in arteries is key to understanding heart disease. It helps doctors and patients decide on the right treatment. Knowing this helps everyone make better choices.
Mild Blockage: Under 50%
Mild blockages, under 50%, are often treated without surgery. Lifestyle changes and medication are the first steps. We suggest eating better, exercising more, and quitting smoking.
Most patients with less than 50 percent blockage get treated with medicine and lifestyle changes. This is based on guidelines that recommend a conservative approach for mild heart disease.
Moderate Blockage: 50-70%
Moderate blockages, 50-70%, need closer watch and sometimes more treatment. Regular check-ups and stress tests help track the blockage.
Stenting might be an option for moderate blockages if symptoms like angina appear. The decision to stent depends on the patient’s health and the blockage details.
Severe Blockage: Over 70%
Severe blockages, over 70%, often need stenting or bypass surgery. This is true if symptoms are bad or if the blockage is in a key artery. Bypass surgery is often chosen for complex blockages.
A blockage of 70% or more in a major artery like the LAD is urgent. We consider the patient’s health, symptoms, and blockage details to choose the best treatment.
Treatment plans are tailored to each patient. It’s not just about the blockage percentage. The patient’s health, symptoms, and wishes are also important. Working with their doctor helps patients make informed decisions.
How Much Blockage Before Stent Placement Is Considered?
The amount of blockage in a coronary artery is key in deciding if a stent is needed. We look at symptoms and the patient’s health to decide on a stent.
The 70% Threshold for Stent Intervention
Doctors usually suggest a stent for blockages over 70% if symptoms like angina or shortness of breath are present. This rule can change based on the patient’s situation.
Important factors for stent placement at 70% include:
- Signs of reduced blood flow to the heart.
- The patient’s overall health and medical history.
- The blockage’s location and complexity.
Exceptions to the 70% Rule
While 70% is a common threshold, there are exceptions. For example, blockages in the Left Anterior Descending (LAD) artery might be treated with stents at lower percentages. This is because they affect heart function a lot.
Other exceptions include:
- Patients with severe symptoms not controlled by medication.
- Blockages causing significant ischemia, shown by tests.
- Patients with a history of heart attack or other heart issues.
Every patient’s case is different. The decision to use a stent is made carefully, considering many factors beyond blockage percentage.
Symptoms That May Indicate Need for Intervention
It’s important to know the signs of heart blockage to get help quickly. The amount of artery blockage affects whether you need a stent or surgery. Let’s look at symptoms that show you might need medical help.
Chest Pain (Angina)
Chest pain, or angina, is a common sign of heart blockage. It happens when blood flow to the heart is low. Angina feels like pressure or squeezing in the chest and happens during effort, but goes away with rest.
If you get angina, talk to your doctor right away. They can figure out the best treatment for you.
Other Symptoms Indicating Reduced Blood Flow
Other signs show the heart might not get enough blood. These include:
- Shortness of breath, often when active or lying down
- Fatigue or feeling very tired or weak
- Pain or discomfort in the jaw, neck, arm, or back
These symptoms might be small, but they’re important. If you notice any, see a doctor to find out why and how to treat it.
Diagnostic Tests to Determine Blockage Percentage
Knowing the exact amount of artery blockage is key to treating heart disease. We use different tests to find out how much is blocked. This helps us decide the best treatment.
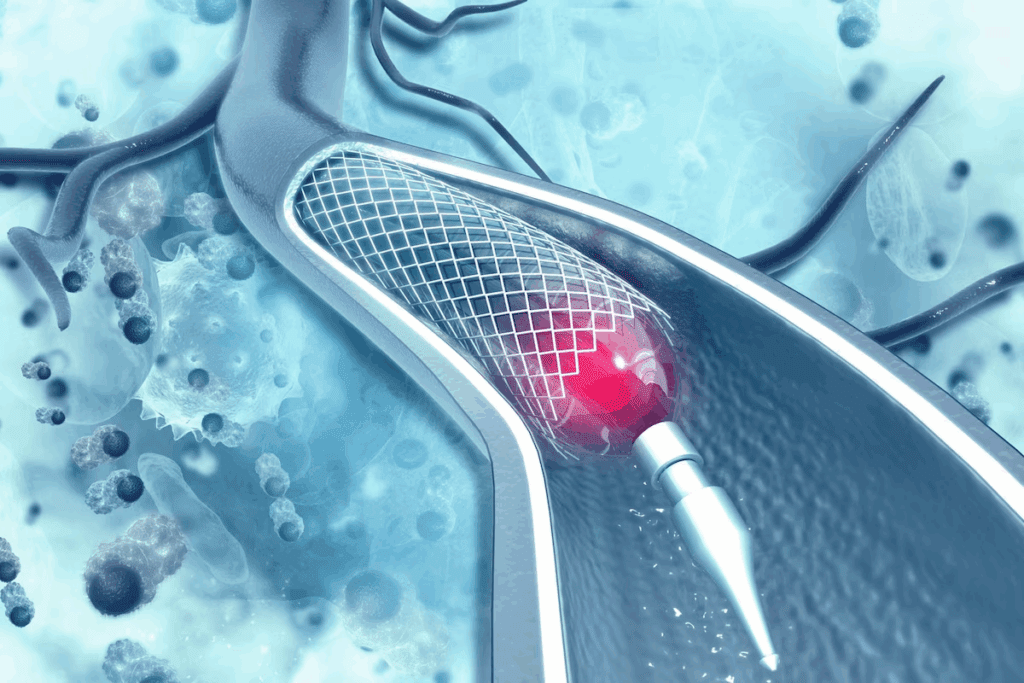
Angiograms and Their Role
An angiogram is a major tool for seeing the heart’s arteries. It shows where and how bad the blockages are. A dye is put into the arteries through a thin tube, and X-rays capture the blood flow.
This test tells us how much of the artery is blocked. It’s vital for deciding if a patient needs a stent or surgery.
Non-invasive Testing Methods
Along with angiograms, non-invasive tests are also important. They include stress tests, CT angiograms, and cardiac MRI.
- Stress Tests: These check how the heart works when stressed, usually through exercise or medicine. They spot areas that might not get enough blood.
- CT Angiograms: This uses CT scans to see the arteries and find blockages. It’s a safer choice than traditional angiography.
- Cardiac MRI: It uses magnetic fields and radio waves to make detailed heart images. This lets us check the heart’s shape and how it works.
These tests give us important information about the heart without needing to insert a tube. They help us make treatment plans and keep track of the disease.
Treatment Options for Different Blockage Percentages
The amount of artery blockage helps decide the best treatment. We choose between conservative management, stent placement, or bypass surgery. Each option depends on the blockage’s severity, symptoms, and health.
Conservative Management for Mild Blockages
For blockages under 50%, we often suggest conservative management. This approach includes lifestyle changes and medication. It aims to manage symptoms and slow disease growth.
- Lifestyle changes: Dietary adjustments, increased physical activity, smoking cessation, and stress management.
- Medication: Cholesterol-lowering drugs, beta-blockers, and antiplatelet agents to reduce the risk of heart attack and stroke.
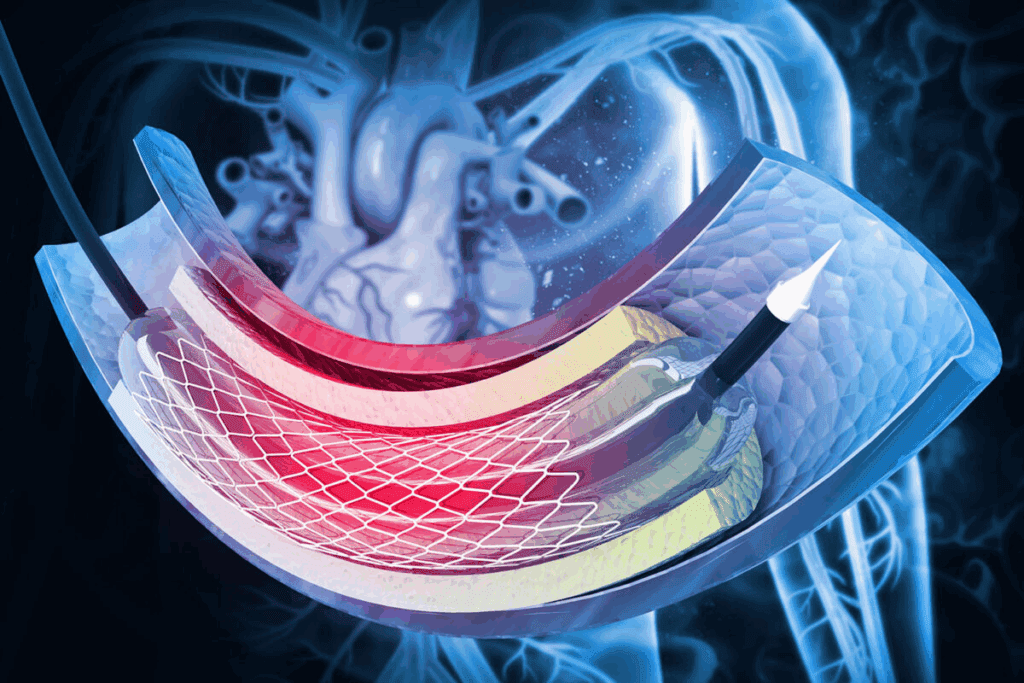
Stent Placement for Moderate to Severe Blockages
Blockages between 50-70% or higher may need stent placement. This involves placing a small, mesh-like tube (stent) in the artery. It keeps the artery open and improves blood flow.
| Blockage Percentage | Treatment Approach | Key Considerations |
| <50% | Conservative Management | Lifestyle changes, medication |
| 50-70% | Stent Placement | Symptom severity, overall health |
| >70% | Stent Placement or Bypass Surgery | Complexity of blockage, patient’s health status |
Stent placement is often recommended for significant symptoms or high heart attack risk. The decision to use stenting depends on symptoms, health, and other medical conditions.
Bypass Surgery Considerations
Bypass surgery, or CABG, is for complex or multiple blockages. It’s also considered when stenting is not possible. This surgery creates a detour around the blocked artery using a graft.
CABG is recommended for patients with:
- Multiple blockages in different coronary arteries.
- Complex blockages that are difficult to treat with stenting.
- Diabetes or other comorbidities that increase surgical risk.
The American Heart Association says, “CABG can improve survival and reduce symptoms in certain high-risk patient populations.”
The Left Anterior Descending (LAD) Artery: Special Considerations
The LAD artery is key to the heart’s blood flow. It needs quick action when blocked. This artery is vital for the heart’s oxygen and nutrient supply.
Why LAD Blockages Are Treated More Aggressively
LAD artery blockages are treated with urgency. They can harm a big part of the heart. This can cause a heart attack.
Doctors take a proactive approach to these blockages. They consider the patient’s health, symptoms, and blockage size when choosing treatment.
What Percentage of LAD Blockage Requires a Stent
Deciding on a stent for the LAD artery depends on several factors. These include blockage size, symptoms, and overall health. A blockage of 50% or more might require a stent if the patient is showing symptoms or has ischemic signs.
Stenting might also be considered for blockages less than 50% if there are high-risk features. Or if the patient has a history of heart disease and previous treatments. The decision varies based on the patient’s specific situation and the cardiologist’s judgment.
Every treatment plan for LAD artery blockage is unique. The patient’s age, other health issues, and personal preferences are all important. These factors help decide the best treatment approach.
When Bypass Surgery Is Preferred Over Stenting
The choice between bypass surgery and stenting depends on several factors. These include the complexity of the blockage.
We choose bypass surgery for patients with complex coronary artery disease. This is true for those with multiple vessel blockages or anatomy not good for stenting.
Complex and Multiple Vessel Blockages
Patients with many blockages or complex diseases often do better with bypass surgery. Stenting may not work as well for multiple blockages at once.
Stenting alone can struggle with long or complex blockages. Bypass surgery offers a more thorough solution in these cases.
| Characteristics | Bypass Surgery | Stenting |
| Complex Blockages | More effective for multiple or complex lesions | Limited by the number and complexity of lesions |
| Multiple Vessel Disease | Preferred treatment for multiple vessel involvement | May not be as effective for multiple-vessel disease |
Unsuitable Anatomy for Stenting
Some patients have an anatomy not right for stenting. This includes heavily calcified arteries or hard-to-reach lesions.
Bypass surgery is a good option for these cases. It lets surgeons go around the blocked parts.
Diabetes and Other Risk Factors
Patients with diabetes and other health issues might do better with bypass surgery. Research shows diabetic patients with complex disease do better with bypass than stenting.
Other health factors, like high blood pressure and cholesterol, also matter. We think about these when choosing between bypass and stenting.
Understanding what makes bypass surgery or stenting better helps us tailor care. We aim to meet each patient’s unique needs.
Is 70 Percent Heart Blockage Dangerous?
A 70 percent blockage in the coronary arteries is very dangerous and needs quick medical help. Such a blockage greatly raises the risk of heart problems, like heart attacks.
Getting a 70 percent heart blockage diagnosis can be scary. It’s important to know the risks and what the future might hold. This helps you make the best choices for your health.
Immediate Risks of Severe Blockage
A blockage of 70 percent or more in the coronary arteries is very serious. It’s a big risk to your heart health. The biggest worry is the chance of a heart attack.
Key immediate risks include:
- Acute coronary syndrome
- Myocardial infarction (heart attack)
- Unstable angina
- Sudden cardiac death
These dangers are high because a big blockage limits blood to the heart. This can harm or kill heart tissue.
Long-term Prognosis Without Intervention
Without the right treatment, the outlook for a 70 percent heart blockage is not good. The chance of heart attacks and needing emergency care goes up a lot.
| Treatment Approach | Short-term Benefits | Long-term Benefits |
| Conservative Management | May reduce symptoms temporarily | Limited long-term benefit; may not prevent future cardiac events |
| Stent Placement | Restores blood flow immediately | Reduces risk of future cardiac events; improves long-term survival |
| Bypass Surgery | Provides a detour around blocked arteries | Can significantly improve long-term survival and reduce cardiac event risk |
It’s key to get medical help fast and get the right treatment. With the right care, people with a 70 percent heart blockage can greatly improve their chances. They can also lower the risk of heart problems in the future.
Comparing Stent Placement and Bypass Surgery
Coronary artery disease can be treated in two main ways: stent placement and bypass surgery. Both are good options, but they differ in recovery time, how invasive they are, and long-term results.
Recovery Time and Procedure Invasiveness
Stent placement is less invasive than bypass surgery. It uses a catheter to put a stent in the blocked artery. This usually takes about an hour and is done under local anesthesia. Patients often go home within a day or two.
Bypass surgery, being more invasive, requires open-heart surgery. It takes longer, often several hours. Recovery is longer, with hospital stays of several days to a week or more.
Long-term Outcomes and Durability
Stent placement can work well for years, but there’s a chance the artery could block again. New stent technologies, like drug-eluting stents, have made this less likely.
Bypass surgery, though more invasive, can last longer. It’s better for complex or multiple blockages. The grafts can stay open for years, improving survival and reducing the need for more surgeries.
Selecting the Right Procedure Based on Blockage Percentage
Choosing between stent placement and bypass surgery depends on several factors. These include the blockage percentage, symptoms, and the patient’s health. For example, those with blockages over 70% might do better with bypass surgery for complex or multiple blockages.
| Procedure | Recovery Time | Invasiveness | Long-term Outcomes |
| Stent Placement | 1-2 days | Less invasive | Effective for many years; risk of restenosis |
| Bypass Surgery | Several days to a week or more | More invasive | More durable long-term results; improved survival |
The choice between stent placement and bypass surgery should be made carefully. It depends on the patient’s condition, preferences, and the doctor’s advice.
Individual Factors That Influence Treatment Decisions
Choosing the right treatment for coronary artery disease is complex. It’s not just about the blockage percentage. Many personal factors are considered to make sure the treatment fits the patient perfectly.
Age and Overall Health
A patient’s age and health are key in deciding treatment. Older adults or those in poor health might need gentler or more intense treatments. We look at their health and any conditions that could affect surgery or recovery.
- Physiological age versus chronological age
- Presence of other health conditions
- Physical resilience and recovery ability
Comorbidities and Risk Factors
Conditions like diabetes, high blood pressure, or kidney disease play a big role. They can change the risk of surgery and how well it works. We check these factors to pick the best treatment.
- Diabetes and its effect on heart health
- Hypertension and its impact on surgery risks
- Kidney disease and its treatment implications
Patient Preferences and Quality of Life
What the patient wants and their quality of life are also important. We talk with patients to understand their values and goals. This helps us choose a treatment that fits their life and expectations.
For example, someone who wants a quick recovery might choose a stent. But someone focusing on long-term results might prefer bypass surgery.
By looking at these personal factors, we create a treatment plan that works for the patient. It treats the disease well and respects the patient’s unique situation and wishes.
Conclusion
Understanding when a stent or bypass surgery is needed is complex. It’s not just about the blockage percentage. Symptoms, patient health, and new treatments also play a big role.
The choice between a stent and surgery depends on several things. These include how severe the blockage is, the symptoms, and the patient’s overall health. Knowing these factors helps both patients and doctors make better choices.
In short, a 70% blockage might need treatment, but it’s not the only thing to consider. We aim to help patients and families understand coronary artery disease treatment. This way, they can make choices that fit their specific needs.
FAQ
What percentage of artery blockage requires a stent?
A blockage of 70 percent or more usually needs a stent. This is true if you have chest pain or if blood flow to the heart is reduced.
At what percent blockage requires a stent?
While 70% is a common threshold, there are exceptions. For example, stents might be used at lower percentages if the blockage is in a critical artery or if symptoms are severe.
What percentage of LAD blockage requires a stent?
Blockages in the LAD artery are treated more aggressively. This is because they can lead to severe consequences. So, stenting might be considered at lower percentages to prevent serious outcomes.
Is 70 percent heart blockage dangerous?
Yes, a 70 percent heart blockage is dangerous. It’s linked to a high risk of heart attack. Without treatment, the outlook is generally poor.
What percentage of blockage requires bypass surgery?
Bypass surgery is often chosen for complex blockages or multiple-vessel disease. The decision depends on the blockage percentage and the patient’s overall health.
How much blockage is considered severe?
Severe blockages are those over 70%. They often need aggressive treatments like stenting or bypass surgery. This is true if symptoms are significant or if the blockage is in a critical artery.
What are the symptoms of reduced blood flow to the heart?
Common symptoms include chest pain or angina, triggered by exertion and relieved by rest. Other signs include shortness of breath, fatigue, and discomfort in the jaw, arm, or back.
How is the percentage of blockage measured?
Tests like angiograms show detailed images of the coronary arteries. This lets doctors assess blockage percentages. Non-invasive tests also provide useful information without the need for catheterization.
What is the difference between stent placement and bypass surgery?
Stent placement is less invasive and has a quicker recovery. Bypass surgery is more invasive but might offer better long-term results, mainly for complex or multiple blockages.
What factors influence treatment decisions for coronary artery disease?
Treatment choices are highly individualized. They consider factors like age, health, comorbidities, risk factors, patient preferences, and quality of life, beyond just the blockage percentage.
References
- Mahadevan, K., et al. (2021). Factors influencing stent failure in chronic total occlusion percutaneous coronary intervention: A multicenter analysis. European Heart Journal. https://pmc.ncbi.nlm.nih.gov/articles/PMC8532005/








