
Getting a correct diagnosis is key to managing sickle cell anemia well. At Liv Hospital, we use the latest genetic and laboratory testing methods. This ensures patients get top-notch care every step of the way.
To diagnose this condition, we combine lab tests and genetic screening. Our team helps patients understand each step. From the first check-up to the final tests, we make sure you know what’s happening.

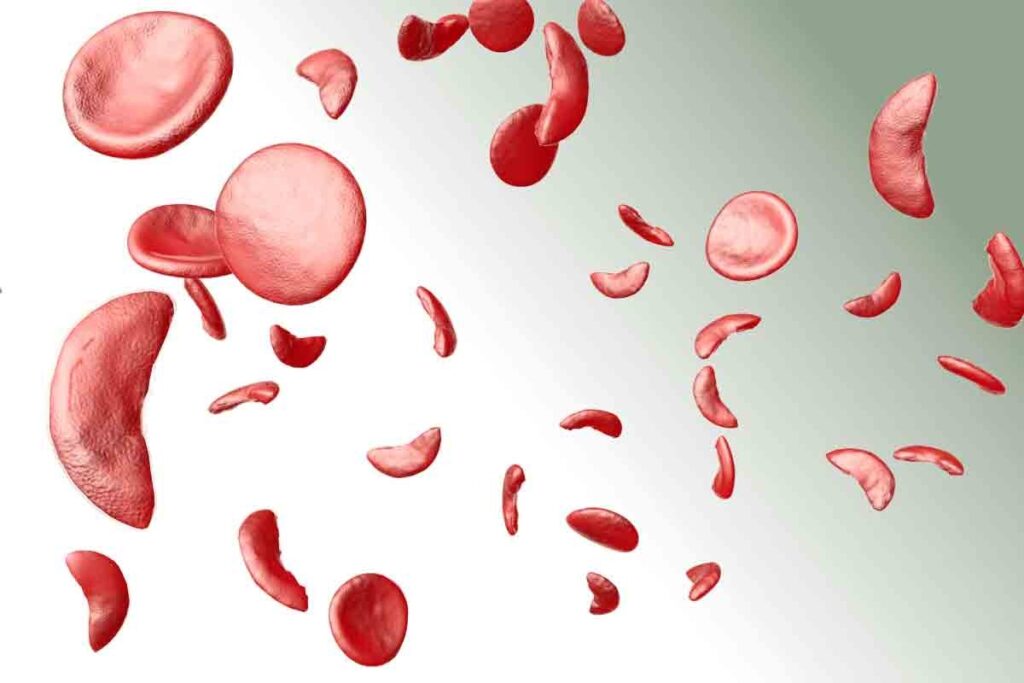
To diagnose sickle cell anemia, we need to know its genetic roots and how it affects red blood cells. This disease is caused by a mutation in the HBB gene. This mutation leads to abnormal hemoglobin, known as sickle hemoglobin or HbS.
Sickle cell disease is passed down in an autosomal recessive pattern. This means a person needs two defective HBB genes to have the disease. Carriers, with one normal and one defective gene, usually don’t show symptoms but can pass the mutated gene to their kids.
Genetic testing can spot carriers and those with the disease early. This allows for early treatment and management. Recent data shows genetic testing is key in diagnosing and managing sickle cell disease.
Abnormal hemoglobin (HbS) makes red blood cells sickle-shaped when oxygen levels are low. These sickled cells are more likely to break down and can block small blood vessels. This can cause many problems.
Getting sickle cell anemia diagnosed early and accurately is key to managing it well. It lets doctors start treatments like vaccinations and antibiotics early. This helps prevent serious problems.
“Early diagnosis and complete care can greatly improve life quality for those with sickle cell disease.”
It’s vital to grasp the genetic cause of sickle cell disease and its effects on red blood cells for early and correct diagnosis. This way, doctors can give focused care and support to those affected.
Diagnosing sickle cell anemia starts with a thorough clinical assessment. We look at the patient’s symptoms, family history, and physical exam. This helps us find those who need more tests.
Symptoms of sickle cell anemia vary from person to person. Common signs include pain crises, infections, and anemia. Spotting these symptoms is key to diagnosing the disease.
Looking into a patient’s family history is vital. Sickle cell anemia is passed down through genes. If family members have it, the patient is more likely to have it too.
We ask about:
Physical exams can give us important clues. We check for jaundice, pallor, and splenomegaly. These signs are linked to sickle cell anemia.
To accurately diagnose sickle cell anemia, healthcare professionals use a detailed testing process. This involves different diagnostic methods.
The testing starts with a complete blood count (CBC). It may also include peripheral blood smear analysis and genetic testing. These tests help find abnormal hemoglobin and check the health of red blood cells.
Genetic testing is key in diagnosing sickle cell anemia. It finds the genetic mutation causing the condition. This info is important for confirming the diagnosis and understanding the risk of passing it to future generations.
Testing for sickle cell anemia is recommended for those showing symptoms like pain, anemia, or infections. It’s also suggested for those with a family history of the disease.
Newborn screening programs are vital for early detection. They help find affected babies early, leading to better care and outcomes.
The journey to diagnose sickle cell anemia involves several steps. It starts with screening tests like CBC to spot possible issues. Then, more specific tests like hemoglobin electrophoresis or HPLC (High-Performance Liquid Chromatography) confirm the diagnosis.
After confirming the diagnosis, we create a management plan. This plan includes monitoring, preventive steps, and treatments to manage symptoms and prevent complications.
A complete blood count (CBC) is the first step in diagnosing sickle cell disease. This test gives insights into the blood cell count. It helps doctors spot any signs that might point to sickle cell anemia.
CBC results show important details about hemoglobin levels and red cell indices. In sickle cell disease, the CBC might show low hemoglobin levels. This is because the body tries to make up for the lack of red blood cells by producing more.
The CBC also looks at red cell indices like mean corpuscular volume (MCV) and mean corpuscular hemoglobin concentration (MCHC). These can be different in sickle cell disease. They help doctors understand the severity of the anemia and if there are other blood disorders.
Doctors look for signs of sickle cell disease in CBC results. Low hemoglobin levels are common because the abnormal hemoglobin (HbS) damages red blood cells. The red cell indices can also give clues, like a high MCHC in sickle cell disease due to dehydrated red blood cells.
Even though the CBC is useful, it’s not enough on its own to diagnose sickle cell disease. It can only suggest the presence of the disease. So, more tests are needed to confirm the diagnosis.
The table below shows what CBC can find in sickle cell disease and its limits:
| CBC Parameter | Typical Findings in Sickle Cell Disease | Implication |
| Hemoglobin Level | Low | Anemia |
| Reticulocyte Count | Elevated | Compensatory response to anemia |
| MCV | Variable | May indicate other hemoglobinopathies |
| MCHC | High | Dehydration of red blood cells |
| Diagnostic Capability | Suggestive but not definitive | Need for confirmatory tests |
Peripheral blood smear analysis helps doctors diagnose sickle cell anemia. They look at red blood cells under a microscope. This method checks for any odd shapes or sizes in the cells.
Looking at a blood smear, doctors aim to spot sickled cells. These cells look like crescents or sickles. Sickled cells are a key sign of sickle cell disease.
To find these cells, lab techs must prepare the smear carefully. They use the right tools and look closely. Here’s how:
Doctors also look for other odd cell shapes. These can include:
These signs help doctors confirm sickle cell disease. They might also point to other conditions.
Even with blood smear analysis, sometimes it’s hard to get a clear answer. This can happen if:
In these cases, doctors might need more tests. These could include hemoglobin electrophoresis or molecular testing.
To confirm a diagnosis of sickle cell disease, several advanced laboratory tests are used. These tests are key to identifying the specific type of hemoglobinopathy and confirming the diagnosis.
Hemoglobin electrophoresis is the top choice for diagnosing sickle cell disease. It separates different types of hemoglobin by their electrical charge. This helps identify abnormal hemoglobin variants, like HbS, which causes sickle cell disease. As noted by a leading medical expert, “Hemoglobin electrophoresis remains the cornerstone of diagnosis due to its high accuracy and reliability.”
The process involves applying a blood sample to a gel or cellulose acetate strip and applying an electric field. The different hemoglobin types move at different rates, creating distinct bands. These bands can be seen and measured. This method is very good at telling different hemoglobinopathies apart, including sickle cell trait and disease.
High-Performance Liquid Chromatography (HPLC) is also key in diagnosing sickle cell disease. HPLC separates and quantifies hemoglobin variants based on their ionic properties. It gives a detailed look at the different hemoglobin types in a patient’s blood. This technique is great for finding small amounts of abnormal hemoglobin and is often used with hemoglobin electrophoresis.
HPLC has many benefits, like high precision and the ability to automate the process. “HPLC has revolutionized the field of hemoglobinopathy diagnosis by providing rapid and accurate results.”
Isoelectric focusing separates proteins based on their isoelectric point (pI). In sickle cell disease, it’s used to identify and quantify different hemoglobin variants. This method is very sensitive and can spot small differences in hemoglobin structure. It’s very useful for diagnosing complex cases.
Isoelectric focusing is mainly used in research and specialized labs because of its technical complexity. But, it’s a valuable tool in diagnosing sickle cell disease.
It’s important to tell sickle cell trait apart from disease. Sickle cell trait is usually harmless, but sickle cell disease can cause serious health issues. Getting the right diagnosis is key to giving the right care and advice.
There are several ways to test for sickle cell trait. These include hemoglobin electrophoresis and high-performance liquid chromatography (HPLC). These tests spot abnormal hemoglobin in the blood.
Quantitative analysis is key to tell sickle cell trait from disease. It measures the levels of different hemoglobin types. This helps doctors see how severe the condition is.
Key aspects of quantitative analysis include:
Rapid tests, like the HemoTypeSC assay, are quick and reliable for diagnosing sickle cell trait and disease. They’re great in places where lab tests are hard to get.
“Rapid diagnostic tests for sickle cell disease are key for early detection and care, mainly in areas with little lab setup.”
It’s important to know the differences in sickle cell trait and disease for patient care. People with sickle cell trait usually don’t have symptoms. But those with sickle cell disease face serious risks.
| Condition | Clinical Implications |
| Sickle Cell Trait | Usually doesn’t cause symptoms, but might under extreme conditions. |
| Sickle Cell Disease | At risk for serious problems, like pain crises, infections, and organ damage. |
Genetic testing is key to accurately diagnosing sickle cell disease. These advanced methods have changed how we understand and manage hemoglobinopathies.
DNA analysis is vital for sickle cell disease diagnosis. Polymerase Chain Reaction (PCR) is a main technique. It amplifies DNA sequences to spot the genetic mutations causing the disease. PCR-based methods are highly sensitive and specific, leading to early and accurate diagnosis.
Medical Expert, “Genetic testing is essential for sickle cell disease diagnosis. It gives valuable info for patients and healthcare providers.”
“Genetic testing is not just about diagnosis; it’s about understanding the genetic basis of the disease, which is key for family planning and management.”
Next-generation sequencing (NGS) has changed genetic diagnostics. NGS lets us analyze many genes at once. It’s a powerful tool for complex conditions like sickle cell disease. This technology gives a full view of an individual’s genetic risks.
Genetic counseling is vital after genetic testing for sickle cell disease. It gives patients and their families critical info about their test results. Counselors help people understand their risks and make informed health choices.
The field of genetic diagnosis is always growing, with new tech emerging. Technologies like CRISPR gene editing promise future therapeutic breakthroughs. As these technologies improve, we can look forward to better diagnosis and treatment of sickle cell disease.
Screening programs are key for catching sickle cell disease early. They help in preventive healthcare, spotting sickle cell trait or disease. This is very important.
Newborn screening for sickle cell disease is common in many countries, like the United States. It’s vital for starting care early. This can greatly help babies with the disease.
The test is a blood sample taken right after birth. It looks for abnormal hemoglobin levels. These levels can show if a baby has sickle cell disease or trait.
| State | Newborn Screening Method | Follow-up Testing |
| California | HPLC or IEF | Confirmatory testing for abnormal results |
| New York | HPLC | Genetic counseling and further testing |
| Florida | IEF or HPLC | Repeat testing and family screening |
Prenatal testing for sickle cell disease is available. It gives families at risk important information. We offer CVS and amniocentesis to check the fetus.
These tests are vital for families with sickle cell history. They help families make informed choices about their pregnancy.
Point-of-care testing has made diagnosing sickle cell disease better, even in tough settings. We see new, quick, and portable tests coming up. They can accurately diagnose the disease.
These tests help doctors make quick care decisions. This improves health outcomes for those with sickle cell disease.
Key benefits of point-of-care testing include:
Getting a correct diagnosis of sickle cell anemia is key to managing the disease well. Knowing the disease helps us give people the care they need to live better lives. Early detection and action can greatly improve how well someone can manage their condition.
After getting a diagnosis, we take a detailed approach to managing sickle cell disease. This includes keeping an eye on health, sticking to medication, and making lifestyle changes. We work with each person to create a care plan that fits their specific needs.
We use the latest medical technology and research to better understand sickle cell anemia. Our aim is to offer top-notch healthcare and support. This way, we help people manage their condition and live happy, fulfilling lives.
The first step is a thorough clinical assessment. This includes looking for symptoms like pain crises and infections. It also involves checking family history and doing physical exams for signs like jaundice or an enlarged spleen.
To diagnose sickle cell anemia, several tests are used. First, screening tests like a CBC and blood smear are done. Then, genetic tests like hemoglobin electrophoresis, HPLC, and isoelectric focusing confirm the diagnosis.
A CBC is often the first test for sickle cell anemia. It shows important information about hemoglobin levels and red cell indices. This can suggest abnormal hemoglobin.
To tell sickle cell trait from disease, specific tests are used. These include tests that analyze hemoglobin types and rapid tests like the HemoTypeSC assay. It’s important to understand the difference for proper patient care.
Genetic testing for sickle cell disease uses advanced DNA analysis. It provides detailed genetic information about the disease. Genetic counseling is also key after testing.
There are several screening programs for sickle cell disease. These include newborn screening, prenatal testing, and point-of-care testing. These help in early detection and management.
Newborn screening protocols diagnose sickle cell disease early. This allows for timely management and care.
Peripheral blood smear analysis examines red blood cells under a microscope. It looks for sickled cells and other abnormalities. While it’s helpful, sometimes blood smears may not be conclusive.
Confirmatory tests for sickle cell disease include advanced techniques like hemoglobin electrophoresis, HPLC, and isoelectric focusing. These tests provide a definitive diagnosis by identifying specific hemoglobin types.
Early and accurate diagnosis of sickle cell anemia greatly improves quality of life. It allows for proper management and support.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us