Last Updated on October 30, 2025 by mcelik
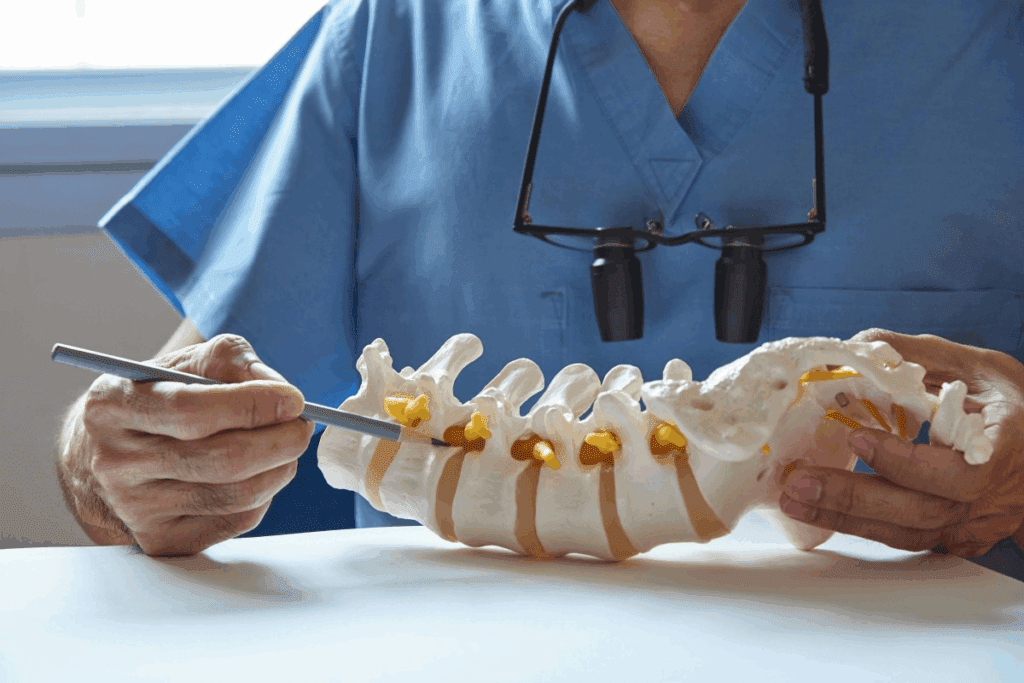
Discover how to heal a fractured vertebrae. Our guide covers proven steps for L1 compression and lumbar fracture treatment for a safe recovery.
A fractured vertebra can really change your life. It can mess with your posture, how you move, and how you feel overall. Seeing a spine expert early is key to getting better.
To fix a vertebral fracture, you need a plan that fits you. Liv Hospital has a new way to treat L1 and lumbar fractures. It’s all about you and getting better.

It’s important to know about vertebral fractures to get the right treatment. These fractures can really affect someone’s life if not treated well.
There are different kinds of vertebral fractures, each with its own level of severity. The main types are:
The lumbar spine and thoracic spine are where vertebral fractures often occur. The lumbar area, being a weight-bearing part, is more prone to fractures, like at L1 and L2. The thoracic spine can also get fractures, mainly at the thoracolumbar junction.
Trauma, like from a fall or car crash, is a big reason for vertebral fractures. Osteoporosis, which makes bones weak, also raises the risk of fractures. In people with osteoporosis, even small stresses can cause a fracture.
There are several things that can make someone more likely to get a vertebral fracture. These include:
Knowing about these causes and risk factors is key to preventing and managing vertebral fractures, mainly in people who are at higher risk.

Spotting vertebral fractures early is key to better treatment. Catching it early helps manage the condition and avoid more problems.
The pain from vertebral fractures can feel sharp or dull. It often gets worse when you move. Sometimes, it’s a constant, dull ache.
Key characteristics of pain include:
Vertebral fractures can also cause nerve problems. This might lead to numbness, tingling, or weakness in your limbs.
Seek medical help right away if you notice:
Doctors use a few ways to find vertebral fractures. X-rays are usually the first step. But, MRI or CT scans might be needed for a closer look.
| Imaging Modality | Use in Diagnosing Vertebral Fractures |
| X-ray | Initial assessment of bone structure and alignment |
| MRI | Detailed evaluation of soft tissues and nerve compression |
| CT Scan | High-resolution imaging of bone fragments and fracture severity |
It’s important to know how bad the fracture is. This helps decide the best treatment. Doctors look at how much the bone is collapsed and if nerves are affected.
The first steps in treating vertebral fractures include a mix of pain management and care for the patient. It’s key to manage pain well, keep the patient comfortable, and help them recover.
For acute vertebral fractures, getting emergency care is essential. Quick medical help is needed to check the fracture’s severity and stabilize it. Emergency responders should handle patients with suspected vertebral fractures with care to avoid further injury. At the hospital, a detailed check-up and imaging studies are done to see how bad the fracture is.
Managing pain is a big part of the initial treatment. There are many medication options to help with pain, from simple over-the-counter drugs to stronger prescription ones for more pain. The right medicine depends on how bad the pain is, the patient’s health history, and other factors.
| Medication Type | Use Case | Benefits |
| Over-the-counter analgesics | Mild to moderate pain | Easily accessible, effective for initial pain relief |
| Prescription pain medications | Moderate to severe pain | Stronger pain relief for more severe fractures |
Rest and changing how active you are are key parts of the treatment plan. Patients should avoid heavy lifting, bending, or hard activities that could make the fracture worse. Gradual return to normal activities is advised, based on how the patient feels and their pain level.
For severe vertebral fractures, or if there are neurological symptoms or pain that’s hard to manage, hospitalization might be needed. Close monitoring and more intensive treatment are available in the hospital, which is important for managing complications and supporting recovery.
In summary, treating vertebral fractures at the start involves emergency care, the right medicine, rest, and changing how active you are. Knowing when to go to the hospital is also key for the best results.
Compression fractures can often be treated without surgery. This method helps ease pain, stabilize the spine, and improve function. It’s a non-surgical approach.
Bracing is key in treating compression fractures. Orthotic braces support the spine, helping to stabilize the fracture and reduce pain. The right brace depends on the fracture’s location and severity.
It’s important to fit the brace correctly for it to work well and be comfortable.
Physical therapy is vital in managing compression fractures. A good physical therapy program boosts mobility, strengthens spine muscles, and lessens pain.
Physical therapy includes:
Several home care strategies can help with recovery from compression fractures.
Regular check-ups with a healthcare provider are important to track the fracture’s healing. This may include imaging studies like X-rays or MRI scans to check the fracture’s healing and spine stability.
Based on the patient’s progress, the treatment plan can be adjusted for the best recovery.
Effective medical therapy is key to healing fractured vertebrae and keeping the spine strong. These plans help manage pain right away and support long-term bone health and healing.
Medicines are important for treating vertebral fractures. Bisphosphonates help slow bone loss and lower fracture risk. Teriparatide boosts bone growth and healing. It’s important to take your medicine as directed for the best bone health.
Good nutrition is essential for healing fractured vertebrae. Eating foods high in calcium and vitamin D supports bone health. Dairy, leafy greens, and fortified cereals are good choices. Drinking enough water is also key for health and recovery.
The healing time for vertebral fractures treated without surgery is usually 8 to 12 weeks. Regular check-ups with doctors are needed to track progress and adjust treatment. Patients should also follow activity guidelines to prevent worsening the injury.
Combining the right medical treatments, nutrition, and monitoring helps patients heal well. This approach also lowers the chance of complications.
Treating L1 and lumbar compression fractures involves different methods. These range from non-surgical to surgical options. The choice depends on the fracture’s severity, the patient’s health, and any neurological symptoms.
L1 compression fractures are often treated without surgery. Conservative treatment includes bracing, physical therapy, and changing how you move. But, if these methods don’t work, surgery might be needed.
Fractures at L2, L3, and L5 need careful treatment, similar to L1. Treatment depends on the fracture’s details. For example, serious fractures or those affecting nerves might need surgery.
T12 and T11 fractures are in the thoracic spine but treated like lumbar fractures. They need careful review because of their impact on the spine’s stability.
Compression fractures in the lumbar spine are challenging, mainly for older adults or those with osteoporosis. Risks include more fractures, chronic pain, and mobility loss. Treatment must include medication, nutrition, and physical therapy.
In summary, treating L1 and lumbar compression fractures requires a detailed plan. It considers the fracture’s location, its characteristics, and the patient’s health.
Severe vertebral fractures often need surgery to prevent more problems and help heal. When other treatments don’t work well or keep the fracture stable, surgery is a key option.
Surgery is usually needed for fractures that are unstable, cause a lot of pain, or harm nerves. The choice to have surgery depends on the fracture’s severity, the patient’s health, and any nerve problems.
Key indicators for surgical intervention include:
Vertebral augmentation, like kyphoplasty and vertebroplasty, are less invasive ways to fix the fracture and ease pain. These methods involve putting bone cement into the broken vertebra to make it stable right away.
For complex or unstable fractures, spinal fusion and stabilization are needed. These methods use rods and screws to hold the spine together and help the vertebrae fuse.
Spinal fusion is often chosen for those with serious spinal instability or nerve damage from the fracture.
The recovery time after surgery for severe vertebral fractures varies. It depends on the surgery type and the patient’s health. Most patients need postoperative rehabilitation to get their strength and mobility back.
Recovery expectations include:
Rehabilitation is key after a vertebral fracture. It helps patients regain strength and function. The goal is to get them back to normal activities safely and quickly.
Progressive activity guidelines help patients get back to normal slowly. At first, they should avoid heavy lifting and bending. As they heal, they can do more.
Physical therapy is vital in rehab. It improves flexibility, strength, and posture. Therapists create exercises that fit each patient’s needs, like stretches and core strengthening.
Strengthening the spine muscles is important for recovery. Exercises like pelvic tilts and bridging are used. Always do these exercises with a healthcare professional’s guidance.
The time it takes to get back to normal varies. It depends on the fracture’s severity and the patient’s health. Generally, light activities can start in 6-8 weeks. Full recovery may take several months. Always follow your healthcare provider’s advice.
| Activity Level | Timeline | Examples of Activities |
| Light Activity | 6-8 weeks | Walking, light housekeeping |
| Moderate Activity | 8-12 weeks | Gardening, light lifting |
| Full Activity | Several months | Heavy lifting, strenuous exercise |
It’s key to prevent future fractures to keep your spine healthy, mainly if you’ve had an L1 vertebrae compression fracture. To do this, you need to make lifestyle changes, exercise regularly, and eat right to help your bones.
Managing osteoporosis is also vital to stop more vertebral fractures. Stick to your medication, eat foods high in calcium and vitamin D, and do exercises that make your bones stronger.
Regular visits to your healthcare provider are also important. They help keep an eye on your spine’s health and fix any issues quickly. By following these steps, you can lower your chance of another fracture and keep your spine in top shape.
By focusing on prevention and long-term care, you can live a better life and avoid spinal problems.
A vertebral compression fracture happens when a vertebra collapses. This usually occurs because of osteoporosis or trauma.
Symptoms include back pain and limited mobility. Sometimes, you might feel numbness or tingling in your legs.
Doctors use X-rays, CT scans, or MRI scans to diagnose. These tests help them see how severe the fracture is.
Treatment can be conservative or surgical. Options include bracing, physical therapy, and pain management. Surgery might involve vertebral augmentation or spinal fusion.
Healing usually takes 8-12 weeks with conservative treatment. But, it depends on the fracture’s severity and your health.
Physical therapy improves mobility and strength. It helps in recovery by promoting healing and reducing future fracture risks.
Yes, osteoporosis weakens bones. This makes them more likely to fracture or collapse.
Surgery is needed for severe, unstable fractures or when conservative methods fail. It’s also considered for significant neurological symptoms.
Preventing fractures involves a healthy lifestyle and regular exercise. Managing osteoporosis and reducing fall risks are also key.
Recovery time varies based on surgery type and individual factors. It includes rest, rehabilitation, and a gradual return to activities.
Treatment for these fractures combines conservative and surgical methods. It depends on the fracture’s severity and location.
Lumbar spine fractures are challenging due to the vertebrae’s weight-bearing role. They often require specialized treatment.
While treatments share similarities, the fracture’s location and severity influence the plan. Each case is evaluated individually.
Yao, P. Y. (2023). Varicose vein treatment: Endovenous laser therapy. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK557719/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us