Last Updated on November 18, 2025 by Ugurkan Demir

If you have chronic lower back pain, lumbar fusion surgery might change your life. This surgery permanently connects two or more vertebrae in your lower back. It helps with problems like degenerative disc disease, spondylolisthesis, and spinal stenosis.
At Liv Hospital, we take a detailed approach to lumbar spine fusion surgery. Our patient-centered care and global expertise ensure you get the best treatment. Knowing how a lumbar fusion is done helps you feel more ready for the surgery.
Key Takeaways
- Lumbar fusion surgery is used to treat various lower back conditions.
- The procedure involves permanently joining two or more vertebrae.
- Minimally invasive approaches are increasingly used to reduce recovery time.
- Liv Hospital’s patient-focused protocols ensure complete care.
- Understanding the surgical process is vital for successful outcomes.
Understanding Lumbar Fusion Surgery

To understand lumbar fusion surgery, we need to know about the spine and why it’s needed. We’ll look at what spinal fusion is, the anatomy of the lumbar spine, and why it’s used for lower back issues.
Definition and Purpose of Spinal Fusion
Lumbar vertebral fusion, or bone fusion lower back surgery, joins vertebrae to stabilize the spine. It aims to treat spinal disorders that cause pain and instability in the lower back.
Anatomy of the Lumbar Spine
The lumbar spine, in the lower back, has five vertebrae. They support our body’s weight and help us move. Knowing about this area is key to understanding lumbar fusion surgery.
Conditions Requiring Fusion of the Lower Back
Several conditions may need lumbar fusion surgery. These include degenerative processes and structural abnormalities.
Degenerative Processes
Degenerative disc disease can cause instability and pain in the lumbar spine. As discs wear out, they can’t cushion vertebrae properly. This can lead to pain and inflammation.
Structural Abnormalities
Structural issues, like spondylolisthesis, where a vertebra slips, may also require spinal lumbar fusion. These problems can cause instability and nerve compression. Surgery is needed to stabilize the spine and relieve nerve pressure.
Understanding these conditions and the lumbar spine’s anatomy helps us see the importance of lumbar fusion surgery for lower back issues.
Common Indications for Lumbar Fusion Surgery

Lumbar fusion surgery is often needed for certain lower back problems. These problems don’t get better with regular treatments. We’ll look at the main reasons for this surgery, which include degenerative and traumatic issues in the lumbar spine.
Degenerative Disc Disease
Degenerative disc disease happens when the discs between vertebrae wear out. This causes pain and makes the spine unstable. Lumbar fusion can help stabilize the area and reduce pain.
Spondylolisthesis
Spondylolisthesis is when a vertebra slips out of place. This can press on nerves and cause pain. Fusion surgery aims to put the vertebra back in place and ease nerve pressure.
Spinal Stenosis
Spinal stenosis is when the spinal canal narrows. This can press on nerves and cause a lot of pain. Sometimes, fusion surgery is done with other surgeries to take pressure off nerves.
Trauma to the Lumbar Region
When the lower back is injured, like with a fracture, fusion surgery might be needed. It helps stabilize the spine and aid in healing.
Failed Back Surgery Syndrome
Failed back surgery syndrome is when pain or symptoms don’t go away after surgery. In some cases, fusion surgery is considered to fix the underlying problems.
| Condition | Description | Treatment |
|---|---|---|
| Degenerative Disc Disease | Loss of disc height and integrity | Lumbar Fusion |
| Spondylolisthesis | Vertebra slips out of place | Lumbar Fusion |
| Spinal Stenosis | Narrowing of the spinal canal | Decompression with Fusion |
Preoperative Assessment and Planning
Preparing to fuse the lower back is a detailed process. We start by carefully checking the patient. This helps us decide the best lumbar fusion operation for them.
Patient Evaluation and Selection Criteria
Choosing the right patients for lumbar vertebrae fusion is key. We look at their health, how severe their condition is, and how well they might recover.
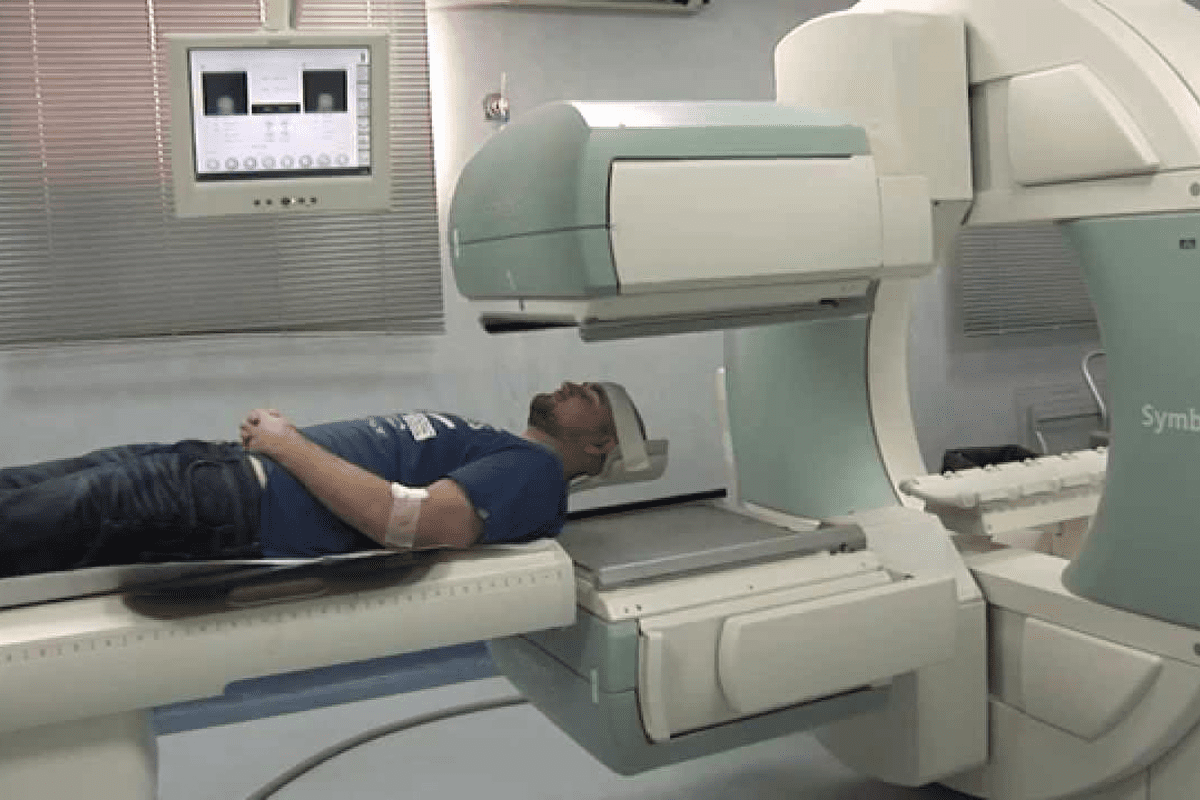
Diagnostic Imaging Techniques
Imaging is vital for planning how is a lumbar fusion done. We use different methods to see the spine clearly.
MRI and CT Scans
MRI and CT scans are important for seeing the spine’s details. They help us spot any issues and plan the surgery.
Flexion-Extension X-rays
Flexion-extension X-rays show how stable the spine is. They help us understand how much the affected area moves.
Surgical Approach Selection
Choosing the right surgery method is essential for fusing lower back success. We consider the patient’s body and the surgeon’s skills.
Patient Preparation Protocol
Getting the patient ready for surgery involves several steps. We educate them, manage their hopes, and make sure they’re physically prepared.
Techniques in Lumbar Spine Fusion Surgery
Lumbar spine fusion surgery uses different techniques to treat spinal problems. The choice of method depends on the patient’s condition, the surgeon’s skills, and the procedure’s needs.
Posterolateral Lumbar Fusion (PLF)
Posterolateral Lumbar Fusion (PLF) is a common method. It fuses the transverse processes in the lumbar spine. This technique is often used for spondylolisthesis and degenerative disc disease. PLF provides stability to the affected segment.
Posterior Lumbar Interbody Fusion (PLIF)
Posterior Lumbar Interbody Fusion (PLIF) removes the disc and inserts a graft or cage from the back. It allows for direct decompression of neural elements and restores disc height. PLIF is good for spinal stenosis and spondylolisthesis.
Transforaminal Lumbar Interbody Fusion (TLIF)
Transforaminal Lumbar Interbody Fusion (TLIF) is similar to PLIF but has a more lateral approach. This reduces the risk of nerve damage. TLIF is great for restoring lordosis and providing full fusion. It’s good for patients with significant disc collapse or foraminal stenosis.
Anterior Lumbar Interbody Fusion (ALIF)
Anterior Lumbar Interbody Fusion (ALIF) accesses the spine from the front to remove the disc and insert a graft or cage. ALIF is best for L5-S1 level conditions. The anterior approach helps restore lordosis and disc height.
Minimally Invasive Approaches
Minimally invasive lumbar fusion is popular for less tissue damage and faster recovery. These methods use small incisions and special tools. They can be used for PLIF and TLIF.
Benefits and Limitations
Minimally invasive fusion has many benefits, like less blood loss and pain, and quicker healing. But, it also has challenges, like a steep learning curve for surgeons and visualization issues.
Patient Selection
Choosing the right patient for minimally invasive fusion is key. The patient’s health, the spinal condition’s complexity, and the surgeon’s experience are important factors.
Step-by-Step Lumbar Fusion Procedure
We will walk you through the steps of lumbar fusion surgery. This surgery is complex and has many stages. Each stage is important for a successful fusion of the lower spine.
Anesthesia Administration and Patient Positioning
The first step is giving anesthesia to keep the patient comfortable. We then position the patient on the table for the best access to the spine.
Surgical Approach and Exposure
Next, we make a precise incision to expose the lumbar vertebrae. The approach depends on the condition and the patient’s body.
Decompression and Disc Removal Process
We then relieve pressure on nerves and remove damaged discs. This step is to ease pain and protect the nerves.
Neural Element Protection
Protecting the nerves is key during this part. We use special techniques and tools to keep them safe.
Endplate Preparation
After removing the disc, we prepare the endplates for fusion. This means cleaning and getting ready for the bone graft.
Bone Graft Placement Techniques
Placing the bone graft is a critical step. We use different methods to ensure the graft contacts the vertebrae well for fusion.
| Bone Graft Type | Description | Advantages |
|---|---|---|
| Autograft | Harvested from the patient’s own body | High fusion rate, no risk of rejection |
| Allograft | Obtained from a donor | Availability, reduced morbidity |
| Synthetic | Man-made materials | Unlimited availability, customizable |
Instrumentation Installation
We use tools like pedicle screws and rods to stabilize the spine. We carefully place these to ensure the spine is aligned and stable.
Pedicle Screw Placement
Placing pedicle screws needs precision. We use advanced imaging to guide this process.
Rod and Cage Insertion
After screws, we insert rods and cages for more stability. These support the fusion process.
Intraoperative Imaging Guidance
We use imaging during the surgery to check our work. This helps us make any needed adjustments.
Wound Closure Methods
At the end, we close the wound. We use layered closure to help healing and prevent complications.
By following this guide, we ensure a successful lumbar fusion. This surgery helps alleviate pain and improves the patient’s life quality.
Fusion of Spine in Lumbosacral Region: Special Considerations
When surgeons fuse the spine in the lumbosacral region, they face unique challenges. This area, where the lumbar spine meets the sacrum, has special anatomical and biomechanical needs.
L5-S1 Junction Challenges
The L5-S1 junction is a key area for surgeons to focus on. It’s under a lot of stress and motion, making it prone to problems like pseudarthrosis or instrumentation failure. Careful planning and execution are essential to overcome these challenges.
Sacropelvic Fixation Techniques
Sacropelvic fixation is vital in lower back surgery fusion, more so when dealing with multiple levels. Techniques like iliac screw fixation or S2-alar-iliac (S2AI) screws help stabilize the area.
Lumbosacral Biomechanics
Understanding the biomechanics of the lumbosacral junction is key to successful fusion. This area is subject to forces like flexion, extension, and rotation. We must consider these forces when planning and executing the fusion to achieve the best results.
Adjacent Segment Considerations
Adjacent segment disease is a risk after lumbar vertebral fusion. We must think about how fusion affects adjacent segments and take steps to reduce the risk of future problems. This includes choosing the right patients, using precise surgical techniques, and providing thorough postoperative care.
| Consideration | Description | Importance |
|---|---|---|
| L5-S1 Junction Challenges | Addressing stress and motion at the L5-S1 junction | High |
| Sacropelvic Fixation Techniques | Providing stable fixation across the lumbosacral junction | High |
| Lumbosacral Biomechanics | Understanding complex forces at the lumbosacral junction | High |
| Adjacent Segment Considerations | Minimizing the risk of adjacent segment disease | Medium |
Bone Fusion in Lower Back Surgery: Materials and Methods
Bone fusion in lumbar spine surgery uses different materials and methods. Each has its own benefits and things to consider. We’ll look into these to see how they help in successful lower back surgery.
Autografts vs. Allografts
Autografts come from the patient’s own body. They are the top choice because they help bone growth well. Allografts, from donors, are an option that doesn’t need another surgery site. We’ll talk about the good and bad of each.
| Characteristics | Autografts | Allografts |
|---|---|---|
| Osteoinductive Properties | High | Variable |
| Donor Site Morbidity | Present | Absent |
| Availability | Limited | Abundant |
Synthetic Bone Graft Substitutes
Synthetic grafts are made to act like natural bone. They are a new option. We’ll talk about what they’re made of and how well they work.
Bone Morphogenetic Proteins (BMPs)
BMPs are proteins that help bones grow. They make bone fusion better. Their use in lumbar spine fusion is very promising.
Fusion Enhancement Technologies
Technologies like electrical stimulation and ultrasound therapy help bone fusion. We’ll look at how they help make surgery successful.
Electrical Stimulation
Electrical stimulation helps bones grow by boosting healing.
Ultrasound Therapy
Low-intensity ultrasound therapy helps bones repair and grow. It supports the fusion process.
In conclusion, choosing the right materials and methods for bone fusion in lower back surgery is key. Knowing our options helps us tailor treatments for each patient.
Postoperative Care and Complications of Lumbar Vertebral Fusion
After lumbar vertebral fusion surgery, it’s key to care for patients well. This helps avoid problems and helps them heal. We know the recovery time can be tough, so we aim to give the best care possible.
Immediate Postoperative Management
Right after surgery, we watch patients closely for any issues. We also make sure they’re not in too much pain before they go home.
Pain Control Strategies
We focus a lot on managing pain. We use different medicines and methods to keep pain down. This helps patients move around sooner and feel better.
Mobilization Protocol
Moving around early is important. It helps prevent blood clots and speeds up healing. Our physical therapists help create a plan for each patient.
Potential Complications
Lumbar fusion surgery is usually safe, but some problems can happen. These include:
Hardware Failure
When the hardware used in surgery fails, it can cause instability. Sometimes, more surgery is needed.
Pseudarthrosis
Pseudarthrosis is when the bone doesn’t fuse right. This can cause ongoing pain and instability.
Adjacent Segment Disease
Changes can happen in the nearby segments. This can cause new pain and symptoms.
Infection Management
Infections are serious and need quick treatment. This often means antibiotics and sometimes more surgery.
| Complication | Description | Management |
|---|---|---|
| Hardware Failure | Failure of surgical hardware | Revision surgery |
| Pseudarthrosis | Failure of bone fusion | Revision surgery, bone grafting |
| Adjacent Segment Disease | Degeneration of adjacent segments | Conservative management, potentially additional surgery |
Monitoring Fusion Progress
We keep an eye on how the bone fusion is doing. We do this with regular check-ups and scans. This helps us catch any problems early and fix them.
We aim to give the best care after lumbar vertebral fusion. Our team is dedicated to helping patients get better during their recovery.
Recovery and Rehabilitation After Lower Spine Fusion
Lower spine fusion surgery is just the start. A good recovery and rehab plan is key for lasting success. We help patients through this important time, focusing on what makes recovery successful.
Expected Timeline for Recovery
The time it takes to recover from lower lumbar fusion surgery varies. Most people see big improvements in 6 to 12 months.
Physical Therapy Protocols
Physical therapy is vital after fusing the lower back. It helps patients get stronger, more flexible, and mobile.
Core Strengthening
Core exercises are key in physical therapy. They help support the spine and improve stability.
Gait Training
Gait training helps patients walk normally again. It also lowers the chance of future problems.
Activity Restrictions and Progression
After lumber fusion surgery, patients must follow certain activity rules. They will slowly start doing more activities with their doctor’s help.
Return to Work and Daily Activities
When to go back to work and daily activities depends on the job and health.
Long-term Outcomes and Follow-up
Most people see great results from fusing lower back surgery. They feel less pain and live better lives. Regular check-ups are important to keep track of progress and solve any issues.
Conclusion
Lumbar fusion surgery is a complex procedure. It needs careful planning, precise technique, and detailed postoperative care. This surgery is key for treating spinal issues like degenerative disc disease and spinal stenosis.
The success of this surgery depends on many factors. These include choosing the right patient, using advanced imaging, and picking the best surgical method. Different techniques are used, depending on the patient’s condition and body.
In this surgery, bone grafts are used to help the spine fuse. These can be from the patient themselves, from another person, or synthetic. Installing instruments is also important. It helps keep the spine stable while it heals.
After the surgery, caring for the patient is critical. This includes managing pain, helping them move, and watching for any complications. Knowing how lumbar fusion surgery works helps us improve care and relieve spinal pain.
FAQ
What is lumbar fusion surgery?
Lumbar fusion surgery is a procedure where we fuse two or more vertebrae in the lower back together. This helps stabilize the spine and relieve pain caused by various spinal conditions.
What conditions require lumbar fusion surgery?
We perform lumbar fusion surgery for conditions like degenerative disc disease, spondylolisthesis, and spinal stenosis. It’s also used for trauma to the lumbar region.
How is a lumbar fusion done?
The surgery includes several steps. First, we administer anesthesia and position the patient. Then, we make an approach and expose the area.
References
- Spine-health : https://www.spine-health.com/video/lumbar-spinal-fusion-surgery-animation
- AAOS (American Academy of Orthopaedic Surgeons) : https://www.aaos.org/en/treatment/spinal-fusion
- NT Neurosurgery : https://ntneurosurgery.com/2023/11/22/what-is-a-three-lumbar-fusion
- Journal of Spine Surgery (JSS) : https://jss.amegroups.org/article/view/6198/html
- Neurosurgical Associates PC : https://neurosurgicalassociatespc.com/posterolateral-lumbar-fusion