Last Updated on November 20, 2025 by Ugurkan Demir

Aplastic anemia is a serious condition where the bone marrow fails to produce blood cells. This disorder can significantly impact a patient’s quality of life, making timely and effective treatment very important.
We know that aplastic anemia treatment depends on many factors. These include the severity of symptoms, the patient’s age, and their overall health. At Liv Hospital, we offer personalized care how to treat aplastic anemia. We use evidence-based pathways and advanced medical treatment options tailored to each patient’s needs.
Our team is dedicated to delivering world-class healthcare. We provide complete support for international patients. By choosing the right medical and therapeutic approach, we can greatly improve treatment outcomes.
Key Takeaways
- Personalized treatment plans are key for effective aplastic anemia management.
- Treatment options vary based on patient-specific factors, including age and overall health.
- Advanced medical treatments and therapeutic approaches can significantly improve outcomes.
- Liv Hospital offers internationally focused care with evidence-based treatment pathways.
- Comprehensive support services are available for international patients.
Understanding Aplastic Anemia
Aplastic anemia is a serious condition where the bone marrow can’t make enough blood cells. This leads to health problems that can really affect a person’s life. It’s important to know what causes it and how it works.
Definition and Pathophysiology
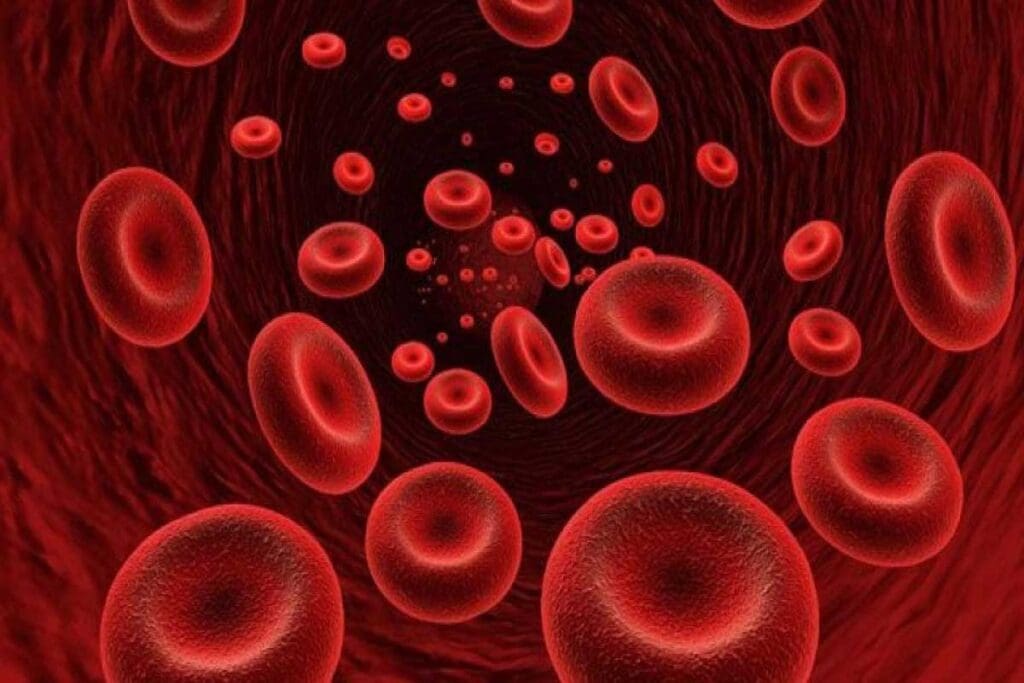
Aplastic anemia happens when the bone marrow can’t make blood cells. This includes red blood cells, white blood cells, and platelets. Without these cells, people can get anemia, catch infections easily, and have bleeding problems.
The bone marrow’s stem cells, which make blood cells, get destroyed or don’t work properly. This is what leads to aplastic anemia.
Without treatment, severe aplastic anemia can be deadly. Up to 70 percent of people with it die within two years. This shows how critical it is to find and use effective treatments quickly.
Causes and Risk Factors
There are many reasons why someone might get aplastic anemia. It can be caused by toxins, chemicals, autoimmune diseases, or viruses. Some cases are linked to genetic problems or radiation.
Some key things that increase the risk include:
- Being exposed to harmful chemicals or pesticides
- Having had radiation or chemotherapy before
- Catching certain viruses like hepatitis or HIV
- Having an autoimmune disease
- Having a genetic condition like Fanconi anemia
Knowing what causes aplastic anemia helps doctors diagnose and treat it better.
Recognizing the Signs and Symptoms
Knowing the signs of aplastic anemia is key to managing it well. This condition often shows up with symptoms that are not specific. We will cover the common signs that might point to aplastic anemia.
Common Clinical Manifestations
The symptoms of aplastic anemia can be different for everyone. They can affect many parts of a person’s health. Here are some common symptoms:
- Persistent fatigue and weakness due to anemia
- Shortness of breath, even at rest or during minimal physical activity
- Frequent infections resulting from a compromised immune system
- Unexplained bruising or bleeding, which can be a sign of low platelet count
- Pale skin, a result of reduced red blood cell production
These symptoms happen because aplastic anemia stops the bone marrow from making blood cells. This can lead to many complications that affect a person’s quality.
When to Seek Medical Attention
If you or someone you know has any of these symptoms, it’s important to see a doctor:
- Severe fatigue that interferes with daily activities
- Recurring infections that do not respond to treatment
- Unexplained bleeding or bruising
- Shortness of breath or chest pain
Getting a diagnosis and treatment early can greatly help patients with aplastic anemia. If you’re experiencing these symptoms, see a doctor right away.
| Symptom | Possible Cause | Action |
| Fatigue | Anemia | Consult a doctor if persistent |
| Frequent Infections | Low white blood cell count | Seek medical attention if recurring |
| Unexplained Bruising | Low platelet count | Visit a healthcare provider |
“Early recognition of aplastic anemia symptoms is vital for effective treatment and improved patient outcomes.”
— Medical Expert
By knowing the signs and symptoms of aplastic anemia, patients can get help early. This can improve their chances of a better outcome and a better life.
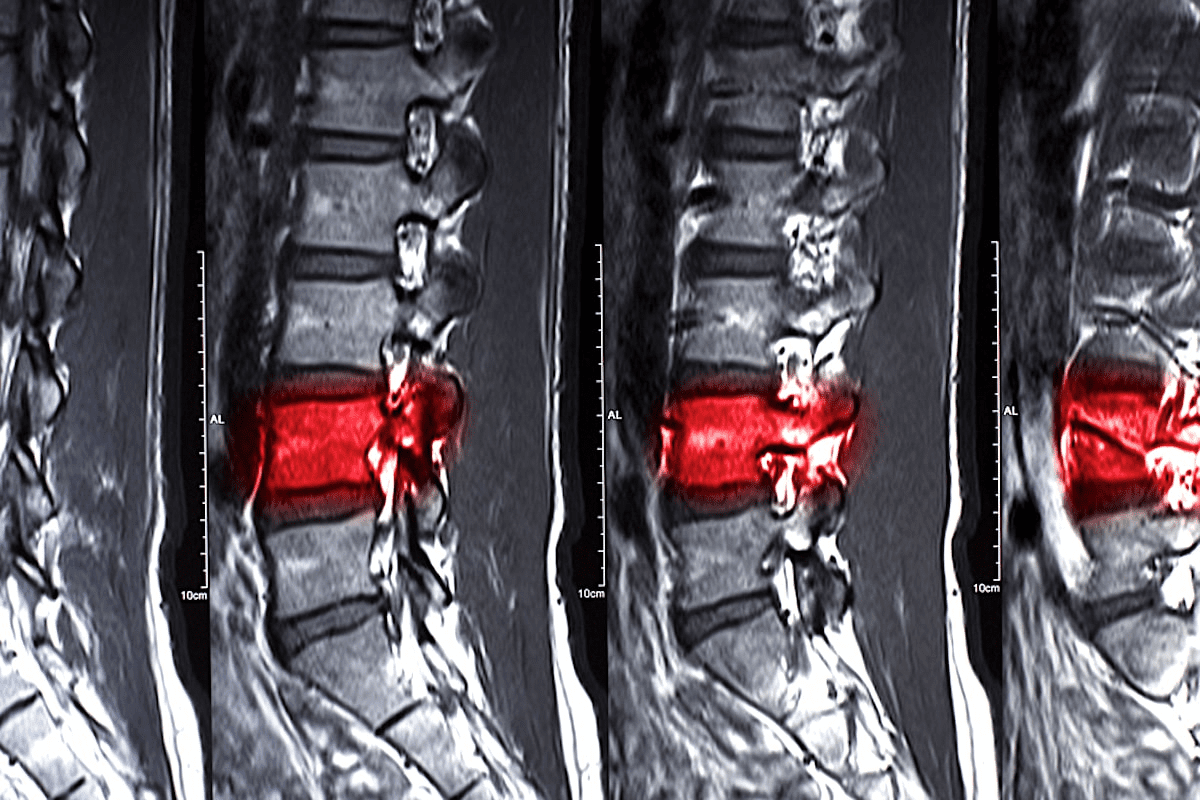
Diagnostic Approach for Aplastic Anemia
To diagnose aplastic anemia, doctors use blood tests and bone marrow biopsies. They follow a detailed process. This helps confirm bone marrow failure and rule out other possible causes of symptoms.
Blood Tests and Complete Blood Count
The first step is blood tests, including a Complete Blood Count (CBC). The CBC checks the levels of red, white blood cells and platelets. In aplastic anemia, all counts are usually low.
More tests might be done to check the bone marrow’s function. These include a reticulocyte count and other tests to see how well the bone marrow works.
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy is key to diagnosing aplastic anemia. It takes a small sample from the hipbone for examination. This helps confirm aplastic anemia by looking at the bone marrow’s cell structure.
Bone marrow aspiration is done at the same time. It takes a liquid sample for analysis. These tests together help see if the bone marrow can make blood cells and find the cause of aplastic anemia.
Ruling Out Other Conditions
Doctors also check for other conditions that might cause similar symptoms. This includes myelodysplastic syndromes, leukemia, and other bone marrow issues. They use the tests mentioned earlier and others as needed.
By looking at the test results, doctors can accurately diagnose aplastic anemia. Then, they can create a treatment plan that fits the patient’s needs.
Classification and Severity Assessment
It’s key to understand the classification and severity of aplastic anemia for good management. The severity of this condition greatly affects treatment and outcomes.
Mild, Moderate, and Severe Aplastic Anemia
Aplastic anemia is divided into three levels: mild, moderate, and severe. These levels are based on blood cell counts and bone marrow function. Severe aplastic anemia shows a big drop in blood cell production. This leads to severely low counts of neutrophils, platelets, and red blood cells.
The National Institutes of Health has guidelines for diagnosing and assessing aplastic anemia. They stress the need for blood tests and bone marrow biopsies.
| Severity | Blood Cell Counts | Bone Marrow Function |
| Mild | Near-normal counts | Moderately reduced |
| Moderate | Reduced counts | Significantly reduced |
| Severe | Very low counts | Severely reduced |
Prognostic Indicators and Mortality Risk
Prognostic indicators are vital in determining the risk of death from aplastic anemia. Age, how severe the blood cell drops are, and how well the first treatment works are key.
“The prognosis for patients with aplastic anemia varies significantly based on the severity of the disease and the patient’s response to treatment.”
Those with severe aplastic anemia face a higher risk of death, mainly from infections and bleeding. Knowing the prognostic indicators helps doctors plan better treatments to improve patient outcomes.
We use clinical checks and diagnostic tests to figure out the severity and what the future might hold for aplastic anemia. This helps us make the right treatment choices.
Initial Treatment Decisions and Considerations
When treating aplastic anemia, the first steps are key to success. Treatment decisions for aplastic anemia depend on many things. These include the patient’s age, health, and whether a good donor is available.
Age-based treatment approaches are vital in treating aplastic anemia well. Younger patients might get more aggressive treatments like stem cell transplants. Older patients might do better with immunosuppressive therapy, which is safer.
Age-Based Treatment Approaches
The patient’s age is a big factor in choosing treatment. Younger patients, under 40, might get stem cell transplants. This could cure them. Older patients or those with health issues might get immunosuppressive therapy instead. This is safer but less likely to cure.
Donor Availability Assessment
Finding a good donor is key to stem cell transplants. We look for a matched donor, like a sibling or an unrelated one. If a donor is found, a transplant becomes a strong option for a cure.
Patient-Specific Factors
Other things matter too, like the patient’s health and how severe their aplastic anemia is. We use these to make a treatment plan that works for them. This way, the treatment is both effective and easy to handle.
In short, starting treatment for aplastic anemia means looking at many things. We consider the patient’s condition, age, and whether a donor is available. This helps us create a treatment plan that gives the patient the best chance to get better.
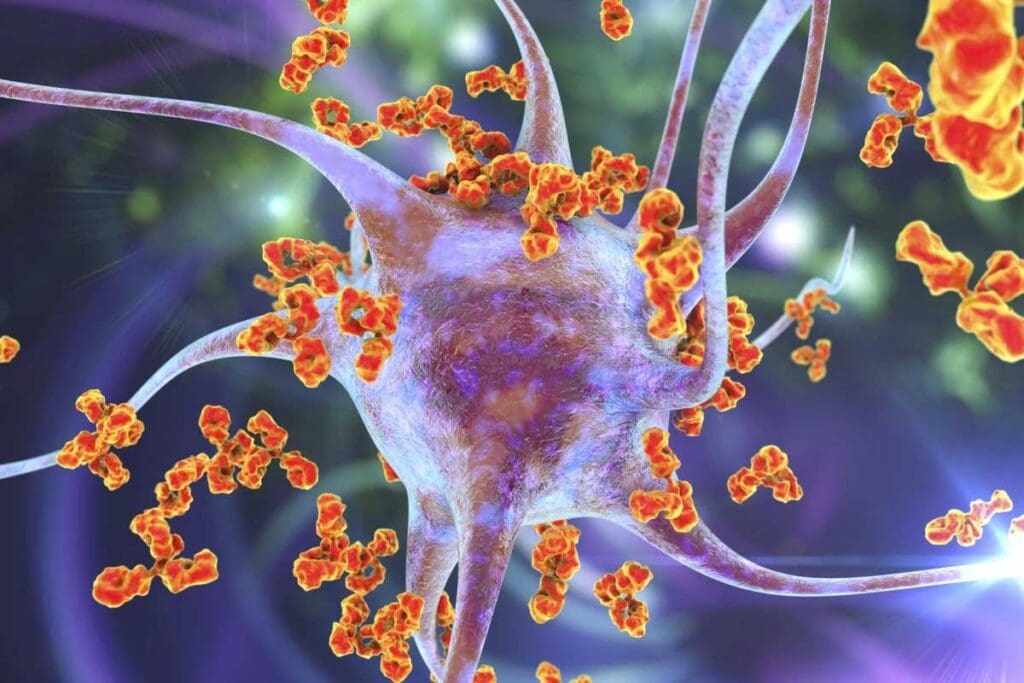
How to Treat Aplastic Anemia with Immunosuppressive Therapy
Immunosuppressive therapy is key for treating aplastic anemia in patients not fit for bone marrow transplants. It helps by reducing the immune system’s attack on the bone marrow. This makes it easier for blood cell production to recover.
Anti-Thymocyte Globulin (ATG) Protocol
Anti-Thymocyte Globulin (ATG) is a vital part of treatment for aplastic anemia. ATG depletes T-cells, which are immune cells that can harm the bone marrow. It’s given intravenously over several days, often with other drugs.
Patients’ responses to ATG vary, with some seeing big improvements in blood counts. It’s important to watch for side effects like serum sickness during treatment.
Cyclosporine Administration
Cyclosporine is another important drug in treating aplastic anemia. It stops T-cell activation, reducing the immune system’s attack on the bone marrow. It’s taken orally, and the dose is adjusted based on how the patient responds.
Using ATG and cyclosporine together can help more patients. It’s important to keep an eye on cyclosporine levels to avoid side effects.
Eltrombopag and Other Agents
Eltrombopag is a drug that helps with platelet recovery in aplastic anemia patients. Adding it to treatment has been shown to improve results.
| Treatment Component | Mechanism of Action | Administration |
| Anti-Thymocyte Globulin (ATG) | Depletes T-cells | Intravenous |
| Cyclosporine | Inhibits T-cell activation | Oral |
| Eltrombopag | Stimulates platelet production | Oral |
Immunosuppressive therapy is a vital treatment for aplastic anemia, giving hope to those not suited for transplants. Understanding ATG, cyclosporine, and eltrombopag helps doctors create personalized treatment plans.
Allogeneic Stem Cell Transplantation Procedure
Allogeneic stem cell transplantation is a key treatment for aplastic anemia, mainly for young patients with a matched sibling donor. It replaces the patient’s sick bone marrow with healthy stem cells from a donor. This could be a cure for the condition.
Matched Sibling Donor Transplantation
For those with a matched sibling donor, this transplant is often the top choice. First, the donor is thoroughly checked for compatibility and health. Then, the patient gets conditioning therapy to clear out the bad bone marrow. After that, the donor’s stem cells are infused into the patient.
Benefits of matched sibling donor transplantation include a lower risk of graft-versus-host disease (GVHD). This could lead to better results and fewer complications.
Matched Unrelated Donor Options
If a matched sibling donor isn’t available, a matched unrelated donor (MUD) can be an option. Thanks to better HLA typing, finding a suitable MUD is easier. This means more patients can find a donor.
Using MUDs has gotten safer with better immunosuppressive treatments. This reduces GVHD risk and boosts transplant success chances.
Haploidentical Transplantation
Haploidentical transplantation uses a donor who is half-matched, usually a family member. It’s becoming more popular because it’s available to more people.
Advances in haploidentical transplantation techniques have made it safer and more effective. The addition of post-transplant cyclophosphamide helps prevent GVHD. This makes the transplant safer and more successful.
Supportive Care Measures
Treating aplastic anemia goes beyond just treatments. It also includes supportive care to keep patients stable and prevent complications. We will explore the key supportive care measures for managing aplastic anemia.
Blood Transfusion Protocols
Blood transfusions are vital for supportive care. They help reduce symptoms like fatigue and shortness of breath by boosting red blood cells. Platelet transfusions are also important to prevent or treat bleeding.
- Red Blood Cell Transfusions: Used to manage anemia and improve oxygen delivery to tissues.
- Platelet Transfusions: Administered to prevent or treat bleeding due to thrombocytopenia.
We watch patients closely for any issues with transfusions and adjust protocols as needed.
Infection Prevention and Management
Preventing infections is a major part of supportive care. Patients with aplastic anemia are more at risk of infections because of low neutrophil counts.
- Prophylactic Antibiotics: May be prescribed to prevent infections in high-risk patients.
- Neutropenia Management: Involves careful monitoring and sometimes the use of granulocyte-colony stimulating factor (G-CSF) to boost neutrophil counts.
Bleeding Prevention Strategies
Preventing bleeding is critical, mainly for those with low platelet counts. Strategies include:
- Platelet Transfusions: To maintain platelet counts above a certain threshold.
- Avoiding Trauma: Patients are advised to avoid activities that could lead to injury or bleeding.
- Medications: Certain medications that can increase the risk of bleeding are avoided or used with caution.
Nutritional Support
Nutritional support is key to ensuring patients get enough calories, proteins, and nutrients. A balanced diet is essential for managing the disease and aiding in recovery.
We collaborate with nutritionists to offer personalized dietary advice and support.
Treatment Pathways Based on Patient Profiles
Effective treatment of aplastic anemia depends on the patient’s profile. The treatment strategy changes based on age, health, and donor availability.
Young Patients with Matched Sibling Donors
Young patients with a matched sibling donor often get allogeneic stem cell transplantation first. This method can cure the disease by replacing the bone marrow with healthy stem cells.
Patients Without Suitable Donors
When no suitable donor is found, immunosuppressive therapy is used. This treatment helps by suppressing the immune system to recovery of bone marrow function.
Elderly or Frail Patients
Elderly or frail patients get more conservative treatment. They focus on supportive care measures like blood transfusions and preventing infections. Immunosuppressive therapy is also considered, based on the patient’s health and treatment tolerance.
Refractory or Relapsed Cases
When initial treatment fails or the disease comes back, new options are needed. This might include experimental therapies or joining clinical trials for new treatments.
Customizing treatment based on the patient’s profile helps healthcare providers achieve better results in managing aplastic anemia.
Monitoring Treatment Response
Monitoring how well treatment works is key in managing aplastic anemia. It helps doctors make sure patients get the best care. Regular checks help see if the treatment is working and if changes are needed.
Blood Count Recovery Assessment
How well blood counts recover is a big sign of treatment success. Regular blood tests track red, white blood cells, and platelets. If these counts go up, it means treatment is working.
We watch for changes in blood counts over time. This shows if the bone marrow is healing. We keep a close eye on complete blood count (CBC) results.
Bone Marrow Evaluation Timeline
Bone marrow health is also important for checking treatment success. Bone marrow biopsies check the marrow’s health and cell count.
These tests are done at the start of treatment and later, based on how the patient is doing. The timing can change, but it’s usually at the start, after a few months, and as needed.
Signs of Treatment Failure
Some patients may not get better or may get worse despite treatment. Signs of treatment failure include not getting better, blood counts staying low, and serious side effects.
We watch for these signs and change the treatment plan if needed. Finding out early if treatment isn’t working is important for trying new options.
Criteria for Treatment Adjustment
Deciding to change treatment depends on several things. These include how well the patient is doing, side effects, and new treatments. Criteria for adjustment include not getting better, bad side effects, and new treatments available.
We think about these things when considering a treatment change. Our goal is to give the best care with the least side effects.
Emerging Therapies and Clinical Trials
New treatments and ongoing studies offer hope for aplastic anemia patients. Research is moving forward, bringing new ways to help patients. These new strategies aim to make treatments better and more effective.
Novel Immunosuppressive Approaches
New ways to fight the immune system are being tested. Anti-thymocyte globulin (ATG) and cyclosporine are key, but new options are coming. For example, eltrombopag might help boost bone marrow and blood counts.
Gene Therapy Prospects
Gene therapy is a new area in treating aplastic anemia. It could fix the genetic problems causing the disease. Though it’s early, gene therapy might offer a lasting solution for some.
Participation in Clinical Trials
Joining clinical trials is key to improving aplastic anemia treatment. These studies offer new treatments and help researchers. We urge patients to look into clinical trials as part of their care.
Updated Therapeutic Protocols
New findings are changing how we treat aplastic anemia. Regular checks help adjust treatments for better results. Keeping up with the latest guidelines is vital for patient care.
Conclusion: Long-Term Outlook and Quality of Life
Modern treatments have greatly improved the outlook for aplastic anemia patients. The survival rate has gone up, thanks to treatments like bone marrow transplants from siblings.
Good treatment plans can really boost a patient’s quality of life. Doctors can now offer care that meets both physical and emotional needs. This makes a big difference for patients.
The success of treatment directly affects a patient’s quality of life. Those who get better can live long, active lives. It’s important to keep an eye on them and provide support to avoid problems.
As research keeps moving forward, we’ll see even better treatments for aplastic anemia. This could lead to even better lives for those affected by this disease.
FAQ
What is aplastic anemia, and how is it diagnosed?
Aplastic anemia is a rare condition where the bone marrow doesn’t make enough blood cells. Doctors use blood tests and a bone marrow biopsy to diagnose it. This helps figure out if it’s aplastic anemia or something else.
What are the causes and risk factors for developing aplastic anemia?
It can happen due to autoimmune issues, toxins, certain meds, or viruses. Being exposed to chemicals or having a family history also raises the risk.
How is the severity of aplastic anemia classified, and what are the prognostic indicators?
It’s divided into mild, moderate, and severe types. The patient’s age and how well they respond to treatment are key. These factors affect how likely they are to survive.
What are the treatment options for aplastic anemia, and how are they determined?
Treatments include immunosuppressive therapy and stem cell transplants. The choice depends on the patient’s age, how severe it is, and if there’s a donor.
What is immunosuppressive therapy, and how is it used to treat aplastic anemia?
It uses meds like ATG, cyclosporine, and eltrombopag. These help calm the immune system so the bone marrow can start making blood cells again.
What is allogeneic stem cell transplantation, and when is it considered?
It’s when new stem cells replace the old ones. It’s for severe cases, mainly when a suitable donor is found.
What supportive care measures are important for managing aplastic anemia?
Care includes blood transfusions and preventing infections. It also includes stopping bleeding and keeping the patient well-nourished to improve their health and quality.
How is treatment response monitored in patients with aplastic anemia?
Doctors check blood counts and bone marrow regularly. They watch for signs that treatment isn’t working. Treatment plans are adjusted as needed.
What emerging therapies and clinical trials are available for aplastic anemia?
New treatments include immunosuppressants and gene therapy. Clinical trials offer access to these new treatments, helping improve care for aplastic anemia.
What is the long-term outlook for patients with aplastic anemia, and how can they improve their quality of life?
With the right treatment, survival rates have improved a lot. Patients can live better by sticking to their treatment, getting regular check-ups, and making healthy choices.
How does acquired aplastic anemia differ from other forms of the condition?
Acquired aplastic anemia is the most common type. It’s not passed down and is caused by things like toxins or meds. It’s different from congenital forms that are present at birth.
What is the role of ATG in treating aplastic anemia?
ATG is a key part of treatment. It helps calm the immune system’s attack on the bone marrow.
Can aplastic anemia be cured, and what are the chances of relapse?
Some patients can be cured, mainly with stem cell transplants. But there’s a chance of relapse, so ongoing care is needed.
References
- Bacigalupo, A. (2025). Aplastic anemia. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK534212/