Last Updated on November 27, 2025 by Bilal Hasdemir
Nearly 600,000 women in the United States undergo a hysterectomy each year, making it one of the most common surgeries. However, many women remain unaware of the hysterectomy side effects that can appear in the long term.
Understanding these hysterectomy side effects is essential before making a decision. It’s important to know both the benefits and potential long-term health impacts of the procedure. This knowledge empowers women to make informed choices about their reproductive and overall well-being.
Key Takeaways
- Understanding what a hysterectomy is and its implications.
- The importance of being informed about the procedure.
- Potential long-term health consequences of uterus removal.
- Factors to consider before undergoing a hysterectomy.
- The role of a hysterectomy in women’s reproductive health.
Understanding Hysterectomy: More Than Just Uterus Removal
A hysterectomy is more than uterus removal; it’s a surgery with a long medical history. It has big effects on a woman’s health, beyond just removing an organ.
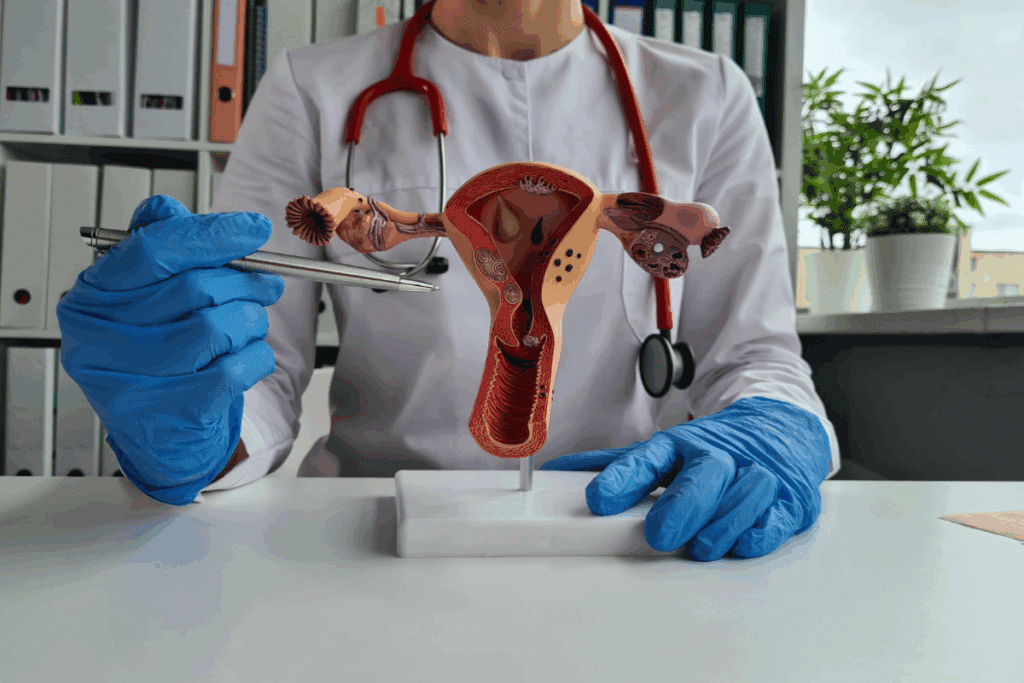
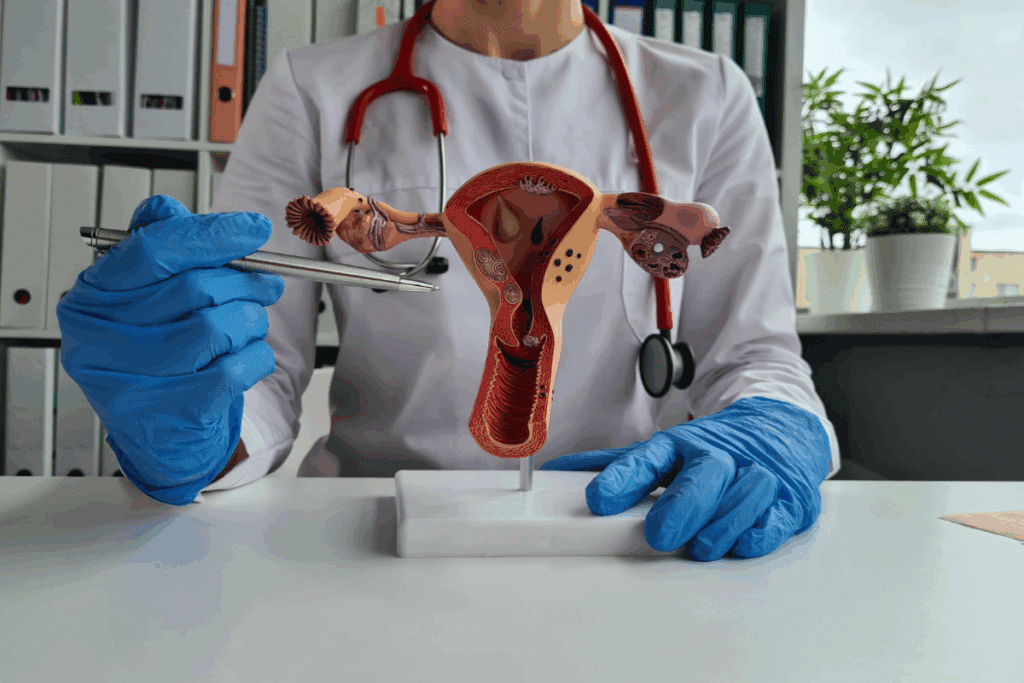
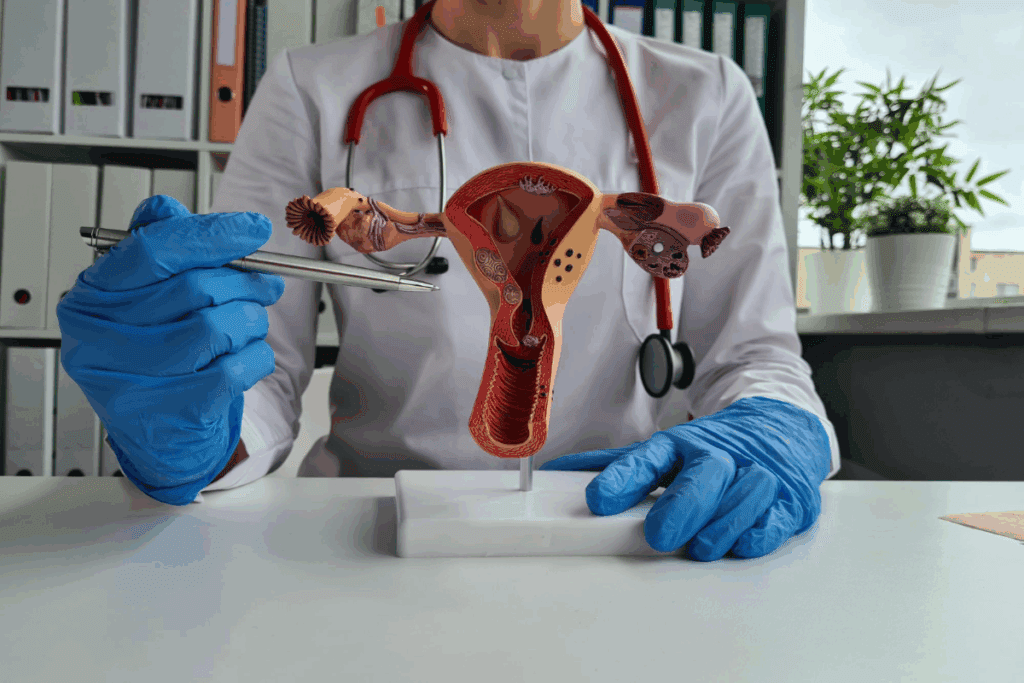
Definition and Basic Procedure
A hysterectomy is when a woman’s uterus is surgically removed. The surgeon might also take out the cervix, ovaries, or fallopian tubes. This depends on the reason for the surgery and the type of hysterectomy.
The surgeon makes an incision in the belly or goes through the vagina. The goal is to remove the uterus and sometimes other organs.
The decision to remove additional organs depends on the patient’s health, the surgery’s reason, and what the patient wants.
Historical Context and Evolution of the Procedure
The first hysterectomy was done in the late 19th century. Over time, the surgery has changed a lot. It’s now done with better techniques, anesthesia, and care after surgery.
At first, hysterectomies were only for life-threatening issues. Now, they’re also done to improve a woman’s quality of life. This includes treating severe endometriosis or uterine fibroids.
The Prevalence of Hysterectomies in the United States
Hysterectomies are very common in the U.S. Health statistics show hundreds of thousands of women have this surgery every year. This is because of conditions like uterine fibroids, endometriosis, and some cancers.
Knowing why hysterectomies are common helps women make better choices about their reproductive health.
Types of Hysterectomy Procedures Explained
Understanding the different types of hysterectomy procedures is key to making a well-informed decision. A hysterectomy is a big surgery done for many medical reasons. The type of surgery you need depends on your health, the reason for the surgery, and what you prefer.
Partial Hysterectomy vs. Total Hysterectomy
A partial hysterectomy removes the uterus but keeps the cervix. This is often chosen when the problem is only in the uterus. A total hysterectomy removes both the uterus and cervix. The choice depends on your health and the reason for the surgery.
It’s important to know the differences to make the right choice for you. A partial hysterectomy might be right for some, but a total hysterectomy is needed for others, like cancer or severe cervical disease.
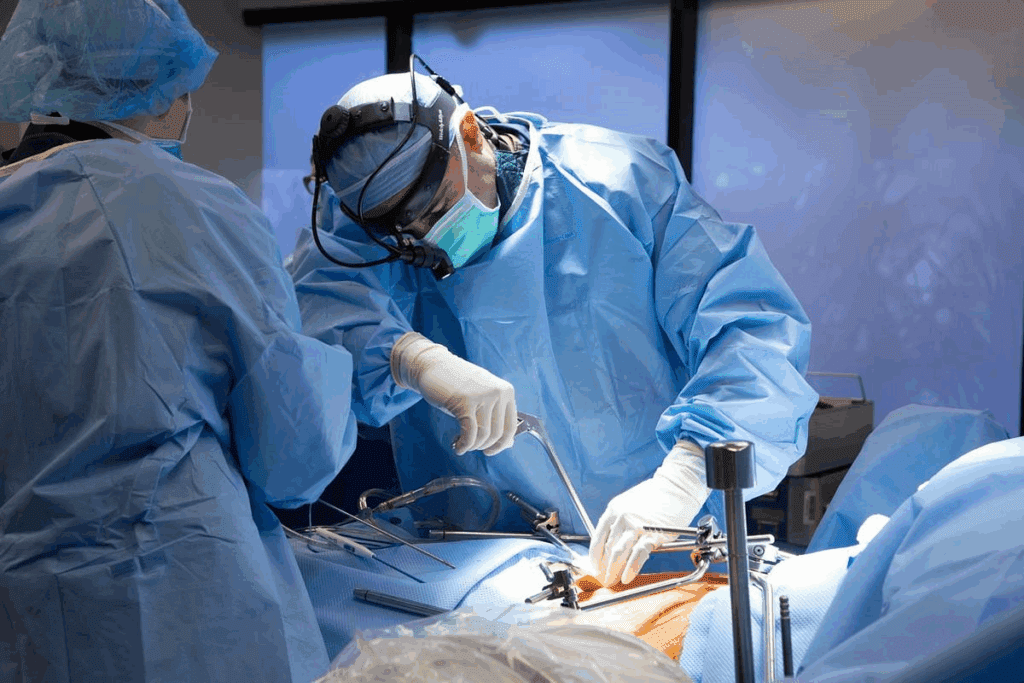
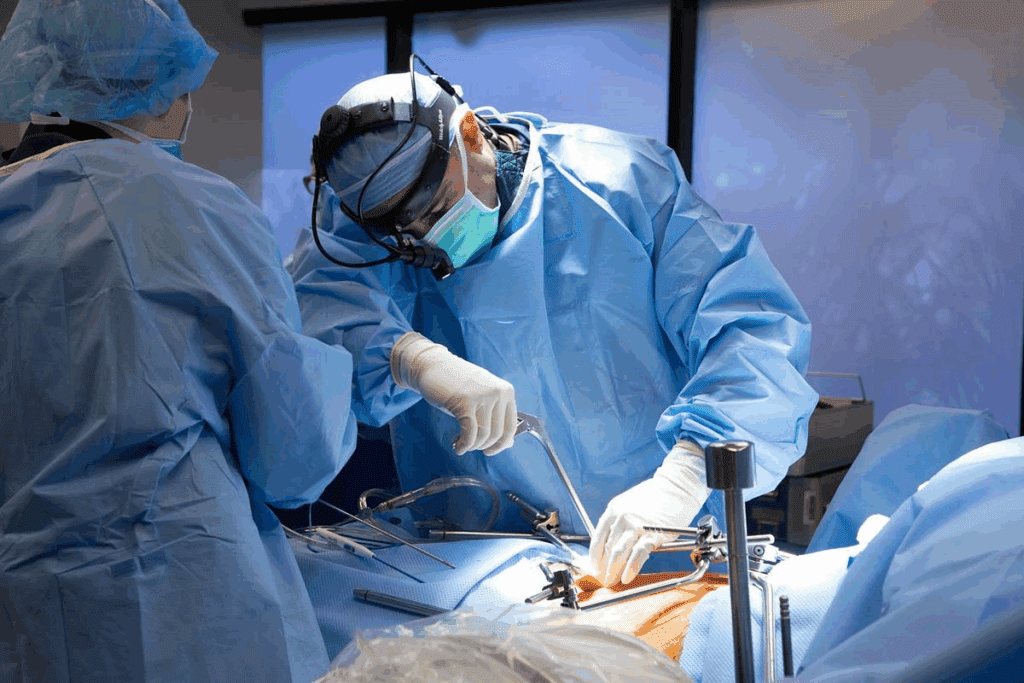
Surgical Approaches: Abdominal, Vaginal, Laparoscopic, and Robotic
The way a hysterectomy is done can vary. You can choose from abdominal, vaginal, laparoscopic, or robotic surgery. Each method has its own benefits and is chosen based on your health, the surgeon’s skill, and the surgery’s needs.
- Abdominal Hysterectomy: This method uses a big incision in the belly to reach the uterus.
- Vaginal Hysterectomy: The uterus is taken out through the vagina, leaving no scar outside.
- Laparoscopic Hysterectomy: This is a small incision surgery that uses a camera for guidance.
- Robotic Hysterectomy: A laparoscopic surgery that uses a robotic system for better precision.
Organ Removal Options: Cervix, Ovaries, and Fallopian Tubes
Deciding to remove other organs like the cervix, ovaries, and Fallopian tubes depends on your health and the surgery’s reason. Removing the ovaries can cause early menopause. Keeping them can help you keep your hormones.
Talking to your doctor about these options is important. It helps you understand the effects of each choice and make a decision that fits your health goals.
Common Medical Reasons for Recommending a Hysterectomy
Doctors often suggest a hysterectomy when other treatments don’t work or aren’t right. This surgery is considered for serious gynecological problems that affect a woman’s life quality.
Fibroids, Endometriosis, and Adenomyosis
Fibroids, endometriosis, and adenomyosis might lead to a hysterectomy. Fibroids are non-cancerous growths in the uterus causing heavy bleeding and pain. Endometriosis is when uterine tissue grows outside, causing pain. Adenomyosis is when uterine tissue grows into the walls, leading to heavy bleeding and pain.
When these conditions are severe and other treatments fail, a hysterectomy might be suggested. We’ll look into these conditions and how they affect the decision to have a hysterectomy.
Cancer and Precancerous Conditions
Cancer or precancerous conditions in the uterus, cervix, or ovaries are big reasons for a hysterectomy. For cancer, removing the uterus and sometimes more is a key treatment. Precancerous conditions might also need a hysterectomy to stop cancer from developing.
Chronic Pelvic Pain and Abnormal Bleeding
Chronic pelvic pain and abnormal uterine bleeding are also reasons for a hysterectomy. When these symptoms are severe and don’t respond to other treatments, surgery might offer relief.
Age-Related Considerations: Hysterectomies in Your 30s, 40s, and 50s
The choice to have a hysterectomy can be influenced by age. Different ages have different considerations and risks. We’ll look at how age plays a role in this decision.
| Condition | Typical Age Group | Common Symptoms |
| Fibroids | 30s-40s | Heavy bleeding, pelvic pain |
| Endometriosis | 20s-40s | Pelvic pain, infertility |
| Cancer/Precancerous Conditions | 40s-60s | Abnormal bleeding, pelvic pain |
Knowing about these conditions and their link to age can help women make informed choices about their reproductive health. It can help them decide if a hysterectomy is the right choice for them.
The Decision-Making Process: Questions to Ask Before Consenting
Before agreeing to a hysterectomy, it’s key to know the procedure, its alternatives, and possible outcomes. This big surgery choice needs careful thought and talking with healthcare experts.
Alternative Treatments Worth Exploring
Looking into other treatments before a hysterectomy is important. Options might include medicine, lifestyle changes, or less invasive surgeries. For example, women with fibroids might look into uterine artery embolization or myomectomy instead of removing the uterus.
Talking with your doctor about these options can help you understand what’s best. It’s a good idea to write down questions and worries for your visit.
Critical Questions Your Doctor May Not Volunteer
Doctors usually share important info, but some key questions might not be asked. It’s up to patients to ask about the long-term effects of surgery, possible complications, and how it might change their life quality.
- What are the possible risks and complications of this surgery?
- Are there other treatments I could try instead?
- How might this surgery affect my hormones and health?
- What’s the recovery time like, and how will it impact my daily life?
Why Some Doctors Resist Patient Requests for Hysterectomy
Doctors might not agree to a hysterectomy, worried about its irreversibility and long-term health effects. They might also think another treatment is better for you.
Knowing why your doctor might say no can lead to a better talk about your options. It’s a team effort that needs clear communication and understanding from both sides.
Insurance Coverage and Financial Considerations
When you think about getting a hysterectomy, knowing about insurance and money matters is key. These details can really shape your choices and how you feel about the whole thing.
Understanding What Insurance Typically Covers
Most health insurance plans pay for hysterectomies if they’re needed for health reasons. But, how much they cover can change a lot. It depends on your insurance, why you need the surgery, and if the doctor is in your network.
Key factors influencing insurance coverage include:
- The type of hysterectomy performed (partial, total, or radical)
- The surgical approach used (abdominal, vaginal, laparoscopic, or robotic)
- Whether the procedure is considered medically necessary or elective
Navigating Approval for Elective Hysterectomies
Getting approval for a hysterectomy you don’t need is harder. Insurance companies might ask for more info or a second opinion to say it’s okay.
Steps to facilitate approval:
- Check with your doctor to see if the surgery is really needed.
- Look at your insurance policy to see what’s covered and what’s not.
- Get approval from your insurance before you schedule the surgery.
Hidden Costs and Financial Preparation
There are costs you might not think about when planning for a hysterectomy. These include things like deductibles, copays, and what you’ll pay for care after surgery.
| Expense Category | Average Cost | Insurance Coverage |
| Surgical Fees | $5,000 – $10,000 | Partial to Full |
| Hospital Stay | $10,000 – $20,000 | Partial to Full |
| Post-Surgical Care | $500 – $2,000 | Limited |
To get ready for the costs, talk to your doctor and insurance. Making a budget for these expenses can help reduce stress about money.
Pre-Surgery Preparation: What Doctors Often Minimize
The days before a hysterectomy are key. Being well-prepared can greatly improve your recovery. Doctors give important advice, but some steps are often missed. These steps are vital for a smooth recovery.
Physical Preparation Steps
Getting your body ready is essential. Eat a healthy diet full of nutrients to aid in recovery. Also, drink lots of water to stay hydrated before surgery.
- Stop smoking weeks before surgery to avoid complications.
- Exercise but avoid hard activities that could hurt your body.
- Keep a healthy weight to lower surgery risks.
Emotional and Psychological Readiness
Getting your mind ready is as important as your body. It’s okay to feel nervous or scared before a big surgery like a hysterectomy.
“I was surprised by how much emotional preparation I needed before my hysterectomy. Talking to a therapist really helped me cope with my feelings.” – Sarah, age 42
Here are steps to help your emotional readiness:
- Seek support from loved ones or groups.
- Try relaxation methods like meditation or deep breathing.
- Learn what to expect during and after surgery.
Practical Home Preparation for Recovery
Preparing your home can make recovery easier. Make sure your home is clean and organized to avoid moving too much.
- Prepare meals ahead and freeze them for easy access.
- Get help with chores and errands.
- Set up a comfy recovery area with pillows, blankets, and entertainment.
Essential Items to Have Before Surgery
Having the right things can improve your comfort and recovery. Get comfortable clothes and personal care items ready.
| Item | Purpose |
| Comfortable clothes | Ease of wear during recovery |
| Pain management medication | Manage post-surgery pain |
| Heating pads or warm compresses | Relieve discomfort and pain |
By focusing on these often-overlooked steps, you can have a better recovery from your hysterectomy.
The Complete List of Hysterectomy Side Effects
Hysterectomy is a big surgery with many possible side effects. These can happen right after surgery or later on. Knowing about these side effects helps patients make better health choices.
Immediate Post-Surgical Complications
Right after a hysterectomy, you might face infections, bleeding, or reactions to anesthesia. It’s key to watch for signs of infection, like fever or unusual discharge. You could also get blood clots, but taking the right medicine and moving around can help prevent this.
Hormonal Changes and Their Impact
After a hysterectomy, hormonal changes can be big, like if your ovaries are taken out. Surgical menopause might happen, causing hot flashes, mood swings, and dry vagina. Doctors might suggest hormone replacement therapy (HRT) to help with these symptoms.
Long-Term Physical Side Effects
Long-term, you might notice changes in how your pelvic floor works, a higher risk of prolapse, and changes in sex life. If your ovaries are removed, you might go into early menopause. This can affect your bones and heart health over time.
Psychological and Emotional Consequences
The emotional side of a hysterectomy is just as important. Women can feel a mix of emotions, from relief to sadness, based on their situation. Having support from doctors, family, and friends is very important during this time. Some might need counseling to deal with the emotional side of surgery.
Talking to your healthcare provider about your risks and possible side effects is key. This way, you can be ready for what happens after a hysterectomy.
Recovery Timeline: Expectations vs. Reality
Recovering from a hysterectomy is different for everyone. The time it takes to heal can vary a lot. Knowing the general timeline can help you get ready for what’s coming.
Hospital Stay and Immediate Recovery
Right after surgery, you’ll need to stay in the hospital for 1 to 3 days. This depends on the type of hysterectomy you had. Medical staff will keep an eye on you, manage your pain, and watch for any problems. It’s important to follow the hospital’s post-operative care guidelines for a smooth start to your recovery.
Weeks 1-6: The Critical Healing Period
The first six weeks are very important for healing. You might feel very tired and emotional. Resting is key during this time, and you should avoid heavy lifting, bending, or hard activities. As you get better, listen to your body and don’t rush things.
Months 2-12: Adjusting to Your New Normal
By the second month, you’ll likely feel more energetic and comfortable. But, it can take up to a year to fully recover. You’ll be getting used to the physical and emotional changes after your surgery. It’s important to keep up with follow-up appointments with your healthcare provider to check on your healing and address any issues.
Physical Activities to Avoid and When to Resume Them
For 6 to 8 weeks after surgery, it’s best to avoid heavy lifting, hard exercise, and sex. The exact time will depend on your surgeon’s advice and how you’re healing. Start adding activities back in slowly as you feel more ready, and always check with your healthcare provider if you’re unsure.
Sexual Health After Hysterectomy: Breaking the Silence
Having a hysterectomy can change your life. It’s important to know how it affects your sex life. The surgery can help with heavy bleeding or pain but might also change how you feel during sex.
Physical Changes Affecting Intimacy
After a hysterectomy, you might notice some physical changes. These can affect how you feel during sex. The surgery can also change the nerves in your pelvic area, which might affect your arousal and orgasm.
Key physical changes include:
- Shortening or narrowing of the vagina
- Changes in vaginal lubrication
- Potential decrease in libido due to hormonal changes
When It’s Safe to Resume Sexual Activity
When you can start having sex again depends on your surgery and healing. Doctors usually say wait 6 to 8 weeks. This helps avoid problems like infection or bleeding.
It’s essential to follow your healthcare provider’s advice and listen to your body. If you feel pain or discomfort during sex, talk to your doctor.
Addressing Concerns with Partners
Talking openly with your partner is key during recovery and after. Share your feelings and any changes you notice. This can make your relationship stronger and more intimate. It’s also good to teach your partner about the changes you might go through.
Potential Issues with Arousal and Orgasm
Some women might notice changes in arousal and orgasm after a hysterectomy. Hormonal changes, nerve damage, and psychological factors can play a role. If these changes bother you, talk to a healthcare provider or sex therapist.
Knowing these changes are part of recovery can help. It lets you manage your expectations and find support when needed.
Hormonal Considerations: With and Without Ovary Removal
Having a hysterectomy can change a woman’s hormones, with or without removing the ovaries. The impact varies based on several factors. These include whether the ovaries are kept or removed during surgery.
Understanding Surgical Menopause
Surgical menopause happens when a hysterectomy is done, often with the ovaries removed. This leads to a sudden drop in hormone levels, causing menopause symptoms. Even if the ovaries stay, some women might see a decrease in their function after surgery.
Surgical Menopause vs. Natural Menopause: Surgical menopause can be more sudden and severe than natural menopause. Knowing this helps manage expectations and find the right treatments.
Hormone Replacement Therapy: Pros and Cons
Hormone Replacement Therapy (HRT) is often suggested to ease surgical menopause symptoms. HRT involves taking hormones to replace those the body no longer makes.
| HRT Benefits | HRT Risks |
| Relief from hot flashes and night sweats | Increased risk of breast cancer |
| Improved vaginal health | Risk of blood clots |
| Reduced risk of osteoporosis | Potential for stroke |
Talking to a healthcare provider about HRT’s pros and cons is key to finding the best option.
Natural Approaches to Hormonal Balance
For those avoiding HRT or seeking natural ways, there are options. These include changing your diet, managing stress, and using certain supplements.
- Dietary adjustments to support hormonal health
- Stress reduction techniques like yoga or meditation
- Supplements such as omega-3 fatty acids and vitamin D
The Role of Progesterone After Hysterectomy
Progesterone is important for women’s health. After a hysterectomy, you might need progesterone therapy, depending on your situation.
The balance between estrogen and progesterone is vital to avoid certain health issues. Progesterone can also help with anxiety and insomnia.
The Psychological Impact: Identity and Emotional Healing
Having a hysterectomy changes a woman’s life in many ways. It’s not just a physical change. It also affects her emotional and psychological health. The surgery can save lives or greatly improve quality of life. But it brings a mix of emotions that need to be faced and healed.
Grief, Loss, and Processing Change
Women often feel grief and loss after a hysterectomy. This can be because of the loss of the uterus, a symbol of being a woman. Or it might be because they can’t have children anymore. It’s important to accept these feelings and give yourself time to process them.
Key emotions that may arise include:
- Sadness and Mourning: For the loss of reproductive capabilities or the end of menstrual cycles.
- Anxiety: About the future, the impact on identity, or changes in sexual function.
- Relief: For the end of painful or heavy menstrual periods, or health issues resolved.
Support Resources and Coping Strategies
Having a strong support system is key for healing. This can be family, friends, support groups, or professional counseling. Hearing others’ stories can be comforting and make you feel less alone.
Coping strategies may involve:
- Using mindfulness and relaxation techniques to handle stress and anxiety.
- Joining support groups to connect with others who’ve gone through similar things.
- Practicing self-care, doing things that make you feel good and define you beyond your body.
Body Image and Femininity Concerns
A hysterectomy can affect how women see themselves. They might feel different physically and in their reproductive identity. It’s important to talk about these feelings with healthcare providers, partners, and counselors.
Considerations for body image and femininity include:
- Remembering that femininity is not just about reproductive abilities.
- Finding ways to reconnect with your body, like through exercise, creative activities, or intimacy.
- Getting professional help to deal with complex emotions and changes.
Long-Term Health Considerations Post-Hysterectomy
A hysterectomy is a life-saving surgery for many women. Yet, it brings up many long-term health issues. It’s important to know how it can affect different parts of a woman’s health.
Bone Health and Osteoporosis Risk
One big concern after a hysterectomy is bone health. When the ovaries are removed, estrogen levels drop sharply. Estrogen helps keep bones strong. So, women without ovaries are more likely to get osteoporosis.
It’s key for them to talk to their doctor about hormone therapy or other treatments to lower this risk.
Cardiovascular Implications
Hysterectomy can also affect heart health. Women, and those without ovaries in particular, might face a higher risk of heart disease. This is because estrogen levels drop, which can harm the heart.
Keeping a healthy lifestyle, like eating right and exercising, is important to reduce this risk.
Ongoing Health Monitoring Needs
Women who’ve had a hysterectomy need regular health checks. These visits can catch problems like osteoporosis and heart disease early. It’s also a chance to talk about any health worries or symptoms.
Cancer Risk Assessment After Hysterectomy
Having a hysterectomy can change cancer risks. For example, it removes the risk of uterine cancer. But, it might not change the risk of ovarian cancer if the ovaries are left. Knowing these risks helps women make better health choices.
Women should talk to their doctor about their specific risks.
Being aware of these health concerns helps women stay healthy after a hysterectomy. It’s about making smart choices and working with doctors for the best health outcomes.
Real Stories: What Women Wish They Had Known
Many women who had a hysterectomy share their stories. They talk about how the surgery changed their lives. Their stories help others who might be thinking about it.
Testimonials and Shared Experiences
Women who had a hysterectomy feel many emotions. Some wish they knew more about side effects like hormonal changes. These changes can affect their health a lot.
One woman said she didn’t know how long it would take to get better. She had to slow down and adjust to her new pace.
Common Regrets and Positive Outcomes
Some women regret their decision to have a hysterectomy. But many are happy with the results. They feel better from chronic pain and abnormal bleeding.
| Common Regrets | Positive Outcomes |
| Lack of information about side effects | Relief from chronic pain |
| Insufficient support during recovery | Improved quality of life |
| Unexpected emotional changes | Resolution of abnormal bleeding |
Celebrity Experiences with Hysterectomy
Celebrities also talk about their hysterectomies. For example, Christina Applegate had one after breast cancer. She talked about her genetic health risks.
Stories from both regular women and celebrities are important. They show how key it is to know what to expect from a hysterectomy.
Conclusion: Making an Informed Decision About Your Reproductive Health
When it comes to hysterectomy, making a choice is big. We’ve looked at many sides of this surgery. This includes the types of procedures, their effects, and long-term health impacts.
Knowing a lot about your health is key. Understanding why a hysterectomy might be needed helps you make a better choice. Talk to your doctor about all your options. This way, you can make a choice that’s right for you.
Choosing what’s best for your reproductive health is a big decision. Stay informed and get support. This will help you make a choice that’s good for your overall health and well-being.
FAQ
What is a hysterectomy?
A hysterectomy is a surgery where the uterus is removed. Sometimes, other reproductive organs are taken out too.
What are the different types of hysterectomy procedures?
There are several types. These include partial, total, and radical hysterectomies. Each has its own surgical method.
Why is a hysterectomy recommended?
Doctors might suggest it for many reasons. This includes fibroids, endometriosis, cancer, and abnormal bleeding.
Will I experience menopause after a hysterectomy?
If your ovaries are removed, you might go into menopause right away. But, if they’re left in, you might not right away.
How long does it take to recover from a hysterectomy?
Recovery time varies. It can take weeks to months, depending on the surgery and the person.
Can I have sex after a hysterectomy?
Yes, but wait until your doctor says it’s okay. This is usually after a few weeks or months.
Will insurance cover a hysterectomy?
Insurance coverage depends on your policy and the reason for the surgery. Always check with your provider.
What are the possible side effects of a hysterectomy?
Side effects can include immediate complications, hormonal changes, and long-term physical and mental effects.
Can I get ovarian cancer after a hysterectomy?
Yes, you can. Even if your ovaries are left in or removed, you’re at risk for ovarian cancer. The risk might be lower, though.
How will a hysterectomy affect my hormone levels?
If your ovaries are removed, your hormone levels will change. You might need hormone replacement therapy.
What are the benefits of a partial hysterectomy?
A partial hysterectomy might save some reproductive organs. It could also lower the risk of some complications.
Can I have a hysterectomy without removing my ovaries?
Yes, it’s possible. Not removing your ovaries can help keep your hormone levels balanced.
How common are hysterectomies?
Hysterectomies are quite common. A lot are done every year around the world.
What should I expect during the recovery process?
Expect to stay in the hospital, then rest and slowly get back to normal. You’ll have some physical limits.
Are there any alternative treatments to hysterectomy?
Depending on your condition, there might be other treatments. It’s important to talk to your doctor about these options.
Can I experience menstrual-like symptoms after a hysterectomy?
Yes, some women might have symptoms like cramps after a hysterectomy. The frequency and severity can vary.
Reference:
PubMed – Clarke-Pearson DL. Complications of hysterectomy. Obstetrics & Gynecology Review, 2013. https://pubmed.ncbi.nlm.nih.gov/23635631/
Nearly 600,000 women in the United States have uterus removal surgery every year. It’s one of the most common surgeries. Yet, many women don’t know the long-term effects of this surgery.
It’s important for women to know everything about a hysterectomy. This includes its benefits and possible long-term health issues. Knowing this helps women make better choices about their reproductive health.
Key Takeaways
- Understanding what a hysterectomy is and its implications.
- The importance of being informed about the procedure.
- Potential long-term health consequences of uterus removal.
- Factors to consider before undergoing a hysterectomy.
- The role of a hysterectomy in women’s reproductive health.
Understanding Hysterectomy: More Than Just Uterus Removal
A hysterectomy is more than uterus removal; it’s a surgery with a long medical history. It has big effects on a woman’s health, beyond just removing an organ.
Definition and Basic Procedure
A hysterectomy is when a woman’s uterus is surgically removed. The surgeon might also take out the cervix, ovaries, or fallopian tubes. This depends on the reason for the surgery and the type of hysterectomy.
The surgeon makes an incision in the belly or goes through the vagina. The goal is to remove the uterus and sometimes other organs.
The decision to remove additional organs depends on the patient’s health, the surgery’s reason, and what the patient wants.
Historical Context and Evolution of the Procedure
The first hysterectomy was done in the late 19th century. Over time, the surgery has changed a lot. It’s now done with better techniques, anesthesia, and care after surgery.
At first, hysterectomies were only for life-threatening issues. Now, they’re also done to improve a woman’s quality of life. This includes treating severe endometriosis or uterine fibroids.
The Prevalence of Hysterectomies in the United States
Hysterectomies are very common in the U.S. Health statistics show hundreds of thousands of women have this surgery every year. This is because of conditions like uterine fibroids, endometriosis, and some cancers.
Knowing why hysterectomies are common helps women make better choices about their reproductive health.
Types of Hysterectomy Procedures Explained

Understanding the different types of hysterectomy procedures is key to making a well-informed decision. A hysterectomy is a big surgery done for many medical reasons. The type of surgery you need depends on your health, the reason for the surgery, and what you prefer.
Partial Hysterectomy vs. Total Hysterectomy
A partial hysterectomy removes the uterus but keeps the cervix. This is often chosen when the problem is only in the uterus. A total hysterectomy removes both the uterus and cervix. The choice depends on your health and the reason for the surgery.
It’s important to know the differences to make the right choice for you. A partial hysterectomy might be right for some, but a total hysterectomy is needed for others, like cancer or severe cervical disease.
Surgical Approaches: Abdominal, Vaginal, Laparoscopic, and Robotic
The way a hysterectomy is done can vary. You can choose from abdominal, vaginal, laparoscopic, or robotic surgery. Each method has its own benefits and is chosen based on your health, the surgeon’s skill, and the surgery’s needs.
- Abdominal Hysterectomy: This method uses a big incision in the belly to reach the uterus.
- Vaginal Hysterectomy: The uterus is taken out through the vagina, leaving no scar outside.
- Laparoscopic Hysterectomy: This is a small incision surgery that uses a camera for guidance.
- Robotic Hysterectomy: A laparoscopic surgery that uses a robotic system for better precision.
Organ Removal Options: Cervix, Ovaries, and Fallopian Tubes
Deciding to remove other organs like the cervix, ovaries, and Fallopian tubes depends on your health and the surgery’s reason. Removing the ovaries can cause early menopause. Keeping them can help you keep your hormones.
Talking to your doctor about these options is important. It helps you understand the effects of each choice and make a decision that fits your health goals.
Common Medical Reasons for Recommending a Hysterectomy
Doctors often suggest a hysterectomy when other treatments don’t work or aren’t right. This surgery is considered for serious gynecological problems that affect a woman’s life quality.
Fibroids, Endometriosis, and Adenomyosis
Fibroids, endometriosis, and adenomyosis might lead to a hysterectomy. Fibroids are non-cancerous growths in the uterus causing heavy bleeding and pain. Endometriosis is when uterine tissue grows outside, causing pain. Adenomyosis is when uterine tissue grows into the walls, leading to heavy bleeding and pain.
When these conditions are severe and other treatments fail, a hysterectomy might be suggested. We’ll look into these conditions and how they affect the decision to have a hysterectomy.
Cancer and Precancerous Conditions
Cancer or precancerous conditions in the uterus, cervix, or ovaries are big reasons for a hysterectomy. For cancer, removing the uterus and sometimes more is a key treatment. Precancerous conditions might also need a hysterectomy to stop cancer from developing.
Chronic Pelvic Pain and Abnormal Bleeding
Chronic pelvic pain and abnormal uterine bleeding are also reasons for a hysterectomy. When these symptoms are severe and don’t respond to other treatments, surgery might offer relief.
Age-Related Considerations: Hysterectomies in Your 30s, 40s, and 50s
The choice to have a hysterectomy can be influenced by age. Different ages have different considerations and risks. We’ll look at how age plays a role in this decision.
| Condition | Typical Age Group | Common Symptoms |
| Fibroids | 30s-40s | Heavy bleeding, pelvic pain |
| Endometriosis | 20s-40s | Pelvic pain, infertility |
| Cancer/Precancerous Conditions | 40s-60s | Abnormal bleeding, pelvic pain |
Knowing about these conditions and their link to age can help women make informed choices about their reproductive health. It can help them decide if a hysterectomy is the right choice for them.
The Decision-Making Process: Questions to Ask Before Consenting
Before agreeing to a hysterectomy, it’s key to know the procedure, its alternatives, and possible outcomes. This big surgery choice needs careful thought and talking with healthcare experts.
Alternative Treatments Worth Exploring
Looking into other treatments before a hysterectomy is important. Options might include medicine, lifestyle changes, or less invasive surgeries. For example, women with fibroids might look into uterine artery embolization or myomectomy instead of removing the uterus.
Talking with your doctor about these options can help you understand what’s best. It’s a good idea to write down questions and worries for your visit.
Critical Questions Your Doctor May Not Volunteer
Doctors usually share important info, but some key questions might not be asked. It’s up to patients to ask about the long-term effects of surgery, possible complications, and how it might change their life quality.
- What are the possible risks and complications of this surgery?
- Are there other treatments I could try instead?
- How might this surgery affect my hormones and health?
- What’s the recovery time like, and how will it impact my daily life?
Why Some Doctors Resist Patient Requests for Hysterectomy
Doctors might not agree to a hysterectomy, worried about its irreversibility and long-term health effects. They might also think another treatment is better for you.
Knowing why your doctor might say no can lead to a better talk about your options. It’s a team effort that needs clear communication and understanding from both sides.
Insurance Coverage and Financial Considerations
When you think about getting a hysterectomy, knowing about insurance and money matters is key. These details can really shape your choices and how you feel about the whole thing.
Understanding What Insurance Typically Covers
Most health insurance plans pay for hysterectomies if they’re needed for health reasons. But, how much they cover can change a lot. It depends on your insurance, why you need the surgery, and if the doctor is in your network.
Key factors influencing insurance coverage include:
- The type of hysterectomy performed (partial, total, or radical)
- The surgical approach used (abdominal, vaginal, laparoscopic, or robotic)
- Whether the procedure is considered medically necessary or elective
Navigating Approval for Elective Hysterectomies
Getting approval for a hysterectomy you don’t need is harder. Insurance companies might ask for more info or a second opinion to say it’s okay.
Steps to facilitate approval:
- Check with your doctor to see if the surgery is really needed.
- Look at your insurance policy to see what’s covered and what’s not.
- Get approval from your insurance before you schedule the surgery.
Hidden Costs and Financial Preparation
There are costs you might not think about when planning for a hysterectomy. These include things like deductibles, copays, and what you’ll pay for care after surgery.
| Expense Category | Average Cost | Insurance Coverage |
| Surgical Fees | $5,000 – $10,000 | Partial to Full |
| Hospital Stay | $10,000 – $20,000 | Partial to Full |
| Post-Surgical Care | $500 – $2,000 | Limited |
To get ready for the costs, talk to your doctor and insurance. Making a budget for these expenses can help reduce stress about money.
Pre-Surgery Preparation: What Doctors Often Minimize
The days before a hysterectomy are key. Being well-prepared can greatly improve your recovery. Doctors give important advice, but some steps are often missed. These steps are vital for a smooth recovery.
Physical Preparation Steps
Getting your body ready is essential. Eat a healthy diet full of nutrients to aid in recovery. Also, drink lots of water to stay hydrated before surgery.
- Stop smoking weeks before surgery to avoid complications.
- Exercise but avoid hard activities that could hurt your body.
- Keep a healthy weight to lower surgery risks.
Emotional and Psychological Readiness
Getting your mind ready is as important as your body. It’s okay to feel nervous or scared before a big surgery like a hysterectomy.
“I was surprised by how much emotional preparation I needed before my hysterectomy. Talking to a therapist really helped me cope with my feelings.” – Sarah, age 42
Here are steps to help your emotional readiness:
- Seek support from loved ones or groups.
- Try relaxation methods like meditation or deep breathing.
- Learn what to expect during and after surgery.
Practical Home Preparation for Recovery
Preparing your home can make recovery easier. Make sure your home is clean and organized to avoid moving too much.
- Prepare meals ahead and freeze them for easy access.
- Get help with chores and errands.
- Set up a comfy recovery area with pillows, blankets, and entertainment.
Essential Items to Have Before Surgery
Having the right things can improve your comfort and recovery. Get comfortable clothes and personal care items ready.
| Item | Purpose |
| Comfortable clothes | Ease of wear during recovery |
| Pain management medication | Manage post-surgery pain |
| Heating pads or warm compresses | Relieve discomfort and pain |
By focusing on these often-overlooked steps, you can have a better recovery from your hysterectomy.
The Complete List of Hysterectomy Side Effects
Hysterectomy is a big surgery with many possible side effects. These can happen right after surgery or later on. Knowing about these side effects helps patients make better health choices.
Immediate Post-Surgical Complications
Right after a hysterectomy, you might face infections, bleeding, or reactions to anesthesia. It’s key to watch for signs of infection, like fever or unusual discharge. You could also get blood clots, but taking the right medicine and moving around can help prevent this.
Hormonal Changes and Their Impact
After a hysterectomy, hormonal changes can be big, like if your ovaries are taken out. Surgical menopause might happen, causing hot flashes, mood swings, and dry vagina. Doctors might suggest hormone replacement therapy (HRT) to help with these symptoms.
Long-Term Physical Side Effects
Long-term, you might notice changes in how your pelvic floor works, a higher risk of prolapse, and changes in sex life. If your ovaries are removed, you might go into early menopause. This can affect your bones and heart health over time.
Psychological and Emotional Consequences
The emotional side of a hysterectomy is just as important. Women can feel a mix of emotions, from relief to sadness, based on their situation. Having support from doctors, family, and friends is very important during this time. Some might need counseling to deal with the emotional side of surgery.
Talking to your healthcare provider about your risks and possible side effects is key. This way, you can be ready for what happens after a hysterectomy.
Recovery Timeline: Expectations vs. Reality
Recovering from a hysterectomy is different for everyone. The time it takes to heal can vary a lot. Knowing the general timeline can help you get ready for what’s coming.
Hospital Stay and Immediate Recovery
Right after surgery, you’ll need to stay in the hospital for 1 to 3 days. This depends on the type of hysterectomy you had. Medical staff will keep an eye on you, manage your pain, and watch for any problems. It’s important to follow the hospital’s post-operative care guidelines for a smooth start to your recovery.
Weeks 1-6: The Critical Healing Period
The first six weeks are very important for healing. You might feel very tired and emotional. Resting is key during this time, and you should avoid heavy lifting, bending, or hard activities. As you get better, listen to your body and don’t rush things.
Months 2-12: Adjusting to Your New Normal
By the second month, you’ll likely feel more energetic and comfortable. But, it can take up to a year to fully recover. You’ll be getting used to the physical and emotional changes after your surgery. It’s important to keep up with follow-up appointments with your healthcare provider to check on your healing and address any issues.
Physical Activities to Avoid and When to Resume Them
For 6 to 8 weeks after surgery, it’s best to avoid heavy lifting, hard exercise, and sex. The exact time will depend on your surgeon’s advice and how you’re healing. Start adding activities back in slowly as you feel more ready, and always check with your healthcare provider if you’re unsure.
Sexual Health After Hysterectomy: Breaking the Silence
Having a hysterectomy can change your life. It’s important to know how it affects your sex life. The surgery can help with heavy bleeding or pain but might also change how you feel during sex.
Physical Changes Affecting Intimacy
After a hysterectomy, you might notice some physical changes. These can affect how you feel during sex. The surgery can also change the nerves in your pelvic area, which might affect your arousal and orgasm.
Key physical changes include:
- Shortening or narrowing of the vagina
- Changes in vaginal lubrication
- Potential decrease in libido due to hormonal changes
When It’s Safe to Resume Sexual Activity
When you can start having sex again depends on your surgery and healing. Doctors usually say wait 6 to 8 weeks. This helps avoid problems like infection or bleeding.
It’s essential to follow your healthcare provider’s advice and listen to your body. If you feel pain or discomfort during sex, talk to your doctor.
Addressing Concerns with Partners
Talking openly with your partner is key during recovery and after. Share your feelings and any changes you notice. This can make your relationship stronger and more intimate. It’s also good to teach your partner about the changes you might go through.
Potential Issues with Arousal and Orgasm
Some women might notice changes in arousal and orgasm after a hysterectomy. Hormonal changes, nerve damage, and psychological factors can play a role. If these changes bother you, talk to a healthcare provider or sex therapist.
Knowing these changes are part of recovery can help. It lets you manage your expectations and find support when needed.
Hormonal Considerations: With and Without Ovary Removal
Having a hysterectomy can change a woman’s hormones, with or without removing the ovaries. The impact varies based on several factors. These include whether the ovaries are kept or removed during surgery.
Understanding Surgical Menopause
Surgical menopause happens when a hysterectomy is done, often with the ovaries removed. This leads to a sudden drop in hormone levels, causing menopause symptoms. Even if the ovaries stay, some women might see a decrease in their function after surgery.
Surgical Menopause vs. Natural Menopause: Surgical menopause can be more sudden and severe than natural menopause. Knowing this helps manage expectations and find the right treatments.
Hormone Replacement Therapy: Pros and Cons
Hormone Replacement Therapy (HRT) is often suggested to ease surgical menopause symptoms. HRT involves taking hormones to replace those the body no longer makes.
| HRT Benefits | HRT Risks |
| Relief from hot flashes and night sweats | Increased risk of breast cancer |
| Improved vaginal health | Risk of blood clots |
| Reduced risk of osteoporosis | Potential for stroke |
Talking to a healthcare provider about HRT’s pros and cons is key to finding the best option.
Natural Approaches to Hormonal Balance
For those avoiding HRT or seeking natural ways, there are options. These include changing your diet, managing stress, and using certain supplements.
- Dietary adjustments to support hormonal health
- Stress reduction techniques like yoga or meditation
- Supplements such as omega-3 fatty acids and vitamin D
The Role of Progesterone After Hysterectomy
Progesterone is important for women’s health. After a hysterectomy, you might need progesterone therapy, depending on your situation.
The balance between estrogen and progesterone is vital to avoid certain health issues. Progesterone can also help with anxiety and insomnia.
The Psychological Impact: Identity and Emotional Healing
Having a hysterectomy changes a woman’s life in many ways. It’s not just a physical change. It also affects her emotional and psychological health. The surgery can save lives or greatly improve quality of life. But it brings a mix of emotions that need to be faced and healed.
Grief, Loss, and Processing Change
Women often feel grief and loss after a hysterectomy. This can be because of the loss of the uterus, a symbol of being a woman. Or it might be because they can’t have children anymore. It’s important to accept these feelings and give yourself time to process them.
Key emotions that may arise include:
- Sadness and Mourning: For the loss of reproductive capabilities or the end of menstrual cycles.
- Anxiety: About the future, the impact on identity, or changes in sexual function.
- Relief: For the end of painful or heavy menstrual periods, or health issues resolved.
Support Resources and Coping Strategies
Having a strong support system is key for healing. This can be family, friends, support groups, or professional counseling. Hearing others’ stories can be comforting and make you feel less alone.
Coping strategies may involve:
- Using mindfulness and relaxation techniques to handle stress and anxiety.
- Joining support groups to connect with others who’ve gone through similar things.
- Practicing self-care, doing things that make you feel good and define you beyond your body.
Body Image and Femininity Concerns
A hysterectomy can affect how women see themselves. They might feel different physically and in their reproductive identity. It’s important to talk about these feelings with healthcare providers, partners, and counselors.
Considerations for body image and femininity include:
- Remembering that femininity is not just about reproductive abilities.
- Finding ways to reconnect with your body, like through exercise, creative activities, or intimacy.
- Getting professional help to deal with complex emotions and changes.
Long-Term Health Considerations Post-Hysterectomy
A hysterectomy is a life-saving surgery for many women. Yet, it brings up many long-term health issues. It’s important to know how it can affect different parts of a woman’s health.
Bone Health and Osteoporosis Risk
One big concern after a hysterectomy is bone health. When the ovaries are removed, estrogen levels drop sharply. Estrogen helps keep bones strong. So, women without ovaries are more likely to get osteoporosis.
It’s key for them to talk to their doctor about hormone therapy or other treatments to lower this risk.
Cardiovascular Implications
Hysterectomy can also affect heart health. Women, and those without ovaries in particular, might face a higher risk of heart disease. This is because estrogen levels drop, which can harm the heart.
Keeping a healthy lifestyle, like eating right and exercising, is important to reduce this risk.
Ongoing Health Monitoring Needs
Women who’ve had a hysterectomy need regular health checks. These visits can catch problems like osteoporosis and heart disease early. It’s also a chance to talk about any health worries or symptoms.
Cancer Risk Assessment After Hysterectomy
Having a hysterectomy can change cancer risks. For example, it removes the risk of uterine cancer. But, it might not change the risk of ovarian cancer if the ovaries are left. Knowing these risks helps women make better health choices.
Women should talk to their doctor about their specific risks.
Being aware of these health concerns helps women stay healthy after a hysterectomy. It’s about making smart choices and working with doctors for the best health outcomes.
Real Stories: What Women Wish They Had Known
Many women who had a hysterectomy share their stories. They talk about how the surgery changed their lives. Their stories help others who might be thinking about it.
Testimonials and Shared Experiences
Women who had a hysterectomy feel many emotions. Some wish they knew more about side effects like hormonal changes. These changes can affect their health a lot.
One woman said she didn’t know how long it would take to get better. She had to slow down and adjust to her new pace.
Common Regrets and Positive Outcomes
Some women regret their decision to have a hysterectomy. But many are happy with the results. They feel better from chronic pain and abnormal bleeding.
| Common Regrets | Positive Outcomes |
| Lack of information about side effects | Relief from chronic pain |
| Insufficient support during recovery | Improved quality of life |
| Unexpected emotional changes | Resolution of abnormal bleeding |
Celebrity Experiences with Hysterectomy
Celebrities also talk about their hysterectomies. For example, Christina Applegate had one after breast cancer. She talked about her genetic health risks.
Stories from both regular women and celebrities are important. They show how key it is to know what to expect from a hysterectomy.
Conclusion: Making an Informed Decision About Your Reproductive Health
When it comes to hysterectomy, making a choice is big. We’ve looked at many sides of this surgery. This includes the types of procedures, their effects, and long-term health impacts.
Knowing a lot about your health is key. Understanding why a hysterectomy might be needed helps you make a better choice. Talk to your doctor about all your options. This way, you can make a choice that’s right for you.
Choosing what’s best for your reproductive health is a big decision. Stay informed and get support. This will help you make a choice that’s good for your overall health and well-being.
FAQ
What is a hysterectomy?
A hysterectomy is a surgery where the uterus is removed. Sometimes, other reproductive organs are taken out too.
What are the different types of hysterectomy procedures?
There are several types. These include partial, total, and radical hysterectomies. Each has its own surgical method.
Why is a hysterectomy recommended?
Doctors might suggest it for many reasons. This includes fibroids, endometriosis, cancer, and abnormal bleeding.
Will I experience menopause after a hysterectomy?
If your ovaries are removed, you might go into menopause right away. But, if they’re left in, you might not right away.
How long does it take to recover from a hysterectomy?
Recovery time varies. It can take weeks to months, depending on the surgery and the person.
Can I have sex after a hysterectomy?
Yes, but wait until your doctor says it’s okay. This is usually after a few weeks or months.
Will insurance cover a hysterectomy?
Insurance coverage depends on your policy and the reason for the surgery. Always check with your provider.
What are the possible side effects of a hysterectomy?
Side effects can include immediate complications, hormonal changes, and long-term physical and mental effects.
Can I get ovarian cancer after a hysterectomy?
Yes, you can. Even if your ovaries are left in or removed, you’re at risk for ovarian cancer. The risk might be lower, though.
How will a hysterectomy affect my hormone levels?
If your ovaries are removed, your hormone levels will change. You might need hormone replacement therapy.
What are the benefits of a partial hysterectomy?
A partial hysterectomy might save some reproductive organs. It could also lower the risk of some complications.
Can I have a hysterectomy without removing my ovaries?
Yes, it’s possible. Not removing your ovaries can help keep your hormone levels balanced.
How common are hysterectomies?
Hysterectomies are quite common. A lot are done every year around the world.
What should I expect during the recovery process?
Expect to stay in the hospital, then rest and slowly get back to normal. You’ll have some physical limits.
Are there any alternative treatments to hysterectomy?
Depending on your condition, there might be other treatments. It’s important to talk to your doctor about these options.
Can I experience menstrual-like symptoms after a hysterectomy?
Yes, some women might have symptoms like cramps after a hysterectomy. The frequency and severity can vary.
Reference:
PubMed – Clarke-Pearson DL. Complications of hysterectomy. Obstetrics & Gynecology Review, 2013. https://pubmed.ncbi.nlm.nih.gov/23635631/





