Did you know that diverticulitis affects millions of people worldwide? It leads to high healthcare costs and a lot of work for doctors. Accurate diagnosis and coding are essential for effectively managing this condition.
We will look into why the right ICD-10 code for diverticulitis matters. The code K57.92 is for cases without perforation, abscess, or bleeding. Knowing this code helps doctors bill correctly and keep patient records accurate.
The 2025 edition of ICD-10-CM K57.92 started on October 1, 2024. It’s for diverticulitis of the intestine, without perforation or abscess, and without bleeding. Using the right code is important for getting paid and keeping medical records up to date.
Key Takeaways
- The ICD-10 code K57.92 is used for diverticulitis cases without perforation, abscess, or bleeding.
- Accurate coding is key for healthcare providers to bill right and manage patient records well.
- The 2025 edition of ICD-10-CM K57.92 became effective on October 1, 2024.
- Using the correct ICD-10 code is vital for reimbursement and keeping medical records accurate.
- Diverticulitis diagnosis and coding have a big impact on healthcare costs and work.
Overview of Diverticulitis
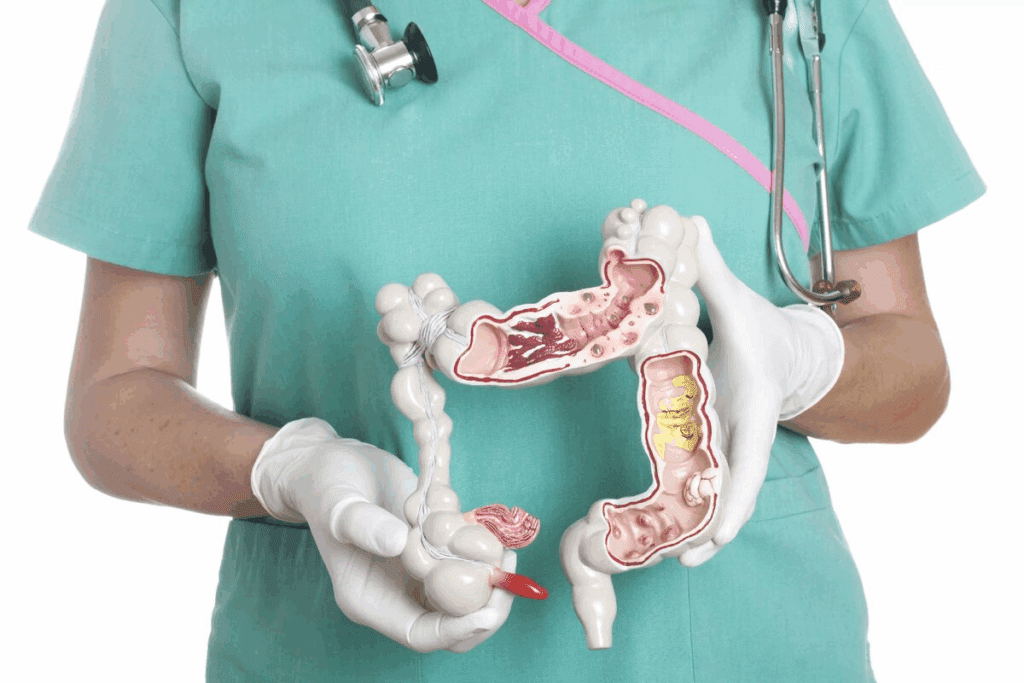
Diverticulitis is a condition that affects the digestive system. It involves inflammation of small pouches in the intestine wall. Understanding it means looking at its definition, causes, and symptoms.
Definition and Causes
Diverticulitis is when these small pouches get inflamed. It can happen due to a low-fiber diet, age, and lifestyle. The K57 series classification in the ICD-10 coding system covers diverticular diseases, including diverticulitis.
Older adults are more likely to get diverticulitis. A diet low in fiber can cause constipation. This increases pressure in the colon, which might lead to diverticula formation.
Symptoms of Diverticulitis
Symptoms of diverticulitis can vary. They include abdominal pain, changes in bowel habits, and fever. In severe cases, symptoms can worsen, indicating complications like perforation abscess.
Some people may have more severe symptoms. These include intense pain, high fever, and significant changes in bowel habits. These symptoms need immediate medical attention.
Risk Factors Involved
Several factors increase the risk of diverticulitis. Age is a big factor, with risk rising after 40. A low-fiber diet and lifestyle factors like lack of exercise and obesity also play a role.
Knowing these risk factors is key to prevention and early diagnosis. For example, a high-fiber diet can help prevent diverticula formation.
Risk Factor | Description |
Age | Increased risk after age 40 |
Diet | Low-fiber diet contributes to diverticula formation |
Lifestyle | Lack of physical activity and obesity are risk factors |
Understanding ICD-10 Codes
Accurate ICD-10 coding is key in healthcare. It makes sure patient diagnoses and procedures are documented right. The ICD-10 coding system, or the International Classification of Diseases, 10th Revision, is used worldwide. It covers health issues like diverticulitis of the large intestine.
What is ICD-10?
The ICD-10 is a detailed coding system. It helps healthcare providers classify diagnoses and procedures accurately. It includes codes for many conditions, like diverticulitis, which falls under the ICD10 large intestine category.
This system aims to make health data more specific and accurate. It helps in better patient care and precise billing.
ICD-10-CM codes are key for clinical documentation. They help create detailed patient records. These records are vital for treatment and insurance purposes. Accurate codes ensure healthcare providers get paid correctly for their work.
Importance of Accurate Coding
Accurate ICD-10 coding is important for several reasons. It ensures healthcare providers get paid right through billable ICD‑10 codes. It also helps in collecting vital health statistics for policy and research.
Accurate coding also improves patient care. It makes sure medical records are precise and complete. This is important for treatment and insurance.
Using the right ICD-10 codes also reduces billing errors. These errors can cause denied claims and delayed payments. By using the correct codes, healthcare providers can make their billing smoother. This improves their financial stability and efficiency.
In conclusion, understanding and accurately using ICD-10 codes is vital in healthcare. It affects the financial side of healthcare and plays a big role in patient care and health data management.
Specific ICD-10 Codes for Diverticulitis
Knowing the ICD-10 codes for diverticulitis is key for correct diagnosis and billing. This condition, where the colon’s wall gets inflamed, needs precise coding. This shows the condition’s severity and details.
Diverticulitis of the Colon
Diverticulitis of the colon gets different codes based on complications. For example, K57.32 is for diverticulitis in the large intestine without perforation or abscess and without bleeding. This code is for cases where the diverticulitis is just in the colon and doesn’t have severe complications.
Diverticulitis with Complications
When diverticulitis has complications, different codes are used. For instance, if there’s a perforation or abscess, the code changes to show the severity. K57.33 might be used for cases with specific complications. This shows how important it is to document accurately for treatment and billing.
Unspecified Diverticulitis
When the details of diverticulitis are not clear, K57.92 might be used. This code is for diverticulitis of the intestine, unspecified part, without perforation or abscess and without bleeding. It’s used when the exact location or complications of the diverticulitis are not detailed.
Accurate coding is vital for healthcare providers. It ensures patients get the right care and billing is correct. By understanding ICD-10 codes for diverticulitis, we can better patient outcomes and healthcare services’ efficiency.
Diagnosis of Diverticulitis
Diagnosing diverticulitis involves several steps. These include clinical evaluation, lab tests, and imaging like CT scans. We’ll dive into these steps and the importance of imaging.
Diagnostic Procedures
The first step is a clinical evaluation. This includes a detailed medical history and physical exam. Doctors look for signs like abdominal pain, fever, and changes in bowel habits.
Labs also play a key role. Tests like complete blood counts (CBC) and blood chemistry tests help gauge the severity. They also help rule out other causes of pain.
Role of Imaging Techniques
Imaging is vital in diagnosing diverticulitis. Computed Tomography (CT) scans are the top choice. They can clearly show inflamed diverticula and how widespread the disease is.
Other methods like ultrasound and MRI are also used. But CT scans are usually the first choice because of their accuracy.
Diagnostic Method | Description | Role in Diagnosing Diverticulitis |
Clinical Evaluation | Includes medical history and physical examination | Identifies symptoms and initial assessment |
Laboratory Tests | CBC, blood chemistry tests | Assesses severity and rules out other conditions |
CT Scans | Imaging technique using X-rays to create detailed images | Confirms diagnosis, assesses disease extent |
Ultrasound/MRI | Alternative imaging techniques | Used in specific cases or patient populations |
Treatment Options for Diverticulitis
Understanding how to manage diverticulitis is key. The right treatment depends on how severe it is, if there are complications, and the patient’s health.
Medical Management
For mild cases, doctors often start with antibiotics. Patients are told to rest and sometimes need to stay in the hospital to manage symptoms and prevent complications. The ICD-10 code for diverticulitis of the small intestine without perforation or abscess is K57.20, and with perforation or abscess is K57.21.
Surgical Interventions
When it’s more serious or complications happen, surgery might be needed. Surgery can remove the affected part of the intestine. The decision to have surgery is made when there are signs of severe diverticulitis, like a lot of bleeding, abscesses, or peritonitis.
Dietary Recommendations
Changing your diet is also important in managing diverticulitis. During an acute episode, a liquid diet can help rest the bowel. After symptoms get better, moving to a high-fiber diet can help prevent future episodes. It’s also good to avoid foods that can irritate the digestive tract, like seeds, nuts, and popcorn.
Treatment Approach | Description | Indications |
Medical Management | Use of antibiotics, rest, and possible hospitalization | Mild diverticulitis |
Surgical Intervention | Removal of the affected portion of the intestine | Severe diverticulitis, significant bleeding, abscesses, or peritonitis |
Dietary Changes | Liquid diet during acute episodes, followed by a high-fiber diet | All cases, to manage symptoms and prevent recurrence |
Complications of Diverticulitis
It’s important to know about the possible complications of diverticulitis. This condition, where the colon’s diverticula get inflamed, can cause serious issues if not treated right. Knowing these complications helps doctors give better care to their patients.
Acute vs. Chronic Complications
Acute problems include perforation, abscesses, and bleeding. These need quick medical help because they can be very dangerous. Chronic issues might mean more diverticulitis attacks, harming the colon over time. Correctly coding these issues, like using the right ICD-10 code for perforation or abscess, is key for billing and insurance.
For example, a perforation might need emergency surgery, while an abscess might need drainage. The right codes help with billing and guide treatment and patient records.
Prevention Strategies
Stopping complications is a big part of managing diverticulitis. This can mean eating more fiber and taking medicines to control symptoms. Being proactive in managing diverticulitis can greatly lower the chance of complications. As one expert says,
‘a high-fiber diet is key in stopping diverticulitis complications.’
By knowing the possible problems and taking steps to avoid them, doctors can help patients get better and lower the risk of serious issues.
How to Properly Code Diverticulitis
Coding diverticulitis correctly is key in healthcare. It affects many areas of care. We’ll show you how to pick the right ICD-10 code and avoid common errors.
Guidelines for Coding
For coding diverticulitis, always check the ICD-10 coding manual. The right code depends on the diagnosis and details. Accurate documentation is key for the correct code.
- Identify the specific type of diverticulitis diagnosed.
- Check for any complications or associated conditions.
- Use the latest version of the ICD-10 coding manual.
Common Mistakes to Avoid
Healthcare providers often face coding challenges with diverticulitis. Mistakes include unspecified coding and not updating codes with new ICD-10 changes. To avoid these, stay current with coding rules and review patient records carefully.
The Role of Healthcare Providers in Coding
Healthcare providers are key to accurate coding. They must document patient info correctly. This is vital for using the right ICD-10 codes, like those in the K57 series for diverticular disease.
Importance of Accurate Documentation
Accurate documentation is essential for correct coding. Clinical documentation code accuracy affects how diverticular disease is coded. Healthcare providers need to understand the importance of detailed and precise documentation to prevent coding mistakes.
Ongoing Education on Coding Updates
The world of medical coding is always changing. “Staying current with coding guidelines is not just a necessity; it’s a responsibility,” say coding experts. It’s important for healthcare providers to keep learning about the latest coding updates, including changes to the K57 series classification.
Here’s why accurate coding matters: “Accurate coding is not just about following rules; it’s about showing patient care accurately in medical records.” This shows how important it is for healthcare providers to code diverticular disease correctly.
Real-World Applications of the ICD-10 Code
Using ICD-10 codes for diverticulitis is key in real-world medicine. It affects how patients are diagnosed, treated, and billed. We’ll look at how these codes work in real situations, including case studies and their effect on insurance and billing.
Case Studies Involving Diverticulitis
Let’s look at some case studies that show why accurate ICD-10 coding for diverticulitis matters. For example, a patient with diverticulitis of the sigmoid colon without abscess gets a different code than one with an abscess.
Case Study 1: A 55-year-old patient had symptoms of diverticulitis. After tests, they were found to have diverticulitis of the sigmoid colon without abscess. The right ICD-10 code was used, making sure billing and insurance went smoothly.
- The patient got treatment like antibiotics and diet changes.
- They had follow-up visits to check on their health.
Case Study 2: A 65-year-old patient had diverticulitis and an abscess. The ICD-10 code for the complication was used, changing their treatment and billing.
- The patient needed hospital care for antibiotics and possibly draining the abscess.
- They might need surgery because of how serious it was.
Impact on Insurance and Billing
Using the right ICD-10 codes for diverticulitis really matters for insurance claims and billing. Correct coding helps healthcare providers get paid right for their work.
Condition | ICD-10 Code | Billing Impact |
Diverticulitis without abscess | K57.92 | Standard billing for medical management |
Diverticulitis with abscess | K57.80 | Increased billing due to complication |
Unspecified diverticulitis | K57.90 | Billing may be delayed pending further diagnosis |
By using the correct ICD-10 code for diverticulitis, healthcare providers make sure patient records are right. This makes billing smoother and cuts down on insurance claim denials.
Resources for Further Information
To keep up with the latest coding for diverticulitis, healthcare providers have many resources. It’s important to use the right ICD-10 code, like K57, for billing and records.
Professional Organizations
Groups like the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC) are great. They offer guidelines, training, and certifications. These help ensure you follow the rules for coding diverticulitis.
Online Coding Manuals and Forums
Places like the Centers for Medicare and Medicaid Services (CMS) and the World Health Organization (WHO) websites are full of useful info. They have coding manuals, updates, and forums. These help with questions and make sure you’re coding correctly for diverticulitis.
Using these resources can improve your coding skills. This ensures your records are accurate and you follow the guidelines.
FAQ
What is diverticulitis and how is it diagnosed?
Diverticulitis is when small pouches in the intestine wall get inflamed. Doctors use a mix of clinical checks, CT scans, and sometimes endoscopy to diagnose it.
What is the ICD-10 code K57.92 used for?
The ICD-10 code K57.92 is for diverticulitis cases without perforation, abscess, or bleeding.
Why is accurate ICD-10 coding important for diverticulitis?
It ensures doctors get paid right and patient data is correct. This is key for billing and tracking health trends.
What are the symptoms of diverticulitis?
Symptoms can be mild or severe. They include stomach pain, changes in bowel habits, and fever.
How is diverticulitis treated?
Treatment includes antibiotics, surgery for serious cases, and diet changes to manage symptoms and prevent future problems.
What are the risk factors for developing diverticulitis?
Risk factors include age, diet, and lifestyle. A low-fiber diet, being overweight, and not being active can increase risk.
Can diverticulitis lead to complications?
Yes, it can cause serious problems like perforation, abscesses, and bleeding. Knowing these risks helps manage the condition better.
How can healthcare providers ensure accurate coding for diverticulitis?
Providers can keep accurate records, stay updated on coding rules, and take part in coding education.
What resources are available for learning more about ICD-10 coding for diverticulitis?
Resources include the American Health Information Management Association (AHIMA) and online coding guides. They offer updates and help with coding.
What is the difference between acute and chronic complications of diverticulitis?
Acute complications happen suddenly, like perforation or abscesses. Chronic complications are ongoing, like recurring diverticulitis or bowel changes.
How does accurate coding impact insurance and billing for diverticulitis treatment?
Accurate coding helps claims get processed right, avoiding delays in payment. This is important for healthcare providers’ financial health.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/nchs/data/icd/10cmguidelines-FY2025.pdf