Inflammatory conditions, like imaging osteomyelitis, are hard to diagnose right. Did you know wrong or late diagnosis can cause a lot of harm? It can lead to long-term suffering and higher healthcare costs. Studies show that quick and accurate diagnosis is key for good treatment.Finding the best scan for inflammation can really help in making a correct diagnosis. There are many imaging techniques out there, each with its own good points and bad points. It’s important for doctors and patients to know about these options.
Key Takeaways
- Accurate diagnosis is critical for effective treatment of inflammatory conditions.
- The best scan for inflammation can vary depending on the specific condition and patient needs.
- Understanding different imaging techniques is essential for diagnostic accuracy.
- Timely diagnosis can reduce healthcare costs and improve patient outcomes.
- A comprehensive guide to imaging osteomyelitis and other inflammatory conditions can aid in diagnosis.
Understanding Inflammation and the Need for Medical Imaging

Inflammation is a body response to harm, like infections or injuries. It’s a complex process that needs a detailed diagnosis. Advanced medical imaging often plays a key role in this.
The Pathophysiology of Inflammation
Inflammation involves many cellular and molecular actions. It brings blood to the affected area, causing redness, heat, swelling, pain, and sometimes loss of function. Medical imaging is key in seeing these changes, helping to understand how severe the inflammation is.
Acute vs. Chronic Inflammatory Processes
Inflammation can be acute or chronic. Acute inflammation is a quick response to injury or infection, usually resolving once the threat is gone. Chronic inflammation lasts longer and can cause diseases like osteomyelitis. Knowing the difference is vital for the right diagnosis and treatment.
| Characteristics | Acute Inflammation | Chronic Inflammation |
| Duration | Short-term | Long-term |
| Causes | Infection, injury | Persistent infection, autoimmune diseases |
| Outcome | Resolution, sometimes fibrosis | Tissue damage, disease progression |
Why Imaging is Essential for Diagnosis and Treatment Planning
Medical imaging is critical for diagnosing inflammatory conditions. X-ray, CT, MRI, and nuclear medicine scans offer insights into inflammation’s extent and severity. In osteomyelitis, for example, imaging shows how the infection spreads to bone and tissues, helping in treatment planning.
Understanding inflammation and using the right imaging helps doctors create effective treatment plans. This improves patient outcomes significantly.
Key Factors in Selecting the Appropriate Inflammatory Imaging Technique

Choosing the right imaging modality is complex. It involves many factors. These factors help in diagnosing inflammatory conditions accurately.
Patient-Specific Considerations
When picking an imaging technique, patient-specific factors are key. These include:
- Age and Comorbidities: Some imaging modalities are better for certain ages or health conditions.
- Medical History: A patient’s past health can affect the imaging choice, like avoiding certain agents or radiation.
- Physical Condition: The patient’s physical state, like implants or claustrophobia, can also influence the choice.
For example, MRI is often chosen for soft tissue inflammation. CT scans are better for detailed bone images.
Clinical Factors Influencing Scan Selection
Clinical factors are also important in choosing the right imaging technique. These include:
- Symptom Duration and Severity: Acute versus chronic inflammation may need different imaging approaches.
- Suspected Inflammatory Condition: Different conditions, like osteomyelitis or vasculitis, may require specific imaging modalities.
- Previous Diagnostic Results: Past imaging results can help choose the next imaging technique.
A leading radiologist notes, “The choice of imaging modality should be tailored to the individual patient’s clinical presentation and medical history.”
“Imaging plays a critical role in the diagnosis and management of inflammatory conditions. The selection of the appropriate imaging technique is critical for accurate diagnosis and effective treatment planning.”
” Expert in Radiology
Practical Considerations
Practical considerations also affect the choice of imaging technique. These include:
- Availability and Accessibility: The availability of imaging modalities can vary between institutions.
- Cost and Insurance Coverage: The cost of imaging techniques and insurance coverage can impact the choice of modality.
- Radiation Exposure: Concerns about radiation exposure, like in pediatric or pregnant patients, can influence the selection of imaging techniques.
In conclusion, selecting the right imaging technique for inflammatory conditions is complex. It involves considering patient-specific, clinical, and practical factors. By carefully evaluating these factors, healthcare providers can choose the most effective imaging modality for accurate diagnosis and treatment planning.
Imaging Osteomyelitis: Techniques and Diagnostic Approach
Getting a correct diagnosis of osteomyelitis depends on the right imaging studies. This bone infection is complex and can be very serious. A detailed diagnostic approach is needed to treat it well.
Pathophysiology of Bone Infection
Osteomyelitis is when the bone gets inflamed due to infection. Pathogens invade the bone, causing inflammation. This can lead to bone damage and death. Knowing this helps in understanding imaging results.
Distinguishing Features of Acute vs. Chronic Osteomyelitis
Acute osteomyelitis starts suddenly with pain, swelling, and fever. Early signs on imaging include soft tissue swelling and periosteal reaction. Chronic osteomyelitis has ongoing infection, often after failed treatments. It shows bone deformity, sequestra, and sinus tracts on imaging.
Key differences between acute and chronic osteomyelitis include:
- Duration of symptoms
- Presence of bone deformity or sequestra
- Evidence of previous infections or treatments
Multi-Modality Imaging Approach for Accurate Diagnosis
Using multiple imaging methods is key to diagnosing osteomyelitis. This includes X-rays, CT scans, MRI, and nuclear medicine. Each method has its own benefits and drawbacks. The choice depends on the patient’s situation and the suspected osteomyelitis stage.
The advantages of a multi-modality approach include:
- Comprehensive assessment of bone and soft tissue
- Improved diagnostic accuracy
- Guidance for treatment planning
By combining different imaging methods, doctors can better understand the bone infection. This leads to better treatment and outcomes for patients.
X-ray Radiography: The First-Line Imaging for Osteomyelitis
X-ray radiography is the first choice for diagnosing osteomyelitis. It gives quick insights into bone health. X-rays are easy to get and show bone structure well.
X-rays help spot changes in bone density and shape. Typical radiographic findings in osteomyelitis include lytic lesions, sclerosis, and periosteal reaction.
Typical Radiographic Findings in Early and Late Osteomyelitis
In early osteomyelitis, X-rays might not show much. But as the disease gets worse, X-rays show clear signs. These include:
- Soft tissue swelling
- Periosteal elevation and new bone formation
- Lytic areas within the bone
- Sclerosis and bone remodeling
Limitations of X-ray in Detecting Early Bone Infection
X-rays have big limits in catching early osteomyelitis. It can take 10-14 days to see changes on X-rays. Early osteomyelitis might not show up on X-rays at all.
This shows we need a full plan to diagnose osteomyelitis. We might need to use MRI or CT scans too for better results.
Computed Tomography (CT) for Detailed Bone Assessment
Computed Tomography (CT) scans are key for checking bone infections, like osteomyelitis. They give clear images of bones, helping doctors spot and treat osteomyelitis better.
Advantages of CT in osteomyelitis evaluation
CT scans are great for seeing bone damage and small bone pieces that X-rays can’t. They are very good at finding small bone fragments and calcifications. A study in a Journal found CT scans catch osteomyelitis early, leading to quicker treatment.
CT protocols for optimal inflammation imaging
For the best CT scans, special steps are taken. Thin slices (0.5-1 mm) and contrast are used to see soft tissues better. The right algorithm is key for clear bone images.
Limitations and radiation concerns
But, CT scans have downsides. They use radiation, which is a big worry for kids and those needing many scans. “The risk of radiation-induced complications should be carefully weighed against the benefits of CT scanning,” experts say. Also, CT scans might not show soft tissues as well as MRI, so more tests might be needed.
In summary, CT scans are a valuable tool for diagnosing and treating osteomyelitis. They give detailed bone images that help doctors make better choices.
MRI: The Gold Standard for Imaging Osteomyelitis
MRI is seen as the top choice for seeing osteomyelitis. It shows the full extent of bone and soft tissue problems. This is key for making the right diagnosis and treatment plan.
Why MRI Excels at Bone Marrow and Soft Tissue Evaluation
MRI is great at showing bone marrow and soft tissues. It can spot early signs of osteomyelitis. It’s also good at finding soft tissue infections or abscesses.
Using MRI sequences like STIR and fat-suppressed T2-weighted images helps a lot. These make marrow edema and soft tissue inflammation stand out. They’re great for catching osteomyelitis early.
Optimal MRI Sequences for Osteomyelitis
There are several MRI sequences used for osteomyelitis. Each gives different information:
- T1-weighted images: Good for looking at bone marrow and finding marrow replacement.
- STIR sequences: Spot marrow edema and soft tissue inflammation well.
- Fat-suppressed T2-weighted images: Show inflammation and edema clearly.
- Post-contrast T1-weighted images: Find abscesses and areas of necrosis.
Interpreting MRI Findings in Acute and Chronic Osteomyelitis
Understanding MRI results for osteomyelitis is important. Acute osteomyelitis shows marrow edema, swelling, and abscesses. Chronic osteomyelitis has bone deformity, sequestra, and sinus tracts.
Getting these findings right is key for treatment. It helps decide if surgery or long-term antibiotics are needed.
Limitations and Contraindications
Even though MRI is powerful, it has its downsides. People with metal implants or pacemakers can’t have it. It’s also not always easy to get and can be expensive.
Despite these issues, MRI is the best choice for osteomyelitis. It offers detailed views and is very accurate.
Nuclear Medicine Techniques in Inflammation Imaging
Nuclear medicine is key in finding inflammatory conditions. It uses advanced imaging to show where and how severe the inflammation is. This helps doctors diagnose and plan treatments.
Three-phase bone scintigraphy
Three-phase bone scintigraphy uses Technetium-99m methylene diphosphonate (Technetium-99m MDP) to check bone health. It’s great for spotting bone infections like osteomyelitis.
The scan has three parts:
- The first part looks at blood flow.
- The second part checks how the tracer spreads in soft tissues.
- The third part shows how bones take up the tracer.
This method makes the scan better at finding bone diseases.
Gallium-67 citrate scanning
Gallium-67 citrate scanning helps find inflammation and infections. Gallium-67 sticks to proteins in inflammatory cells.
This scan is good for finding long-term infections and inflammation, not just in bones.
Techniques like three-phase bone scintigraphy and Gallium-67 citrate scanning are powerful tools. They give detailed information about inflammation. This helps doctors make more accurate diagnoses.
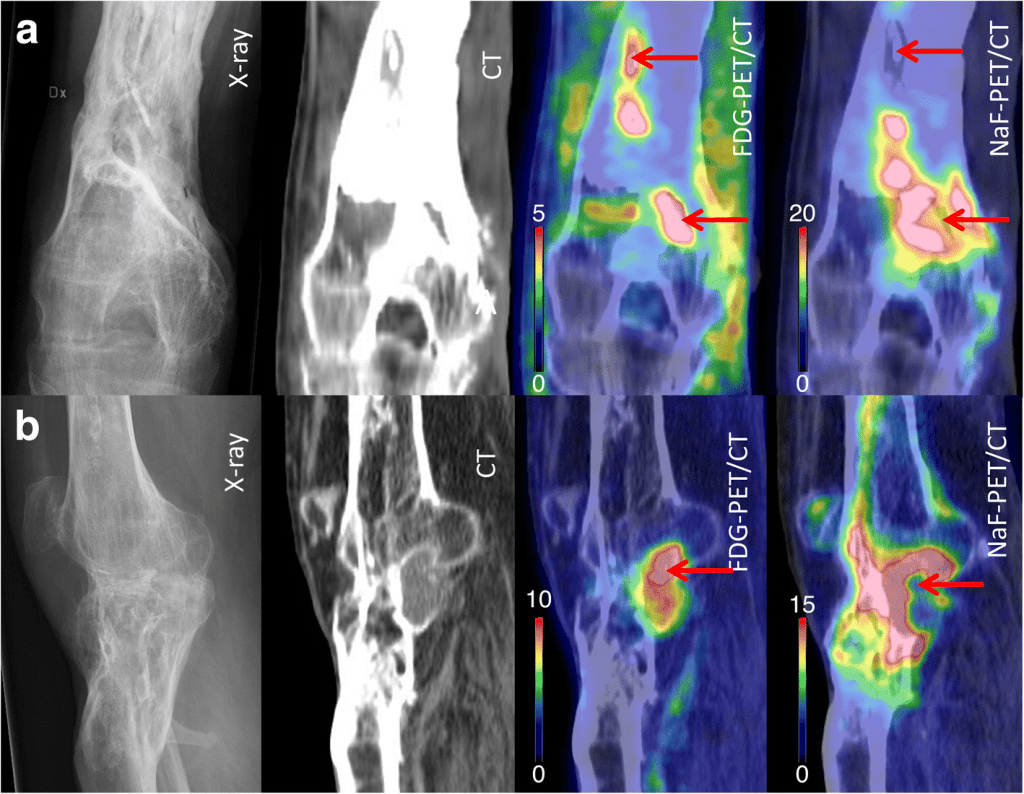
PET and PET/CT: Advanced Functional Imaging for Inflammation
PET and PET/CT imaging are key in understanding inflammation. They give deep insights into how inflammation works. This helps doctors plan better treatments.
FDG-PET Mechanisms in Infection Detection
FDG-PET uses glucose to find infections. FDG is taken up by active inflammatory cells like macrophages and neutrophils. This shows where inflammation is happening.
FDG gets trapped in cells because of a chemical reaction. How much FDG is taken up shows how severe the inflammation is.
PET/CT Fusion Advantages in Osteomyelitis
PET/CT scanners are great for looking at osteomyelitis. PET/CT combines PET’s function with CT’s anatomy. This helps pinpoint where inflammation is in bones and soft tissues.
This combo makes diagnosing osteomyelitis more accurate. It shows both the metabolic activity and structural changes.
Quantitative Assessment Using SUV Values
PET imaging lets us measure inflammation with SUV values. SUV values show how much FDG is taken up. This helps see how severe the inflammation is and if treatment is working.
SUV values help compare inflammation levels in different areas or over time. This is useful for planning treatments.
Comparing FDG-PET to Conventional Nuclear Medicine Studies
FDG-PET has many benefits over older imaging methods. It has better resolution and can measure metabolic activity. FDG-PET gives more precise and detailed info on inflammation.
FDG-PET is very sensitive and specific. It’s a powerful tool for diagnosing and managing complex inflammatory conditions. It might even cut down on the need for more tests.
Ultrasound Applications in Soft Tissue Inflammation
Ultrasound technology is a key tool for checking soft tissue inflammation. It’s non-invasive and works well for diagnosing issues. Its real-time images are great for watching how things move and helping with treatments.
Role in Detecting Periosteal Reactions and Subperiosteal Abscesses
Ultrasound is key in spotting periosteal reactions and subperiosteal abscesses. These are linked to osteomyelitis. It shows the periosteum and finds signs of infection or swelling. High-resolution ultrasound finds abscesses, helping to treat osteomyelitis right.
Power Doppler Assessment of Inflammatory Hyperemia
Power Doppler ultrasound is great for looking at blood flow in inflammation. It shows how much blood is moving to the area. Increased vascularity means inflammation is active. It helps see how treatments are working.
Ultrasound-Guided Procedures in Osteomyelitis Management
Ultrasound helps a lot with osteomyelitis treatments like draining abscesses. It makes sure the right spot is hit, lowering risks and making tests more accurate. Ultrasound-guided interventions are key for getting to abscesses or fluid for tests or treatment.
| Ultrasound Application | Benefits | Clinical Utility |
| Detecting Periosteal Reactions | Non-invasive, real-time imaging | Early detection of osteomyelitis |
| Power Doppler Assessment | Quantifies inflammatory hyperemia | Monitoring treatment response |
| Guiding Interventions | Precise targeting, reduced complications | Effective management of osteomyelitis |
MRI vs. PET Inflammation Imaging: Comparative Analysis
MRI and PET are two ways to see inflammation, each with its own strengths and weaknesses. Knowing what each can do helps pick the best tool for diagnosing.
Anatomical vs. Functional Information
MRI gives detailed pictures of soft tissues, showing changes in inflammation. PET, on the other hand, shows where inflammation is active by looking at metabolism. This is key for catching inflammation early, before it shows up in pictures.
MRI is great for looking at detailed anatomy, like in joints or soft tissues. PET is better for seeing how active inflammation is, helping diagnose things like vasculitis or infection.
Cost-Effectiveness Analysis
Cost is a big factor when choosing MRI or PET for looking at inflammation. MRI is cheaper and more common than PET, which is more expensive and less available. But, the cost must be balanced against how well it works and how it helps in treating the patient.
Looking at the whole picture, not just the first cost, is important. For example, PET might save money by catching problems early, avoiding more tests later.
Radiation Exposure Considerations
MRI doesn’t use harmful radiation, making it safer for patients needing many scans or kids. PET, on the other hand, uses radiation from a tracer.
The radiation from PET is a big deal, mainly for kids or when many scans are needed. We must think about the benefits of PET against the risks of radiation.
Availability and Accessibility Factors
MRI is easy to find in most hospitals, but PET is less common because it’s more expensive and needs special equipment. This makes MRI a better choice in many places.
Accessibility matters a lot, too. In places where PET isn’t available, MRI is often a better option for looking at inflammation.
Pediatric Considerations in Imaging Osteomyelitis
Choosing the right imaging method for pediatric osteomyelitis is very important. This is because kids are more sensitive to radiation and need accurate diagnoses. Osteomyelitis in children can show up differently than in adults, so we need a special approach to imaging.
Unique Aspects of Pediatric Bone Infections
Pediatric bone infections have their own special features. Kids’ bones are growing, and their immune systems are just starting to develop. This can change how osteomyelitis shows up and grows.
Key differences in pediatric osteomyelitis:
- Hematogenous spread is more common in children.
- The presence of growth plates can complicate diagnosis and treatment.
- Children’s bones are more vascular, potentially altering imaging findings.
Growth Plate Considerations
The growth plate, or physis, is a key area in kids’ bones where they grow. We must pick imaging methods carefully to avoid harming this area. At the same time, we need to get accurate diagnostic info.
Growth plate considerations include:
- Avoiding radiation when possible to prevent damage to the growth plate.
- Using MRI, which is highly sensitive for assessing the growth plate and surrounding bone marrow.
Hematogenous Osteomyelitis Imaging Patterns
Hematogenous osteomyelitis is a common issue in kids, where the infection comes from the blood. Imaging is key in showing how big and serious the infection is.
Typical imaging findings include:
- Early changes detectable on MRI, such as bone marrow edema.
- Ultrasound can be useful for detecting subperiosteal abscesses.
- CT scans may be used in certain cases to assess bone destruction.
Specialized Imaging for Vasculitis and Vascular Inflammation
Imaging is key in diagnosing vasculitis, a condition that affects blood vessels. The right imaging method depends on the type of vasculitis, the size of the vessels, and how much inflammation there is.
Large Vessel Vasculitis Assessment
Large vessel vasculitis, like giant cell arteritis and Takayasu arteritis, needs imaging that can see the aorta and its big branches well. PET/CT is a great tool here, giving both functional and anatomical details.
FDG-PET shows inflammation in the vessel walls, while CT gives detailed anatomy. Together, they’re great for diagnosing and tracking large vessel vasculitis.
Medium and Small Vessel Vasculitis Imaging
For medium and small vessel vasculitis, like polyarteritis nodosa and ANCA-associated vasculitis, MRI and ultrasound are very helpful. They can spot inflammation and damage in smaller vessels.
Ultrasound checks vascular flow and finds aneurysms, which is good for medium vessel vasculitis. MRI, with its detailed soft tissue images, spots inflammation well.
Role of Angiography vs. Cross-Sectional Imaging
Conventional angiography has been the top choice for vascular problems. But cross-sectional imaging like CT and MRI angiography are getting more use. They’re non-invasive and show both the vessel lumen and wall well.
Angiography is great for seeing the vascular lumen. But cross-sectional imaging looks at the vessel wall and surrounding tissues too.
PET/CT Applications in Vasculitis
PET/CT is very useful for large vessel vasculitis. It spots inflammation early and tracks treatment response. The FDG uptake measure gives a clear view of inflammation.
PET and CT together give a precise diagnosis and help figure out how widespread vasculitis is. This guides treatment plans.
Sarcoidosis Imaging: Multi-System Inflammatory Assessment
Imaging is key in managing sarcoidosis, a disease that affects many parts of the body. It helps doctors diagnose and understand how widespread the disease is. This is important for planning the right treatment.
Chest Imaging in Pulmonary Sarcoidosis
Pulmonary sarcoidosis is a common form of the disease. Chest imaging is vital for checking it. High-resolution computed tomography (HRCT) is great for looking at the lungs. It can spot signs like micronodules and lymphadenopathy.
| Imaging Modality | Key Features in Pulmonary Sarcoidosis |
| Chest X-ray | Initial assessment, lymphadenopathy |
| HRCT | Detailed lung assessment, micronodules, fibrosis |
| PET/CT | Metabolic activity assessment, inflammation detection |
Cardiac Sarcoidosis Detection Challenges
Cardiac sarcoidosis is hard to diagnose because symptoms are not clear and imaging has its limits. Cardiac MRI is now a top choice for spotting heart problems. It gives detailed views of the heart’s shape and how it works.
Neurosarcoidosis Imaging Approaches
Neurosarcoidosis can hit any part of the brain and spinal cord. Imaging is key for finding out. MRI is best for seeing lesions and inflammation in the brain and spinal cord.
Managing sarcoidosis needs a mix of imaging methods to see how it affects different parts of the body. Using various imaging tools, doctors can get a full picture of the disease. This helps them make better treatment plans.
Cardiac Inflammation Imaging Techniques
Imaging is key in spotting and handling cardiac inflammation. Many tests are used to check and keep track of heart inflammation.
MRI Protocols for Myocarditis
Magnetic Resonance Imaging (MRI) is great for finding myocarditis. This is when the heart muscle gets inflamed. Special MRI plans are used to see how bad the heart muscle damage is.
- MRI Sequences: T2-weighted images spot heart muscle swelling. Late gadolinium enhancement (LGE) sequences show fibrosis and scarring.
- Protocol Optimization: Changing MRI plans to include T1 and T2 mapping gives exact data on heart inflammation and scarring.
PET Imaging for Cardiac Inflammation
Positron Emission Tomography (PET) imaging is also key for heart inflammation. It shows how active the heart tissue is.
- FDG-PET: Fluorodeoxyglucose (FDG) PET checks the heart’s metabolic activity of inflammatory cells.
- Hybrid Imaging: Mixing PET with CT or MRI gives better results by showing both how the heart works and its structure.
Echocardiography in Inflammatory Heart Disease
Echocardiography is a common and safe test for checking the heart’s function and shape in inflammatory heart disease.
- Functional Assessment: Echocardiography looks at the left ventricle’s function and finds issues like pericardial effusion.
- Limitations: Echocardiography is good for first checks but doesn’t show detailed inflammation or scarring.
Combined Imaging Approaches for Complex Cases
For hard cases of heart inflammation, using more than one imaging method is best. This mix of methods gives a full picture of the condition.
| Imaging Modality | Strengths | Limitations |
| MRI | Shows detailed tissue, finds fibrosis and edema | Not for all patients, expensive |
| PET | Checks metabolic activity, works with other images | Uses radiation, pricey |
| Echocardiography | Easy to get, non-invasive, checks function | Doesn’t show inflammation or scarring well |
Inflammatory Bowel Disease: Optimal Imaging Strategies
Imaging is key in managing inflammatory bowel disease (IBD). It helps doctors decide on treatments. Different imaging methods are used, each with its own strengths and uses.
CT Enterography Techniques and Findings
CT enterography gives detailed views of the small bowel. It uses contrast agents to make the bowel stand out. This helps spot thickened walls, hyperenhancement, and issues like strictures and fistulae.
CT enterography is vital for IBD checks, showing disease activity and complications. But, it’s important to consider the radiation risks, mainly for young patients needing many scans.
MR Enterography Advantages in IBD
MR enterography is great for IBD imaging because it doesn’t use harmful radiation. It’s perfect for those needing many scans or are sensitive to radiation, like kids and young adults.
It’s good at showing disease activity, extent, and complications. MR enterography looks at the bowel and surrounding areas, making it a top choice for IBD checks.
Ultrasound Applications in Crohn’s Disease
Ultrasound is useful for Crohn’s disease. It checks bowel wall thickness, strictures, and complications like abscesses. Doppler ultrasound helps see how active the disease is by looking at blood flow.
Ultrasound is non-invasive, doesn’t use radiation, and is easy to find. It’s great for first checks and follow-ups in Crohn’s patients.
Nuclear Medicine Approaches for IBD Activity Assessment
Nuclear medicine, like PET/CT, helps measure IBD activity. It uses special drugs that light up where inflammation is. This lets doctors see how active the disease is.
While not the first choice, nuclear medicine is useful in tough cases or when checking treatment results. It adds a functional view to the anatomical details from other scans.
Conclusion: Selecting the Right Inflammatory Imaging Modality
Choosing the right imaging method is key for diagnosing and treating inflammatory conditions. This guide has covered many imaging options. These include X-ray, CT scans, MRI, nuclear medicine, and ultrasound.
Each method has its own benefits and drawbacks. The right choice depends on the patient, the condition, and practical factors. For example, MRI is top for seeing osteomyelitis because it shows bone and soft tissue well.
In summary, knowing about different imaging methods is vital for doctors. By picking the best one, they can improve diagnosis and treatment. This leads to better care for patients.
FAQ
What is the best imaging technique for diagnosing osteomyelitis?
MRI is the top choice for spotting osteomyelitis because it checks bone marrow and soft tissue well. But, the right imaging method also depends on the disease stage, the patient, and the situation.
How does PET/CT compare to MRI in inflammation imaging?
PET/CT shows how active inflammation is, while MRI gives detailed views of anatomy. PET/CT is great for finding active inflammation. MRI is better for soft tissue and bone marrow details.
What is the role of ultrasound in diagnosing inflammatory conditions?
Ultrasound is good for seeing soft tissue inflammation and guiding procedures. It also helps spot inflammation by using Power Doppler.
Can X-ray detect early osteomyelitis?
X-rays can miss early bone infections, as changes might not show up for 10-14 days. Yet, it’s a good first step for checking.
How is vasculitis diagnosed using imaging techniques?
To spot vasculitis, doctors use PET/CT, MRI, and CT angiography. The best method depends on the vessel size and the situation.
What imaging strategies are used for inflammatory bowel disease?
For inflammatory bowel disease, doctors use CT enterography, MR enterography, ultrasound, and nuclear medicine. The choice depends on the question and the patient.
How is cardiac inflammation imaged?
Cardiac inflammation is seen with MRI, PET, and echocardiography. MRI is key for myocarditis. PET is good for inflammation. Echocardiography checks heart function and signs of disease.
What are the advantages of using labeled WBC scans for infection imaging?
Labeled WBC scans are very specific for finding infections. They’re great for diagnosing osteomyelitis when other methods don’t work.
Can CT scans detect osteomyelitis?
CT scans can spot osteomyelitis, but they’re better for later stages. MRI is more sensitive for early signs.
How is sarcoidosis assessed using imaging techniques?
Sarcoidosis is checked with chest imaging for lung issues, cardiac MRI or PET for heart problems, and MRI or CT for brain issues.
References
- Lee, Y. J., et al. (2016). The imaging of osteomyelitis. Insights into Imaging, 7(2), 265-274. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4858469/
- Taş, F., et al. (2005). Comparison of MRI, ultrasonography and radiography sensitivities in early diagnosis of acute osteomyelitis. European Journal of Radiology, 56(2), 180-185. https://doi.org/10.1016/j.ejrad.2005.02.016
- NIHR. (2022). Imaging for detection of osteomyelitis: A systematic review and assessment of modalities. https://njl-admin.nihr.ac.uk/document/download/2025115










