Last Updated on November 26, 2025 by Bilal Hasdemir

Diagnostic imaging is key in today’s healthcare. It helps doctors see inside the body for correct diagnosis and treatment plans. At Liv Hospital, we use the latest imaging studies for fast and reliable diagnoses.
Accurate diagnosis is vital for good treatment. Diagnostic imaging leads the way in this area. We use the newest clinical diagnostic imaging to give our patients the best care.
Key Takeaways
- Diagnostic imaging is essential for accurate diagnosis and treatment planning.
- Liv Hospital uses state-of-the-art diagnostic imaging technologies.
- Clinical diagnostic imaging enables clinicians to visualize internal structures.
- Accurate diagnosis is vital for effective treatment.
- Diagnostic imaging is a vital part of modern healthcare.
The Critical Role of Diagnostic Imaging in Modern Healthcare

Modern healthcare depends a lot on diagnostic imaging for quick and accurate decisions. It’s key in managing many medical issues. It lets doctors see inside the body in great detail.
Diagnostic medical imaging is vital for better patient care. It lets us see inside the body. This helps find diseases early and treat them fast.
Global Impact on Disease Detection and Management
Diagnostic imaging is key in finding diseases early. This helps lower sickness and death rates. It’s very important worldwide for both long-term and sudden illnesses.
- Early cancer detection with mammograms and CT scans.
- Spotting heart diseases with MRI and CT angiography.
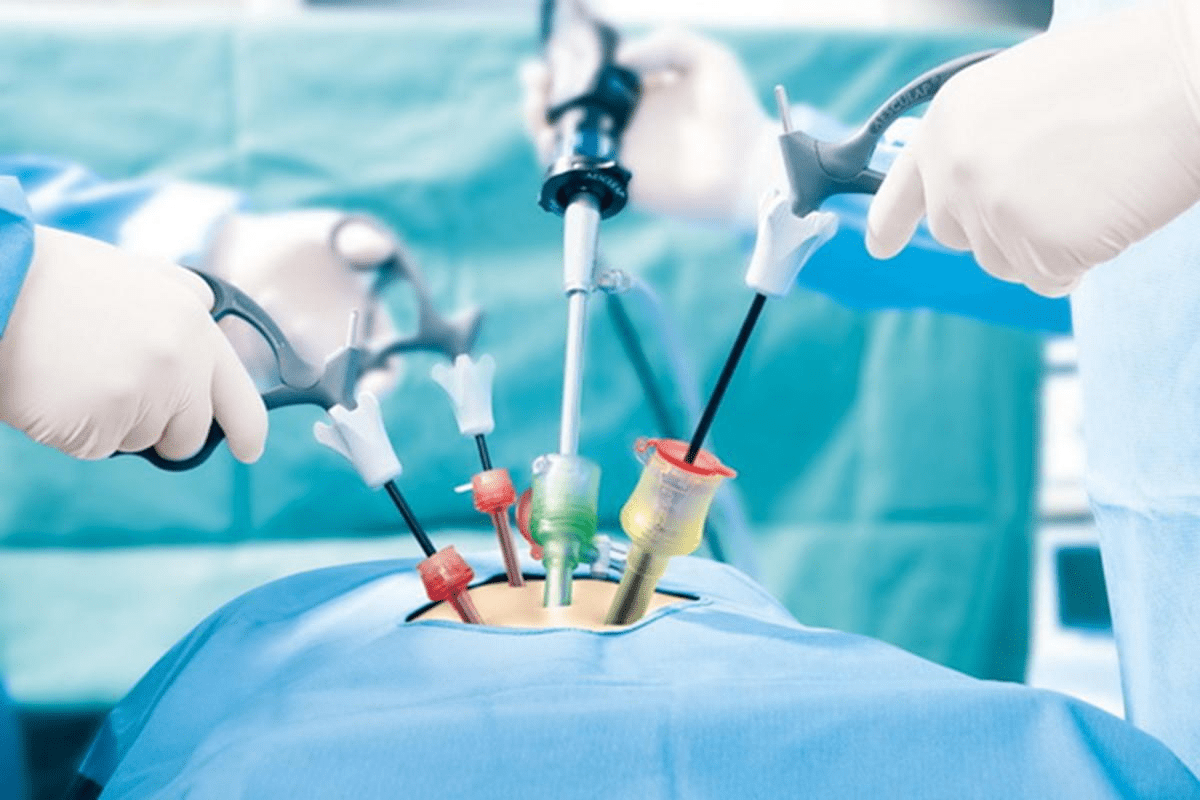
- Helping with less invasive surgeries with fluoroscopy and ultrasound.
New imaging methods are changing how we diagnose and treat. They let us find health problems before they get worse. This makes patients better off.
How Imaging Transforms Clinical Decision-Making
Diagnostic imaging changes how doctors make decisions. It gives them detailed views of a patient’s health. This is key for making good treatment plans.
- It helps know how serious a disease is, which helps choose the right treatment.
- It makes procedures safer and more successful.
- It lets us track how a disease is changing and how well treatments are working.
Imaging helps doctors understand patients better. This is why diagnostic imaging meaning is so important. We use these tools to give our patients the best care.
X-Ray Radiography: Fundamental Imaging Studies for Rapid Assessment

X-Ray Radiography is a key tool in medical imaging. It gives quick and accurate results for many health issues. Over time, it has improved a lot thanks to new technology.
Technical Principles and Image Acquisition
X-Ray Radiography works by showing how different tissues absorb X-rays. This creates contrast to see inside the body. Today’s X-Ray systems use digital radiography. This is better than old film systems because it’s faster, uses less radiation, and has better image quality.
Key technical advancements include:
- Digital detectors that turn X-ray energy into electronic signals for quick image display and processing.
- Image enhancement algorithms that make details clearer.
- Tomosynthesis, which makes three-dimensional images from multiple X-ray exposures.
Primary Clinical Applications and Decision Points
X-Ray Radiography is used for first checks in many cases. This includes injuries, lung problems, and bone issues. It’s very useful in emergencies because it’s fast and always available.
| Clinical Scenario | Primary Use of X-Ray Radiography | Decision Points |
| Trauma | Checking for fractures and dislocations | Presence of fracture, displacement, and possible complications |
| Respiratory Conditions | Looking at lung problems | Pneumonia, effusions, or other issues |
| Musculoskeletal Disorders | Diagnosing bone and joint problems | Osteoarthritis, osteoporosis, or other degenerative changes |
Limitations and Radiation Safety Considerations
Even though X-Ray Radiography is very useful, it has some downsides. It can’t show soft tissues well and there’s a risk of radiation harm. To reduce these risks, doctors follow the ALARA rule. This means they use the least amount of radiation needed for a good diagnosis.
Radiation safety measures include:
- Using shields for patients and staff.
- Adjusting exposure to lower doses.
- Checking equipment regularly to make sure it works right.
Computed Tomography (CT): Cross-Sectional Insights for Urgent Diagnoses
Computed Tomography (CT) scans have changed how we diagnose illnesses. They give us detailed images of the body’s inside. These images are key in emergency and trauma care.
How CT Technology Creates Detailed Anatomical Images
CT scans use X-rays and computers to show the body’s inside. They rotate around the body, capturing data. This data is then turned into detailed images.
These images show organs, bones, and soft tissues clearly. Doctors can spot many conditions, like injuries, infections, cancers, and vascular diseases.
Critical Applications in Emergency and Trauma Care
In emergencies, CT scans are vital. They quickly show the severity of injuries. They help find:
- Internal bleeding
- Fractures
- Organ damage
This fast info lets doctors make quick decisions. It can save lives.
Balancing Diagnostic Benefits with Radiation Exposure
CT scans are great for diagnosing but involve radiation. We must weigh their benefits against the risks. This is true for kids and when scans are needed often.
To lower risks, we follow the ALARA rule. This means keeping doses low. We make sure the benefits of CT scans are worth the risks.
Magnetic Resonance Imaging (MRI): Superior Tissue Characterization
MRI has greatly improved our ability to diagnose and manage complex medical conditions. It provides high-resolution images of soft tissues, making it a key tool in modern medicine.
Non-Ionizing Technology and Multiparametric Capabilities
MRI uses non-ionizing radiation, making it safer than other imaging methods. It can provide detailed tissue characterization without the risks of radiation. We can get images in different planes and contrasts, improving diagnostic accuracy.
Key features of MRI include:
- High soft tissue contrast
- Multiplanar imaging capabilities
- Ability to assess functional and anatomical information
Key Clinical Scenarios and Decision-Making Criteria
MRI is great for diagnosing and monitoring conditions in the central nervous system, musculoskeletal system, and soft tissues. It’s also useful for detecting and characterizing tumors, assessing vascular diseases, and guiding interventions.
| Clinical Scenario | MRI’s Role | Decision-Making Criteria |
| Central Nervous System Disorders | Detailed imaging of brain and spinal cord | Presence of lesions, tumors, or demyelinating diseases |
| Musculoskeletal Injuries | Assessment of soft tissue injuries and joint disorders | Extent of injury, presence of ligament tears or tendonitis |
| Tumor Detection and Characterization | Evaluation of tumor size, location, and characteristics | Tumor staging, planning for biopsy or treatment |
Contraindications and Accessibility Considerations
Despite its benefits, MRI has some limitations. It’s not suitable for patients with certain metal implants, pacemakers, or those with claustrophobia. Accessibility can also be a challenge due to the need for specialized equipment and trained personnel. We must consider these factors when deciding if MRI is right for a patient.
As diagnostic imaging evolves, new techniques like photon-counting CT and artificial intelligence will improve our diagnostic abilities. MRI will continue to play a vital role, providing unique advantages in tissue characterization and diagnostic accuracy.
Ultrasound: Real-Time Visualization for Immediate Clinical Decisions
Ultrasound technology has changed medical imaging a lot. It gives us real-time images for quick decisions. This is great because it doesn’t use harmful radiation, making it safe for many uses.
Principles of Sonography and Recent Advancements
Sonography uses sound waves to see inside the body. Special devices send and get these waves, turning them into clear images. New ultrasound tech has made images better, Doppler more detailed, and devices smaller and easier to use.
The principles of sonography are based on sound waves and how they bounce off tissues. Knowing this helps us get better images. Today’s ultrasound systems also have cool features like harmonic imaging and elastography, giving us more info.
Point-of-Care Applications Across Medical Specialties
Ultrasound is key in many medical fields because it’s flexible and shows images as it happens. It’s used in emergency rooms, for checking on babies during pregnancy, and for heart exams. Its point-of-care applications mean doctors can make quick decisions right at the patient’s side.
Ultrasound is also used for guiding procedures like biopsies and drainages. Its live images make these procedures safer and more accurate. It’s also used in muscle and bone exams to check for injuries and guide injections.
Advantages and Limitations in Clinical Practice
The advantages of ultrasound include being non-invasive, not using harmful radiation, and showing images in real-time. It’s also cheaper than some other imaging methods. These reasons make it a good choice for first checks and follow-ups.
But, ultrasound has limitations too. How well it works depends on the person using it, and some things like being overweight or having gas can make it harder to see. It might not show as much detail as other methods for some problems.
Even with these issues, ultrasound tech keeps getting better. For example, contrast-enhanced ultrasound helps spot and understand lesions better. The future looks bright with ultrasound getting smarter thanks to AI and machine learning.
Fluoroscopy: Dynamic Imaging for Procedural Guidance
Fluoroscopy has greatly improved our ability to see inside the body in real-time. It helps with complex medical procedures. This technology gives continuous X-ray images, helping doctors guide tools through the body.
Real-Time X-Ray Visualization Techniques
Fluoroscopy uses real-time X-ray images for many medical procedures. It offers continuous imaging, which is key for navigating the body’s complex structures. Doctors use a contrast agent to make certain areas, like blood vessels, clearer.
This technology lets doctors make quick changes during procedures. This improves accuracy and lowers the chance of problems. We use it for many interventions, from vascular to orthopedic.
Interventional Applications and Diagnostic Procedures
Fluoroscopy is key for guiding interventional procedures, like angiography and embolization. It’s also used for diagnostic tests, such as barium studies. The dynamic imaging it provides is essential for these tasks, giving insights that static images can’t.
In interventional radiology, fluoroscopy helps place devices and deliver treatments precisely. It’s used in many fields, including cardiology and gastroenterology. It supports both diagnostic and treatment efforts.
Radiation Management and Alternative Approaches
Fluoroscopy is a powerful tool but involves radiation. We manage radiation doses carefully to protect patients and staff. Pulsed fluoroscopy and image collimation help lower radiation exposure.
When possible, we use ultrasound and MRI instead to avoid radiation. But fluoroscopy is often essential due to its unique abilities. We regularly update our methods to balance fluoroscopy’s benefits with radiation safety.
Looking ahead, new fluoroscopy technologies promise better safety and effectiveness. Advances like AI-driven analysis and other innovations will likely increase fluoroscopy’s role in guiding procedures.
Positron Emission Tomography (PET): Metabolic Mapping for Disease Detection
PET scans give us a peek into how our cells work. They spot changes before damage shows up. This helps us find diseases early and plan better treatments.
Principles of Functional Molecular Imaging
PET scans use special drugs that light up where cells are very active. These drugs help us see and measure how cells use energy, like glucose. This is important because diseased cells often use energy differently.
The most used PET drug is Fluorodeoxyglucose (FDG). It acts like glucose and shows up in cancer cells. This lets us find tumors and check if treatments are working.
Hybrid PET/CT and PET/MRI Applications
Hybrid scans like PET/CT and PET/MRI mix PET’s metabolic info with CT or MRI’s body maps. This mix makes diagnoses more accurate by linking energy use to body parts.
PET/CT is great for cancer, helping us see how far it has spread and plan treatments. PET/MRI is better for soft tissues and is used in brain and some cancer cases.
| Imaging Modality | Key Features | Clinical Applications |
| PET/CT | Combines metabolic activity with anatomical detail | Cancer staging, treatment planning, response assessment |
| PET/MRI | Superior soft tissue characterization, reduced radiation | Neurological disorders, certain cancers |
Clinical Decision Support in Oncology and Neurology
In cancer care, PET scans are key for finding and tracking tumors. They help us tell apart tumors from dead tissue or scar tissue.
In brain diseases, like Alzheimer’s, PET scans help us see how brain cells work. This helps us diagnose and plan treatments early.
PET scans give us detailed info on how cells work. This helps us make better treatment plans for each patient.
Nuclear Medicine Imaging: Targeted Physiological Assessment
Nuclear medicine imaging is a top-notch diagnostic tool. It uses radiopharmaceuticals for a detailed look at how our bodies work. This helps us see how different parts of our body function.
Radiopharmaceuticals and Gamma Camera Technology
The heart of nuclear medicine imaging is radiopharmaceuticals. These are special compounds with tiny amounts of radioactive material. They target specific areas in the body, giving us clear images.
When given to a patient, these compounds gather in the needed areas. They then send out gamma rays that a gamma camera picks up. This tech lets us see what’s happening inside our bodies.
Gamma camera technology has gotten much better. Now, we can get detailed images with less radiation. This makes it safer for patients.
Essential Applications in Cardiology and Endocrinology
Nuclear medicine imaging is key in cardiology and endocrinology. It helps check how well the heart works and spots heart disease. It also looks at how well the thyroid gland works.
In cardiology, it’s used to see how blood flows to the heart. This helps doctors decide the best treatment. For thyroid issues, it helps figure out if the gland is working right.
“Nuclear medicine imaging has revolutionized the way we diagnose and manage cardiac and endocrine disorders, giving us deep insights into how our bodies work.”
Appropriate Use Criteria and Limitations
Even though nuclear medicine imaging is very helpful, we need to use it wisely. We must think about radiation risks, cost, and if it’s available. It’s important to know when it’s the best choice.
Knowing its strengths and weaknesses helps us use it better. This way, we can give our patients the best care possible.
Advanced and Emerging Diagnostic Imaging Technologies
The world of diagnostic imaging is changing fast. New technologies are coming that will help doctors make better decisions. These new tools are set to change how we see and treat diseases.
Photon-Counting CT and Next-Generation Techniques
Photon-counting CT is a big step forward in CT scans. It can count each photon and measure its energy. This means better pictures, less noise, and more accurate diagnoses. It’s a game-changer for imaging, making diagnoses more accurate and safer for patients.
This tech offers clearer images, spots small problems, and tells different materials apart. As it gets better, it will be key in many areas, like cancer and heart disease.
Artificial Intelligence Integration in Image Interpretation
Artificial intelligence (AI) is changing how we look at images. AI can quickly go through lots of data and spot things we might miss. AI is making diagnoses better, making work easier, and helping patients more.
AI helps by analyzing complex data, finding patterns, and giving exact numbers. As AI gets smarter, it will help doctors make better choices and tailor care to each patient.
Molecular and Functional Imaging Innovations
Molecular and functional imaging are giving us new views of diseases. They let us see and measure biological processes early. We’re leading the way in using these technologies to improve diagnosis and treatment.
New tools in molecular imaging, like special contrast agents, are helping us find and track diseases better. As these technologies grow, we’ll see big improvements in patient care and doctor decisions.
Conclusion: Selecting the Right Imaging Method for Optimal Clinical Outcomes
Choosing the right imaging method is key for the best patient care. Diagnostic imaging includes many ways to see inside the body. Each method has its own strengths and weaknesses.
Medical imaging has changed how we treat patients. It helps find problems early and treat them right. New technologies like artificial intelligence and molecular imaging are coming.
We need to keep up with these new tools. This way, doctors can pick the best imaging for each patient. This leads to better care and helps the field of medical imaging grow.
FAQ
What is diagnostic imaging?
Diagnostic imaging uses technology to see inside the body. It helps doctors make better decisions. We use X-ray, CT, MRI, and more to help patients.
How does diagnostic imaging contribute to disease detection and management?
It helps find and track diseases by showing what’s inside the body. These images guide doctors in treating patients.
What are the different diagnostic imaging modalities?
There are many ways to see inside the body, like X-ray and MRI. Each has its own uses and limits. We pick the best one for each patient.
How does CT scan technology work?
CT scans use X-rays and computers to make detailed images. They’re key in emergencies and for many other tests.
What are the benefits and limitations of MRI?
MRI shows detailed images without harmful radiation. It’s great for many tests but not for everyone. We consider this when choosing MRI.
How is ultrasound used in clinical practice?
Ultrasound is flexible and safe. It’s used right away to help doctors make quick decisions. It’s also portable and affordable.
What is the role of fluoroscopy in procedural guidance?
Fluoroscopy shows moving images in real-time. It helps guide procedures and diagnose issues. It’s essential for many medical tasks.
How does PET scan technology work?
PET scans show how the body works at a molecular level. They help find and track diseases, like cancer. They also check how treatments are working.
What are the emerging trends in diagnostic imaging?
New trends include better CT scans and using artificial intelligence. We keep up with these to improve care and accuracy.
How is diagnostic imaging used in cardiology and endocrinology?
Imaging is key in heart and hormone health. We use it to check the heart and diagnose hormone issues. It helps a lot in these fields.
What is the importance of selecting the right imaging method?
Choosing the right imaging is vital for good care. We think about the patient’s needs and the risks and benefits of each method. This ensures the best care for each patient.
References
- Hussain, S. (2022). Modern Diagnostic Imaging Technique Applications and Advances. PMC, https://pmc.ncbi.nlm.nih.gov/articles/PMC9192206/