Blog
Liv Hospital aspires to lead the way in providing reliable and high-quality healthcare by combining a patient-centered approach, an experienced team of physicians, and the strength of multidisciplinary collaboration. With our commitment to applying advanced diagnostic and treatment methods in step with global standards, our ultimate focus remains clear: your health.
Sort By Letter
 Cancer
CancerWhat are the Three Main Ways that Cancer Can be Treated?
What are the three main ways that cancer can be treated? Every year, millions of people worldwide are diagnosed with ...
 Endocrinology
EndocrinologyKey Sign: Hypothyroidism Dizziness
Are you feeling unexplained fatigue, dizziness, or dry skin? These could be signs of thyroid issues, affecting millio...
 Pediatrics
PediatricsWeak Immune System: The #1 Cause of Dangerous Illness
Respiratory illnesses are a big problem for kids all over the world. Pneumonia is a top cause of death, affecting hun...
 Neurology
NeurologySurgeries Requiring Neuromonitoring: When It’s Most Needed
Millions of people get MRI scans every year. But many don’t know the important steps to prepare. Proper MRI pre...
 Kidney Disease
Kidney DiseaseWhat Is Nephropathy? Understanding Kidney Disease Terms
Understand the medical term "nephropathy" and its impact on kidney health. Learn about the causes, symptoms, and trea...
 Geriatrics
GeriatricsAmnesia Definition: The Essential Meaning
What is the amnesia definition? This essential guide explains the meaning, types, and causes of memory loss. Amnesia ...
 Gastroenterology
GastroenterologyGood Meal Plan for Building Muscle: Best, Simple Guide
Building muscle and losing fat at the same time is now backed by science. Studies show that with resistancetraining ...
 Clinical Neurophysiology
Clinical NeurophysiologyIntraoperative Monitoring: Purpose & Patient Safety
Surgeries on the nervous system are complex and risky for neurological damage. Studies show that intraoperative monit...
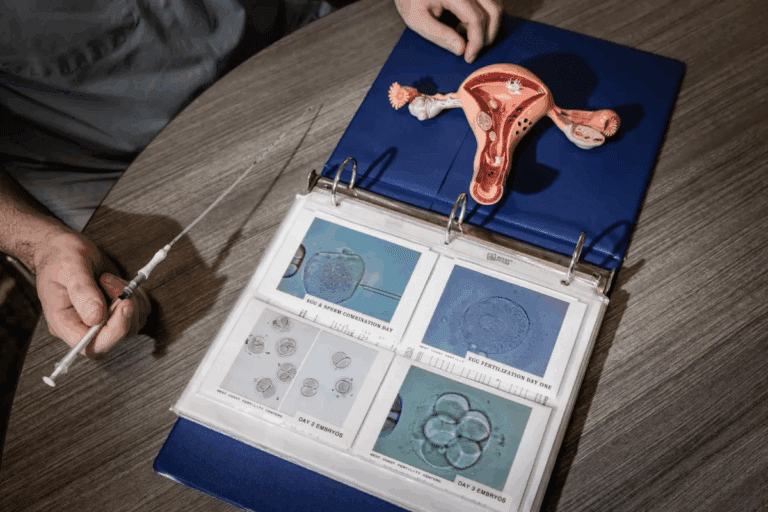 IVF
IVFAnalyzing 5 day fresh embryo transfer success rates vs. Day 3
When thinking about in vitro fertilization (IVF), choosing the right time for embryo transfer is key. The debate is b...
No posts found
Try different filters



